Abstract
Study design
Retrospective cohort.
Background
Over 44 million adults are estimated to have either osteoporosis or osteopenia. Adult spinal deformity (ASD) is estimated to affect between 32 and 68% of the elderly population.
Objective
Retrospective investigation comparing rates of postoperative complications following thoracolumbar scoliosis surgery in patients with normal bone mineral density (BMD) to those with osteopenia or osteoporosis in addition to analyzing the effects of pretreatment with anti-osteoporotic medications in patients with low BMD.
Methods
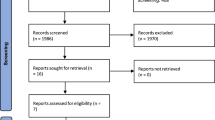
Using administrative database of Humana beneficiaries, ICD-9 and ICD-10 diagnosis codes were used to identify ASD patients undergoing multilevel thoracolumbar fusions between 2007 and 2017.
Results
The propensity matched population analyzed in this study contained 1044 patients equally represented by those with a history of osteopenia, osteoporosis, or normal BMD. Osteopenia and osteoporosis were associated with increased odds of revision surgery (OR 2.01 95% CI 1.36–2.96 and OR 1.57, 95% CI 1.05–2.35), respectively. Similarly, there was an almost twofold increased odds of proximal and distal junctional kyphosis in patients with osteopenia and osteoporosis (OR 1.95, 95% CI 1.40–2.74 and OR 1.88, 95% CI 1.34–2.64), respectively. A total of 258 (37.1%) patients with osteoporosis were pretreated with anti-osteoporotic medications and there was no statistically significant decrease in odds of proximal or distal junctional kyphosis or revision surgery in these patients.
Conclusion
Patients with ASD undergoing multilevel thoracolumbar fusion surgery have significantly higher rates of postoperative pseudarthrosis, proximal and distal junctional kyphosis, and revision surgery rates compared to patients with normal BMD.




Similar content being viewed by others
References
Amin RM, Raad M, Jain A et al (2019) Risk factors for nonroutine discharge in adult spinal deformity surgery. Spine J Off J North Am Spine Soc 19(2):357–363. https://doi.org/10.1016/j.spinee.2018.06.366
Barber JW, Boden SD, Ganey T, Hutton WC (1998) Biomechanical study of lumbar pedicle screws: does convergence affect axial pullout strength? J Spinal Disord 11(3):215–220
Buerba RA, Sharma A, Ziino C, Arzeno A, Ajiboye RM (2018) Bisphosphonate and teriparatide use in thoracolumbar spinal fusion: a systematic review and meta-analysis of comparative studies. Spine 43(17):E1014–E1023. https://doi.org/10.1097/BRS.0000000000002608
Carmouche JJ, Molinari RW, Gerlinger T, Devine J, Patience T (2005) Effects of pilot hole preparation technique on pedicle screw fixation in different regions of the osteoporotic thoracic and lumbar spine. J Neurosurg Spine 3(5):364–370. https://doi.org/10.3171/spi.2005.3.5.0364
Chen F, Dai Z, Kang Y, Lv G, Keller ET, Jiang Y (2016) Effects of zoledronic acid on bone fusion in osteoporotic patients after lumbar fusion. Osteoporos Int J Establ Result Coop Eur Found Osteoporos Natl Osteoporos Found USA 27(4):1469–1476. https://doi.org/10.1007/s00198-015-3398-1
Deyo RA, Gray DT, Kreuter W, Mirza S, Martin BI (2005) United States trends in lumbar fusion surgery for degenerative conditions. Spine. 30(12):1441–1445. https://doi.org/10.1097/01.brs.0000166503.37969.8a
Díaz-Romero Paz R, Sosa Henríquez M, ArmasMelián K, Coloma VG (2019) Trends and attitudes of spine surgeons regarding osteoporosis. Neurocir Astur Spain 30(6):268–277. https://doi.org/10.1016/j.neucir.2019.04.004
Diebo BG, Shah NV, Boachie-Adjei O et al (2019) Adult spinal deformity. Lancet Lond Engl 394(10193):160–172. https://doi.org/10.1016/S0140-6736(19)31125-0
Dipaola CP, Bible JE, Biswas D, Dipaola M, Grauer JN, Rechtine GR (2009) Survey of spine surgeons on attitudes regarding osteoporosis and osteomalacia screening and treatment for fractures, fusion surgery, and pseudoarthrosis. Spine J Off J North Am Spine Soc 9(7):537–544. https://doi.org/10.1016/j.spinee.2009.02.005
