Abstract
Background
Aneurysmal subarachnoid hemorrhage (aSAH) patients admitted to primary stroke centers are often transferred to neurosurgical and endovascular services at tertiary centers. The effect on microsurgical outcomes of the resultant delay in treatment is unknown. We evaluated microsurgical aSAH treatment > 72 h after the ictus.
Methods
All aSAH patients treated at a single tertiary center between August 1, 2007, and July 31, 2019, were retrospectively reviewed. The additional inclusion criterion was the availability of treatment data relative to time of bleed. Patients were grouped based on bleed-to-treatment time as having acute treatment (on or before postbleed day [PBD] 3) or delayed treatment (on or after PBD 4). Propensity adjustments were used to correct for statistically significant confounding covariables.
Results
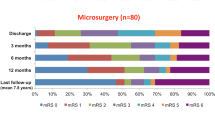
Among 956 aSAH patients, 92 (10%) received delayed surgical treatment (delayed group), and 864 (90%) received acute endovascular or surgical treatment (acute group). Reruptures occurred in 3% (26/864) of the acute group and 1% (1/92) of the delayed group (p = 0.51). After propensity adjustments, the odds of residual aneurysm (OR = 0.09; 95% CI = 0.04–0.17; p < 0.001) or retreatment (OR = 0.14; 95% CI = 0.06–0.29; p < 0.001) was significantly lower among the delayed group. The OR was 0.50 for rerupture, after propensity adjustments, in the delayed setting (p = 0.03). Mean Glasgow Coma Scale scores at admission in the acute and delayed groups were 11.5 and 13.2, respectively (p < 0.001).
Conclusions
Delayed microsurgical management of aSAH, if required for definitive treatment, appeared to be noninferior with respect to retreatment, residual, and rerupture events in our cohort after adjusting for initial disease severity and significant confounding variables.

Similar content being viewed by others
Abbreviations
- aSAH:
-
Aneurysmal subarachnoid hemorrhage
- CI:
-
Confidence interval
- CSC:
-
Comprehensive stroke center
- GCS:
-
Glasgow Coma Scale
- mRS:
-
Modified Rankin Scale
- OR:
-
Odds ratio
- PBD:
-
Postbleed day
- SD:
-
Standard deviation
References
An H, Park J, Kang DH, Son W, Lee YS, Kwak Y, Ohk B (2019) Should cerebral angiography be avoided within three hours after subarachnoid hemorrhage? J Korean Neurosurg Soc 62:526–535
Berman MF, Solomon RA, Mayer SA, Johnston SC, Yung PP (2003) Impact of hospital-related factors on outcome after treatment of cerebral aneurysms. Stroke 34:2200–2207
Burkhardt JK, Lawton MT (2019) Practice trends in intracranial bypass surgery in a 21-year experience. World Neurosurg 125:e717–e722
Buscot MJ, Chandra RV, Maingard J, Nichols L, Blizzard L, Stirling C, Smith K, Lai L, Asadi H, Froelich J, Reeves MJ, Thani N, Thrift A, Gall S (2022) Association of onset-to-treatment time with discharge destination, mortality, and complications among patients with aneurysmal subarachnoid hemorrhage. JAMA Netw Open 5:e2144039. https://doi.org/10.1001/jamanetworkopen.2021.44039
Catalano AR, Winn HR, Gordon E, Frontera JA (2012) Impact of interhospital transfer on complications and outcome after intracranial hemorrhage. Neurocrit Care 17:324–333
Catapano JS, Srinivasan VM, Labib MA, Rumalla K, Nguyen CL, Rahmani R, Baranoski JF, Cole TS, Rutledge C, Jadhav AP, Ducruet AF, Albuquerque FC, Zabramski JM, Lawton MT (2022) The times they are a-changin’: increasing complexity of aneurysmal subarachnoid hemorrhages in patients treated from 2004 to 2018. World Neurosurg 161:e168–e173
Catapano JS, Srinivasan VM, Rumalla K, Labib MA, Nguyen CL, Cole TS, Baranoski JF, Rutledge C, Rahmani R, Lawton MT, Ducruet AF, Albuquerque FC (2022) Length of hospital stay in aneurysmal subarachnoid hemorrhage patients without vasospasm on angiography: potential for a fast-track discharge cohort. J Neurointerv Surg 14:376–379
Connolly ES Jr, Rabinstein AA, Carhuapoma JR, Derdeyn CP, Dion J, Higashida RT, Hoh BL, Kirkness CJ, Naidech AM, Ogilvy CS, Patel AB, Thompson BG, Vespa P (2012) Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 43:1711–1737
Crowley RW, Yeoh HK, Stukenborg GJ, Ionescu AA, Kassell NF, Dumont AS (2009) Influence of weekend versus weekday hospital admission on mortality following subarachnoid hemorrhage. Clinical article. J Neurosurg 111:60–66
Deshmukh H, Hinkley M, Dulhanty L, Patel HC, Galea JP (2016) Effect of weekend admission on in-hospital mortality and functional outcomes for patients with acute subarachnoid haemorrhage (SAH). Acta Neurochir (Wien) 158:829–835
Gittins A, Talbott N, Gilani AA, Packer G, Browne R, Mullhi R, Khan Z, Whitehouse T, Belli A, Mehta RL, Gao-Smith F, Veenith T (2021) Outcomes following acute poor-grade aneurysmal subarachnoid bleed—is early definitive treatment better than delayed management? J Intensive Care Soc 22:198–203
Goertz L, Kabbasch C, Pflaeging M, Pennig L, Laukamp KR, Timmer M, Styczen H, Brinker G, Goldbrunner R, Krischek B (2021) Impact of the weekend effect on outcome after microsurgical clipping of ruptured intracranial aneurysms. Acta Neurochir (Wien) 163:783–791
