Abstract
Objectives
Improper orthodontic force often causes root resorption or destructive bone resorption. There is evidence that T helper 17 (Th17) cells and regulatory T (Treg) cells may be actively involved in bone remodeling during tooth movement. In a combination of in vitro and in vivo studies, we investigated the effect of human periodontal ligament cells (hPDLCs) on Th17/Treg cells under different orthodontic forces and corticotomy.
Material and methods
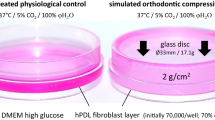
hPDLCs were cultured in vitro and subjected to different mechanical forces. The expression of interleukin (IL)-6 and transforming growth factor (TGF)-β in the supernatant and the mRNA levels of hypoxia inducible factor (HIF)-1α, Notch1, and TGF-β in hPDLCs were investigated. Supernatants were collected and co-cultured with activated CD4+T cells, and the differentiation of Th17/Treg cells was analyzed by flow cytometry. We also established an animal model of tooth movement with or without corticotomy. The tooth movement distance, alveolar bone height, and root resorption were analyzed using micro-computed tomography. Expression of interleukin (IL)-17A, forkhead Box P3 (Foxp3), and IL-6 were analyzed using immunohistochemistry, while osteoclasts were evaluated by tartrate-resistant acid phosphatase (TRAP) staining. The mRNA levels of IL-17A, IL-6, Foxp3, IL-10, HIF-1α, notch1, and C-X-C motif chemokine ligand 12 (CXCL12) in alveolar bone and gingiva were investigated.
Results
Heavy force repressed cell viability and increased the mortality rate of hPDLCs; it also improved the expression of IL-6, declined the expression of TGF-β, and promoted the mRNA expression level of HIF-1α. The expression of TGF-β and Notch1 mRNA decreased and then increased. The supernatant of hPDLCs under heavy force promotes the polarization of Th17 cells. The heavy force caused root resorption and decreased alveolar bone height and increased the positive area of IL-17A immunohistochemical staining and the expression of IL-17A, IL-6, HIF-1α, and Notch1 mRNA. Corticotomy accelerated tooth movement, increased the proportion of Foxp3-positive cells, and up-regulated the expression of Foxp3, IL-10, and CXCL12 mRNA.
Conclusions
During orthodontic tooth movement, the heavy force causes root resorption and inflammatory bone destruction, which could be associated with increased expression of Th17 cells and IL-6. Corticotomy can accelerate tooth movement without causing root resorption and periodontal bone loss, which may be related to the increased expression of Treg cells.
Clinical relevance
Altogether, this report provides a new perspective on the prevention of inflammatory injury via the regulation of Th17/Treg cells in orthodontics.
















Similar content being viewed by others
References
Wise GE, King GJ (2008) Mechanisms of tooth eruption and orthodontic tooth movement. J Dent Res 87(5):414–434. https://doi.org/10.1177/154405910808700509
Gonzales C, Hotokezaka H, Arai Y, Ninomiya T, Tominaga J, Jang I et al (2009) An in vivo 3D micro-CT evaluation of tooth movement after the application of different force magnitudes in rat molar. Angle Orthod 79(4):703–714. https://doi.org/10.2319/071308-366.1
Krishnan V, Davidovitch Z (2006) Cellular, molecular, and tissue-level reactions to orthodontic force. Am J Orthod Dentofacial Orthop 129(4):461–469. https://doi.org/10.1016/j.ajodo.2005.10.007