Fehlings MG, Tetreault L, Nater A et al (2015) The aging of the global population: the changing epidemiology of disease and spinal disorders. Neurosurgery 77(Suppl 4):S1-5. https://doi.org/10.1227/NEU.0000000000000953
Gupta A, Upadhyaya S, Patel A et al (2020) DEXA sensitivity analysis in patients with adult spinal deformity. Spine J Off J North Am Spine Soc 20(2):174–180. https://doi.org/10.1016/j.spinee.2019.08.011
Hackenberg L, Link T, Liljenqvist U (2002) Axial and tangential fixation strength of pedicle screws versus hooks in the thoracic spine in relation to bone mineral density. Spine 27(9):937–942. https://doi.org/10.1097/00007632-200205010-00010
Hadjipavlou AG, Nicodemus CL, al-Hamdan FA, Simmons JW, Pope MH. (1997) Correlation of bone equivalent mineral density to pull-out resistance of triangulated pedicle screw construct. J Spinal Disord. 10(1):12–19
Halvorson TL, Kelley LA, Thomas KA, Whitecloud TS, Cook SD (1994) Effects of bone mineral density on pedicle screw fixation. Spine 19(21):2415–2420. https://doi.org/10.1097/00007632-199411000-00008
Huang RC, Khan SN, Sandhu HS et al (2005) Alendronate inhibits spine fusion in a rat model. Spine 30(22):2516–2522. https://doi.org/10.1097/01.brs.0000186470.28070.7b
Jung A, Bisaz S, Fleisch H (1973) The binding of pyrophosphate and two diphosphonates by hydroxyapatite crystals. Calcif Tissue Res 11(4):269–280. https://doi.org/10.1007/BF02547227
Khosla S, Melton LJ (2007) Clinical practice. Osteopenia N Engl J Med 356(22):2293–2300. https://doi.org/10.1056/NEJMcp070341
Kim HJ, Iyer S (2016) Proximal junctional kyphosis. J Am Acad Orthop Surg 24(5):318–326. https://doi.org/10.5435/JAAOS-D-14-00393
Kim HJ, Yagi M, Nyugen J, Cunningham ME, Boachie-Adjei O (2012) Combined anterior-posterior surgery is the most important risk factor for developing proximal junctional kyphosis in idiopathic scoliosis. Clin Orthop 470(6):1633–1639. https://doi.org/10.1007/s11999-011-2179-1
Kim JS, Phan K, Cheung ZB et al (2019) Surgical, radiographic, and patient-related risk factors for proximal junctional kyphosis: a meta-analysis. Glob Spine J 9(1):32–40. https://doi.org/10.1177/2192568218761362
Kumano K, Hirabayashi S, Ogawa Y, Aota Y (1994) Pedicle screws and bone mineral density. Spine 19(10):1157–1161. https://doi.org/10.1097/00007632-199405001-00012
Lehman RA, Kuklo TR, Freedman BA, Cowart JR, Mense MG, Riew KD (2004) The effect of alendronate sodium on spinal fusion: a rabbit model. Spine J Off J North Am Spine Soc 4(1):36–43. https://doi.org/10.1016/s1529-9430(03)00427-3
Margulies JY, Payzer A, Nyska M, Neuwirth MG, Floman Y, Robin GC (1996) The relationship between degenerative changes and osteoporosis in the lumbar spine. Clin Orthop 324:145–152. https://doi.org/10.1097/00003086-199603000-00017
McDonald MM, Dulai S, Godfrey C, Amanat N, Sztynda T, Little DG (2008) Bolus or weekly zoledronic acid administration does not delay endochondral fracture repair but weekly dosing enhances delays in hard callus remodeling. Bone 43(4):653–662. https://doi.org/10.1016/j.bone.2008.05.019
Miller PD (2008) Anti-resorptives in the management of osteoporosis. Best Pract Res Clin Endocrinol Metab 22(5):849–868. https://doi.org/10.1016/j.beem.2008.07.004
Miller PD, Watts NB, Licata AA et al (1997) Cyclical etidronate in the treatment of postmenopausal osteoporosis: efficacy and safety after seven years of treatment. Am J Med 103(6):468–476. https://doi.org/10.1016/s0002-9343(97)00278-7
Morris CD, Einhorn TA (2005) Bisphosphonates in orthopaedic surgery. J Bone Joint Surg Am 87(7):1609–1618. https://doi.org/10.2106/JBJS.D.03032
Nagahama K, Kanayama M, Togawa D, Hashimoto T, Minami A (2011) Does alendronate disturb the healing process of posterior lumbar interbody fusion? A prospective randomized trial. J Neurosurg Spine 14(4):500–507. https://doi.org/10.3171/2010.11.SPINE10245
Nakao S, Minamide A, Kawakami M, Boden SD, Yoshida M (2011) The influence of alendronate on spine fusion in an osteoporotic animal model. Spine 36(18):1446–1452. https://doi.org/10.1097/BRS.0b013e3181f49c47
