Abstract
Objective
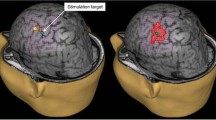
Navigated transcranial magnetic stimulation (nTMS) has been increasingly used for presurgical cortical mapping of the primary motor cortex (M1) but remains controversial for the evaluation of non-primary motor areas (NPMA). This study investigates clinical and neurophysiological parameters in brain tumour patients and healthy volunteers to decide whether single-pulse biphasic nTMS allows to reliably elicite MEP outside from M1 or not.
Materials and methods
Twelve brain tumour patients and six healthy volunteers underwent M1 nTMS mapping. NPMA nTMS mapping followed using 120% and 150% M1 resting motor threshold (RMT) stimulation intensity. Spearman’s correlation analysis tested the association of clinical and neurophysiological parameters between M1 and NPMA mapping.
Results
A total of 88.81% of nTMS stimulations in NPMA in patients/83.87% in healthy volunteers in patients/83.87% in healthy volunteers did not result in MEPs ≥ 50 μV. Positive nTMS mapping in NPMA correlated with higher stimulation intensity and larger M1 areas in patients (120% M1 RMT SI p = 0.005/150% M1 RMT SI p = 0.198).
Conclusion
Our findings indicate that in case of positive nTMS mapping in NPMA, MEPs originate mostly from M1. For future studies, MEP parameters and TMS coil rotation should be studied closely to assess the risk for postoperative motor deterioration.






Similar content being viewed by others
Abbreviations
- FDI:
-
First dorsal interosseous muscle
- FT:
-
Finger tapping
- KPSS:
-
Karnofsky Performance Status Scale
- MEP:
-
Motor evoked potentials
- MRC:
-
Medical Research Council
- M1:
-
Primary motor cortex
- NHPT:
-
Nine-Hole Peg Test
- NPMA:
-
Non-primary motor areas
- nTMS:
-
Navigated transcranial magnetic stimulation
- PMC:
-
Premotor cortex
- RMT:
-
Resting motor threshold
- SMA:
-
Supplementary motor area
References
Ahdab R, Ayache SS, Brugieres P, Farhat WH, Lefaucheur JP (2016) The hand motor hotspot is not always located in the hand knob: a neuronavigated transcranial magnetic stimulation study. Brain Topogr 29:590–597. https://doi.org/10.1007/s10548-016-0486-2
Barz A, Noack A, Baumgarten P, Seifert V, Forster MT (2018) Motor cortex reorganization in patients with glioma assessed by repeated navigated transcranial magnetic stimulation-a longitudinal study. World Neurosurg 112:e442–e453. https://doi.org/10.1016/j.wneu.2018.01.059
Bellace JV, Healy D, Besser MP, Byron T, Hohman L (2000) Validity of the Dexter evaluation system’s Jamar dynamometer attachment for assessment of hand grip strength in a Normal population. J Hand Ther 13:46–51. https://doi.org/10.1016/s0894-1130(00)80052-6
Bulubas L, Sabih J, Wohlschlaeger A, Sollmann N, Hauck T, Ille S, Ringel F, Meyer B, Krieg SM (2016) Motor areas of the frontal cortex in patients with motor eloquent brain lesions. J Neurosurg 125:1431–1442. https://doi.org/10.3171/2015.11.JNS152103
Civardi C, Cantello R, Asselman P, Rothwell JC (2001) Transcranial magnetic stimulation can be used to test connections to primary motor areas from frontal and medial cortex in humans. Neuroimage 14:1444–1453. https://doi.org/10.1006/nimg.2001.0918
Conway N, Wildschuetz N, Moser T, Bulubas L, Sollmann N, Tanigawa N, Meyer B, Krieg SM (2017) Cortical plasticity of motor-eloquent areas measured by navigated transcranial magnetic stimulation in patients with glioma. J Neurosurg 127:981–991. https://doi.org/10.3171/2016.9.JNS161595