Ahuja R, Almuzian M, Khan A, Pascovici D, Dalci O, Darendeliler MA (2017) A preliminary investigation of short-term cytokine expression in gingival crevicular fluid secondary to high-level orthodontic forces and the associated root resorption: case series analytical study. Prog Orthod 18(1):23. https://doi.org/10.1186/s40510-017-0177-x
Dandajena TC, Ihnat MA, Disch B, Thorpe J, Currier GF (2012) Hypoxia triggers a HIF-mediated differentiation of peripheral blood mononuclear cells into osteoclasts. Orthod Craniofac Res 15(1):1–9. https://doi.org/10.1111/j.1601-6343.2011.01530.x
Von Bohl M, Maltha J, Von den Hoff H, Kuijpers-Jagtman AM (2004) Changes in the periodontal ligament after experimental tooth movement using high and low continuous forces in beagle dogs. Angle Orthod 74(1):16–25. https://doi.org/10.1043/0003-3219(2004)074%3c0016:CITPLA%3e2.0.CO;2
von Bohl M, Maltha JC, Von Den Hoff JW, Kuijpers-Jagtman AM (2004) Focal hyalinization during experimental tooth movement in beagle dogs. Am J Orthod Dentofacial Orthop 125(5):615–623. https://doi.org/10.1016/j.ajodo.2003.08.023
Li Y, Jacox LA, Little SH, Ko CC (2018) Orthodontic tooth movement: The biology and clinical implications. Kaohsiung J Med Sci 34(4):207–214. https://doi.org/10.1016/j.kjms.2018.01.007
Kraiwattanapong K, Samruajbenjakun B (2018) Effects of different force magnitudes on corticotomy-assisted orthodontic tooth movement in rats. Angle Orthod 88(5):632–637. https://doi.org/10.2319/103117-736.1
Lekic P, McCulloch CA (1996) Periodontal ligament cell population: the central role of fibroblasts in creating a unique tissue. Anat Rec 245(2):327–341. https://doi.org/10.1002/(SICI)1097-0185(199606)245:2%3c327::AID-AR15%3e3.0.CO;2-R
Andrukhov O, Behm C, Blufstein A, Rausch-Fan X (2019) Immunomodulatory properties of dental tissue-derived mesenchymal stem cells: Implication in disease and tissue regeneration. World J Stem Cells 11(9):604–617. https://doi.org/10.4252/wjsc.v11.i9.604
Konermann A, Beyer M, Deschner J, Allam JP, Novak N, Winter J et al (2012) Human periodontal ligament cells facilitate leukocyte recruitment and are influenced in their immunomodulatory function by Th17 cytokine release. Cell Immunol 272(2):137–143. https://doi.org/10.1016/j.cellimm.2011.10.020
Tsukasaki M, Takayanagi H (2019) Osteoimmunology: evolving concepts in bone-immune interactions in health and disease. Nat Rev Immunol 19(10):626–642. https://doi.org/10.1038/s41577-019-0178-8
Roodman GD (2004) Mechanisms of bone metastasis. N Engl J Med 350(16):1655–1664. https://doi.org/10.1056/NEJMra030831
Dar HY, Azam Z, Anupam R, Mondal RK, Srivastava RK (2018) Osteoimmunology: the Nexus between bone and immune system. Front Biosci (Landmark Ed) 23:464–492. https://doi.org/10.2741/4600
Arun KV, Talwar A, Kumar TS (2011) T-helper cells in the etiopathogenesis of periodontal disease: A mini review. J Indian Soc Periodontol 15(1):4–10. https://doi.org/10.4103/0972-124X.82255
Wang L, Wang J, Jin Y, Gao H, Lin X (2014) Oral administration of all-trans retinoic acid suppresses experimental periodontitis by modulating the Th17/Treg imbalance. J Periodontol 85(5):740–750. https://doi.org/10.1902/jop.2013.130132
Tsukasaki M, Komatsu N, Nagashima K, Nitta T, Pluemsakunthai W, Shukunami C et al (2018) Host defense against oral microbiota by bone-damaging T cells. Nat Commun 9(1):701. https://doi.org/10.1038/s41467-018-03147-6
Hayashi N, Yamaguchi M, Nakajima R, Utsunomiya T, Yamamoto H, Kasai K (2012) T-helper 17 cells mediate the osteo/odontoclastogenesis induced by excessive orthodontic forces. Oral Dis 18(4):375–388. https://doi.org/10.1111/j.1601-0825.2011.01886.x