Okuyama K, Abe E, Suzuki T, Tamura Y, Chiba M, Sato K (2001) Influence of bone mineral density on pedicle screw fixation: a study of pedicle screw fixation augmenting posterior lumbar interbody fusion in elderly patients. Spine J Off J North Am Spine Soc 1(6):402–407. https://doi.org/10.1016/s1529-9430(01)00078-x
Rajaee SS, Bae HW, Kanim LEA, Delamarter RB (2012) Spinal fusion in the United States: analysis of trends from 1998 to 2008. Spine 37(1):67–76. https://doi.org/10.1097/BRS.0b013e31820cccfb
Rodan GA, Fleisch HA (1996) Bisphosphonates: mechanisms of action. J Clin Invest 97(12):2692–2696. https://doi.org/10.1172/JCI118722
Schimmer RC, Bauss F (2003) Effect of daily and intermittent use of ibandronate on bone mass and bone turnover in postmenopausal osteoporosis: a review of three phase II studies. Clin Ther 25(1):19–34. https://doi.org/10.1016/s0149-2918(03)90005-1
Schreiber JJ, Hughes AP, Taher F, Girardi FP (2014) An association can be found between Hounsfield units and success of lumbar spine fusion. HSS J 10(1):25–29. https://doi.org/10.1007/s11420-013-9367-3
Seki S, Hirano N, Kawaguchi Y et al (2017) Teriparatide versus low-dose bisphosphonates before and after surgery for adult spinal deformity in female Japanese patients with osteoporosis. Eur Spine J 26(8):2121–2127. https://doi.org/10.1007/s00586-017-4959-0
Sheu H, Liao J-C, Lin Y-C (2019) The fate of thoracolumbar surgeries in patients with Parkinson’s disease, and analysis of risk factors for revision surgeries. BMC Musculoskelet Disord 20(1):106. https://doi.org/10.1186/s12891-019-2481-8
Soshi S, Shiba R, Kondo H, Murota K (1991) An experimental study on transpedicular screw fixation in relation to osteoporosis of the lumbar spine. Spine 16(11):1335–1341. https://doi.org/10.1097/00007632-199111000-00015
Tonino RP, Meunier PJ, Emkey R et al (2000) Skeletal benefits of alendronate: 7-year treatment of postmenopausal osteoporotic women Phase III Osteoporosis Treatment Study Group. J Clin Endocrinol Metab. 85(9):3109–3115. https://doi.org/10.1210/jcem.85.9.6777
Tu C-W, Huang K-F, Hsu H-T, Li H-Y, Yang SS-D, Chen Y-C (2014) Zoledronic acid infusion for lumbar interbody fusion in osteoporosis. J Surg Res. 192(1):112–116. https://doi.org/10.1016/j.jss.2014.05.034
Watanabe K, Lenke LG, Bridwell KH, Kim YJ, Koester L, Hensley M (2010) Proximal junctional vertebral fracture in adults after spinal deformity surgery using pedicle screw constructs. Spine 35(2):138–145. https://doi.org/10.1097/BRS.0b013e3181c8f35d
Wright NC, Looker AC, Saag KG et al (2014) The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine. J Bone Miner Res Off J Am Soc Bone Miner Res 29(11):2520–2526. https://doi.org/10.1002/jbmr.2269
Zou D, Li W, Deng C, Du G, Xu N (2019) The use of CT Hounsfield unit values to identify the undiagnosed spinal osteoporosis in patients with lumbar degenerative diseases. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 28(8):1758–1766. https://doi.org/10.1007/s00586-018-5776-9
Zhao J, Chen K, Zhai X, Chen K, Li M, Lu Y. Incidence and risk factors of proximal junctional kyphosis after internal fixation for adult spinal deformity: a systematic evaluation and meta-analysis. Neurosurg Rev. Published online May 19, 2020. doi:https://doi.org/10.1007/s10143-020-01309-z
DeWald CJ, Stanley T (2006) Instrumentation-related complications of multilevel fusions for adult spinal deformity patients over age 65: surgical considerations and treatment options in patients with poor bone quality. Vol 31. doi:https://doi.org/10.1097/01.brs.0000236893.65878.39
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The present study was evaluated by our institution’s IRB and was deemed to be except from IRB approval.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Spine degenerative
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Khalid, S.I., Nunna, R.S., Smith, J.S. et al. The role of bone mineral density in adult spinal deformity patients undergoing corrective surgery: a matched analysis. Acta Neurochir 164, 2327–2335 (2022). https://doi.org/10.1007/s00701-022-05317-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-022-05317-4