Hillman J, Fridriksson S, Nilsson O, Yu Z, Saveland H, Jakobsson KE (2002) Immediate administration of tranexamic acid and reduced incidence of early rebleeding after aneurysmal subarachnoid hemorrhage: a prospective randomized study. J Neurosurg 97:771–778
Hopkins LN, Holmes DR Jr (2017) Public health urgency created by the success of mechanical thrombectomy studies in stroke. Circulation 135:1188–1190
Johnson WC, Morton-Gonzaba NA, Lacci JV, Godoy D, Mirahmadizadeh A, Seifi A (2019) Re-evaluating the weekend effect on SAH: a nationwide analysis of the association between mortality and weekend admission. Neurocrit Care 30:293–300
Kassell NF, Boarini DJ, Adams HP Jr, Sahs AL, Graf CJ, Torner JC, Gerk MK (1981) Overall management of ruptured aneurysm: comparison of early and late operation. Neurosurgery 9:120–128
Kassell NF, Torner JC (1983) Aneurysmal rebleeding: a preliminary report from the Cooperative Aneurysm Study. Neurosurgery 13:479–481
Kawahara I, Matsunaga Y, Tsutsumi K, Takahata H, Ono T, Toda K, Baba H (2014) Timing of helicopter transportation for patients presenting with subarachnoid hemorrhage on isolated islands. No Shinkei Geka 42:537–543
Kim T, Jwa C (2021) Impact of off-hour hospital presentation on mortality in different subtypes of acute stroke in Korea: National Emergency Department Information System Data. J Korean Neurosurg Soc 64:51–59
Kurogi R, Kada A, Ogasawara K, Kitazono T, Sakai N, Hashimoto Y, Shiokawa Y, Miyachi S, Matsumaru Y, Iwama T, Tominaga T, Onozuka D, Nishimura A, Arimura K, Kurogi A, Ren N, Hagihara A, Nakaoku Y, Arai H, Miyamoto S, Nishimura K, Iihara K (2020) Effects of case volume and comprehensive stroke center capabilities on patient outcomes of clipping and coiling for subarachnoid hemorrhage. J Neurosurg 134:929–939
Kusumi M, Yamada M, Kitahara T, Endo M, Kan S, Iida H, Sagiuchi T, Fujii K (2005) Rerupture of cerebral aneurysms during angiography—a retrospective study of 13 patients with subarachnoid hemorrhage. Acta Neurochir (Wien) 147:831–837
Mikhail M, Ayling OGS, Eagles ME, Ibrahim GM, Macdonald RL (2019) Association between weekend admissions and mortality after aneurysmal subarachnoid hemorrhage: the “weekend effect” revisited. J Neurosurg 132:1167–1173
Nichols L, Stirling C, Stankovich J, Gall S (2020) Time to treatment following an aneurysmal subarachnoid hemorrhage, rural place of residence and inter-hospital transfers. Australas Emerg Care 23:225–232
Ohman J, Heiskanen O (1989) Timing of operation for ruptured supratentorial aneurysms: a prospective randomized study. J Neurosurg 70:55–60
Pandey AS, Gemmete JJ, Wilson TJ, Chaudhary N, Thompson BG, Morgenstern LB, Burke JF (2015) High subarachnoid hemorrhage patient volume associated with lower mortality and better outcomes. Neurosurgery 77:462–470; discussion 470
Phillips TJ, Dowling RJ, Yan B, Laidlaw JD, Mitchell PJ (2011) Does treatment of ruptured intracranial aneurysms within 24 hours improve clinical outcome? Stroke 42:1936–1945
Sanai N, Caldwell N, Englot DJ, Lawton MT (2012) Advanced technical skills are required for microsurgical clipping of posterior communicating artery aneurysms in the endovascular era. Neurosurgery 71:285–294; discussion 294–285
Solomon RA, Mayer SA, Tarmey JJ (1996) Relationship between the volume of craniotomies for cerebral aneurysm performed at New York state hospitals and in-hospital mortality. Stroke 27:13–17
Spetzler RF, McDougall CG, Zabramski JM, Albuquerque FC, Hills NK, Russin JJ, Partovi S, Nakaji P, Wallace RC (2015) The Barrow Ruptured Aneurysm Trial: 6-year results. J Neurosurg 123:609–617
Tayebi Meybodi A, Gadhyia A, Borba Moreira L, Lawton MT (2021) Coding cerebral bypasses: a proposed nomenclature to better describe bypass constructs and revascularization techniques. J Neurosurg 136:163–174
Acknowledgements
We thank the staff of Neuroscience Publications at Barrow Neurological Institute for assistance with manuscript preparation.
Funding
No funding was received for this research.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Stefan W. Koester and Candice L. Nguyen. The first draft of the manuscript was written by Stefan W. Koester and Visish M. Srinivasan and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This retrospective study was approved by the Institutional Review Board and St. Joseph’s Hospital and Medical Center in Phoenix, Arizona.
Informed consent
Informed consent was waived due to the low risk to patients in this IRB-approved, retrospective study.
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Vascular Neurosurgery – Aneurysm
Rights and permissions
About this article
Cite this article
Srinivasan, V.M., Koester, S.W., Karahalios, K. et al. Microsurgical treatment of ruptured aneurysms beyond 72 hours after rupture: implications for advanced management. Acta Neurochir 164, 2431–2439 (2022). https://doi.org/10.1007/s00701-022-05283-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-022-05283-x