Xie R, Kuijpers-Jagtman AM, Maltha JC (2009) Osteoclast differentiation during experimental tooth movement by a short-term force application: an immunohistochemical study in rats. Acta Odontol Scand 66(5):314–320. https://doi.org/10.1080/00016350802317488
Wang J, Jiao D, Huang X, Bai Y (2021) Osteoclastic effects of mBMMSCs under compressive pressure during orthodontic tooth movement. Stem Cell Res Ther 12(1):148. https://doi.org/10.1186/s13287-021-02220-0
Castro-Manrreza ME, Montesinos JJ (2015) Immunoregulation by mesenchymal stem cells: biological aspects and clinical applications. J Immunol Res 2015:394917. https://doi.org/10.1155/2015/394917
Liu D, Xu J, Liu O, Fan Z, Liu Y, Wang F et al (2012) Mesenchymal stem cells derived from inflamed periodontal ligaments exhibit impaired immunomodulation. J Clin Periodontol 39(12):1174–1182. https://doi.org/10.1111/jcpe.12009
Kanzaki H, Chiba M, Shimizu Y, Mitani H (2002) Periodontal ligament cells under mechanical stress induce osteoclastogenesis by receptor activator of nuclear factor kappaB ligand up-regulation via prostaglandin E2 synthesis. J Bone Miner Res 17(2):210–220. https://doi.org/10.1359/jbmr.2002.17.2.210
Kook S, Jang Y, Lee J (2011) Human periodontal ligament fibroblasts stimulate osteoclastogenesis in response to compression force through TNF-α-mediated activation of CD4+ T cells. J Cell Biochem 112(10):2891–2901. https://doi.org/10.1002/jcb.23205
Sun K, Luo J, Jing X, Xiang W, Guo J, Yao X et al (2021) Hyperoside ameliorates the progression of osteoarthritis: An in vitro and in vivo study. Phytomedicine 80:153387. https://doi.org/10.1016/j.phymed.2020.153387
Lancioni CL, Thomas JJ, Rojas RE (2009) Activation requirements and responses to TLR ligands in human CD4+ T cells: comparison of two T cell isolation techniques. J Immunol Methods 344(1):15–25. https://doi.org/10.1016/j.jim.2009.02.005
Ahmadi M, Yousefi M, Abbaspour-Aghdam S, Dolati S, Aghebati-Maleki L, Eghbal-Fard S et al (2019) Disturbed Th17/Treg balance, cytokines, and miRNAs in peripheral blood of patients with Behcet’s disease. J Cell Physiol 234(4):3985–3994. https://doi.org/10.1002/jcp.27207
Kirschneck C, Bauer M, Gubernator J, Proff P, Schroder A (2020) Comparative assessment of mouse models for experimental orthodontic tooth movement. Sci Rep 10(1):12154. https://doi.org/10.1038/s41598-020-69030-x
Wang Y, Zhang H, Sun W, Wang S, Zhang S, Zhu L et al (2018) Macrophages mediate corticotomy-accelerated orthodontic tooth movement. Sci Rep 8(1):16788. https://doi.org/10.1038/s41598-018-34907-5
Li C, Li B, Dong Z, Gao L, He X, Liao L et al (2014) Lipopolysaccharide differentially affects the osteogenic differentiation of periodontal ligament stem cells and bone marrow mesenchymal stem cells through Toll-like receptor 4 mediated nuclear factor kappaB pathway. Stem Cell Res Ther 5(3):67. https://doi.org/10.1186/scrt456
He D, Kou X, Luo Q, Yang R, Liu D, Wang X et al (2015) Enhanced M1/M2 macrophage ratio promotes orthodontic root resorption. J Dent Res 94(1):129–139. https://doi.org/10.1177/0022034514553817
Liao W, Okada M, Inami K, Hashimoto Y, Matsumoto N (2016) Cell survival and gene expression under compressive stress in a three-dimensional in vitro human periodontal ligament-like tissue model. Cytotechnology 68(2):249–260. https://doi.org/10.1007/s10616-014-9775-3
Yamaguchi M, Ozawa Y, Nogimura A, Aihara N, Kojima T, Hirayama Y et al (2004) Cathepsins B and L increased during response of periodontal ligament cells to mechanical stress in vitro. Connect Tissue Res 45(3):181–189. https://doi.org/10.1080/03008200490514149
Schroder A, Kuchler EC, Omori M, Spanier G, Proff P, Kirschneck C (2019) Effects of ethanol on human periodontal ligament fibroblasts subjected to static compressive force. Alcohol 77:59–70. https://doi.org/10.1016/j.alcohol.2018.10.004
Ullrich N, Schroder A, Jantsch J, Spanier G, Proff P, Kirschneck C (2019) The role of mechanotransduction versus hypoxia during simulated orthodontic compressive strain-an in vitro study of human periodontal ligament fibroblasts. Int J Oral Sci 11(4):33. https://doi.org/10.1038/s41368-019-0066-x
Hu Q, Zhou J, Xu X, Dai H (2018) Effect of EMD on the orthodontically induced root resorption repair process in rats. J Orofac Orthop 79(2):83–95. https://doi.org/10.1007/s00056-017-0119-8
Nakano T, Hotokezaka H, Hashimoto M, Sirisoontorn I, Arita K, Kurohama T et al (2014) Effects of different types of tooth movement and force magnitudes on the amount of tooth movement and root resorption in rats. Angle Orthod 84(6):1079–1085. https://doi.org/10.2319/121913-929.1
Crane JL, Xian L, Cao X (2016) Role of TGF-beta Signaling in coupling bone remodeling. Methods Mol Biol 1344:287–300. https://doi.org/10.1007/978-1-4939-2966-5_18
Karst M, Gorny G, Galvin RJ, Oursler MJ (2004) Roles of stromal cell RANKL, OPG, and M-CSF expression in biphasic TGF-beta regulation of osteoclast differentiation. J Cell Physiol 200(1):99–106. https://doi.org/10.1002/jcp.20036
Mucida D, Park Y, Kim G, Turovskaya O, Scott I, Kronenberg M et al (2007) Reciprocal TH17 and regulatory T cell differentiation mediated by retinoic acid. Science 317(5835):256–260. https://doi.org/10.1126/science.1145697
Corcoran SE, O’Neill LA (2016) HIF1alpha and metabolic reprogramming in inflammation. J Clin Invest 126(10):3699–3707. https://doi.org/10.1172/JCI84431
Hienz SA, Paliwal S, Ivanovski S (2015) Mechanisms of bone resorption in periodontitis. J Immunol Res 2015:615486. https://doi.org/10.1155/2015/615486
Ebersole JL, Kirakodu S, Novak MJ, Stromberg AJ, Shen S, Orraca L et al (2014) Cytokine gene expression profiles during initiation, progression and resolution of periodontitis. J Clin Periodontol 41(9):853–861. https://doi.org/10.1111/jcpe.12286
Dutzan N, Konkel JE, Greenwell-Wild T, Moutsopoulos NM (2016) Characterization of the human immune cell network at the gingival barrier. Mucosal Immunol 9(5):1163–1172. https://doi.org/10.1038/mi.2015.136
Zenobia C (2000) Hajishengallis G (2015) Basic biology and role of interleukin-17 in immunity and inflammation. Periodontol 69(1):142–159. https://doi.org/10.1111/prd.12083
Alvarez C, Rojas C, Rojas L, Cafferata EA, Monasterio G, Vernal R (2018) Regulatory T lymphocytes in periodontitis: a translational view. Mediators Inflamm 2018:7806912. https://doi.org/10.1155/2018/7806912
Wang L, Guan N, Jin Y, Lin X, Gao H (2015) Subcutaneous vaccination with Porphyromonas gingivalis ameliorates periodontitis by modulating Th17/Treg imbalance in a murine model. Int Immunopharmacol 25(1):65–73. https://doi.org/10.1016/j.intimp.2015.01.007
Yamaguchi M, Fukasawa S (2021) Is inflammation a friend or foe for orthodontic treatment?: Inflammation in orthodontically induced inflammatory root resorption and accelerating tooth movement. Int J Mol Sci 22(5):2388. https://doi.org/10.3390/ijms22052388
Feller L, Khammissa R, Siebold A, Hugo A, Lemmer J (2019) Biological events related to corticotomy-facilitated orthodontics. J Int Med Res 47(7):2856–2864. https://doi.org/10.1177/0300060519856456
Du L, Lin L, Li Q, Liu K, Huang Y, Wang X et al (2019) IGF-2 preprograms maturing macrophages to acquire oxidative phosphorylation-dependent anti-inflammatory properties. Cell Metab 29(6):1363–1375. https://doi.org/10.1016/j.cmet.2019.01.006
Wing K, Yamaguchi T, Sakaguchi S (2011) Cell-autonomous and -non-autonomous roles of CTLA-4 in immune regulation. Trends Immunol 32(9):428–433. https://doi.org/10.1016/j.it.2011.06.002
Luo CY, Wang L, Sun C, Li DJ (2011) Estrogen enhances the functions of CD4(+)CD25(+)Foxp3(+) regulatory T cells that suppress osteoclast differentiation and bone resorption in vitro. Cell Mol Immunol 8(1):50–58. https://doi.org/10.1038/cmi.2010.54
Strazza M, Mor A (2017) Consider the chemokines: a review of the interplay between chemokines and T cell subset function. Discov Med 24(130):31–39
Vanoni G, Ercolano G, Candiani S, Rutigliani M, Lanata M, Derré L et al (2021) Human primed ILCPs support endothelial activation through NF-κB signaling. eLife 10 e58838. https://doi.org/10.7554/eLife.58838
Dyson MR, Masters E, Pazeraitis D, Perera RL, Syrjanen JL, Surade S et al (2020) Beyond affinity: selection of antibody variants with optimal biophysical properties and reduced immunogenicity from mammalian display libraries. mAbs 12(1):1829335. https://doi.org/10.1080/19420862.2020.1829335
Alissafi T, Kalafati L, Lazari M, Filia A, Kloukina I, Manifava M et al (2020) Mitochondrial oxidative damage underlies regulatory T cell defects in autoimmunity. Cell Metab 32(4):591–604. https://doi.org/10.1016/j.cmet.2020.07.001
Bailur JK, McCachren SS, Pendleton K, Vasquez JC, Lim HS, Duffy A et al (2020) Risk-associated alterations in marrow T cells in pediatric leukemia. JCI Insight 5(16):e140179. https://doi.org/10.1172/jci.insight.140179
Schwarz A, Philippsen R, Schwarz T (2021) Induction of regulatory T cells and correction of cytokine disbalance by short-chain fatty acids: implications for psoriasis therapy. J Investig Dermatol 141(1):95–104. https://doi.org/10.1016/j.jid.2020.04.031
Gao L, Dou J, Zhang B, Zeng J, Cheng Q, Lei L et al (2020) Ozone therapy promotes the differentiation of basal keratinocytes via increasing Tp63-mediated transcription of KRT10 to improve psoriasis. J Cell Mol Med 24(8):4819–4829. https://doi.org/10.1111/jcmm.15160
Chen S, Tang Y, Yang C, Li K, Huang X, Cao J (2020) Silencing CDC25A inhibits the proliferation of liver cancer cells by downregulating IL6 in vitro and in vivo. Int J Mol Med 45(3):743–752. https://doi.org/10.3892/ijmm.2020.4461
Acknowledgements
The authors would like to thank Professor Sha Wu (Southern Medical University) for the helpful discussion and technical support.
Funding
This work was financially supported by the Natural Science Foundation of Guangdong Province, China (No. 2018A0303130261). Natural science foundation of guangdong province,No. 2018A0303130261,Chufeng Liu
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The in vitro portion of the study was approved by the Ethical Committee of Southern Medical University and with the informed consent of all the volunteers. All protocols for animal experiments were approved by the Animal Ethics Committee of Zhujiang Hospital of Southern Medical University (LAEC-2020–193).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lin, J., Huang, J., Zhang, Z. et al. Periodontal ligament cells under mechanical force regulate local immune homeostasis by modulating Th17/Treg cell differentiation. Clin Oral Invest 26, 3747–3764 (2022). https://doi.org/10.1007/s00784-021-04346-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-021-04346-0