Duffau H, Lopes M, Arthuis F (2005) Contribution of intraoperative electrical stimulations in surgery of low grade gliomas: a comparative study between two series without (1985-96) and with (1996-2003) functional mapping in the same institution. J Neurol Neurosurg Psychiatry 76:845–851
Duffau H (2001) Acute functional reorganisation of the human motor cortex during resection of central lesions: a study using intraoperative brain mapping. J Neurol Neurosurg Psychiatry 70:506–513
Dum RP, Strick PL (1991) The origin of corticospinal projections from the premotor areas in the frontal lobe. J Neurosci 11:667–689
Feys P, Lamers I, Francis G, Benedict R, Phillips G, LaRocca N, Hudson LD, Rudick R, Multiple Sclerosis Outcome Assessments C (2017) The Nine-Hole Peg Test as a manual dexterity performance measure for multiple sclerosis. Mult Scler 23:711–720. https://doi.org/10.1177/1352458517690824
Forster MT, Hattingen E, Senft C, Gasser T, Seifert V, Szelenyi A (2011) Navigated transcranial magnetic stimulation and functional magnetic resonance imaging: advanced adjuncts in preoperative planning for central region tumors. Neurosurgery 68:1317–1324; discussion 1324-1315. https://doi.org/10.1227/NEU.0b013e31820b528c
Forster MT, Senft C, Hattingen E, Lorei M, Seifert V, Szelenyi A (2012) Motor cortex evaluation by nTMS after surgery of central region tumors: a feasibility study. Acta Neurochir 154:1351–1359. https://doi.org/10.1007/s00701-012-1403-4
Fox PT, Narayana S, Tandon N, Sandoval H, Fox SP, Kochunov P, Lancaster JL (2004) Column-based model of electric field excitation of cerebral cortex. Hum Brain Mapp 22:1–14. https://doi.org/10.1002/hbm.20006
Fukaya C, Katayama Y, Nagaoka T, Kobayashi K, Kasai M, Oshima H, Yamamoto T (2004) Impairment of motor function after frontal lobe resection with preservation of the primary motor cortex. Int Congr Ser 1259:421–424. https://doi.org/10.1016/s0531-5131(03)01189-0
Groppa S, Werner-Petroll N, Munchau A, Deuschl G, Ruschworth MF, Siebner HR (2012) A novel dual-site transcranial magnetic stimulation paradigm to probe fast facilitatory inputs from ipsilateral dorsal premotor cortex to primary motor cortex. Neuroimage 62:500–509. https://doi.org/10.1016/j.neuroimage.2012.05.023
He SQ, Dum RP, Strick PL (1993) Topographic organization of corticospinal projections from the frontal lobe: motor areas on the lateral surface of the hemisphere. J Neurosci 13:952–980
He SQ, Dum RP, Strick PL (1995) Topographic organization of corticospinal projections from the frontal lobe: motor areas on the medial surface of the hemisphere. J Neurosci 15:3284–3306
Janssen AM, Oostendorp TF, Stegeman DF (2015) The coil orientation dependency of the electric field induced by TMS for M1 and other brain areas. J NeuroEng Rehabil 12:47. https://doi.org/10.1186/s12984-015-0036-2
Johansen-Berg H, Behrens TEJ, Robsons MD, Drobnjak I, Rushworth MFS, Brady JM, Smith SM, Higham DJ, Matthews PM (2014) Changes in connectivity profiles define functionally distinct regions in human medial frontal cortex. PNAS. 101(36):13335–13340
Julkunen P (2014) Methods for estimating cortical motor representation size and location in navigated transcranial magnetic stimulation. J Neurosci Methods 232:125–133. https://doi.org/10.1016/j.jneumeth.2014.05.020
Kim YH, Kim CH, Kim JS, Lee SK, Han JH, Kim CY, Chung CK (2015) Topographical risk factor analysis of new neurological deficits following precentral gyrus resection. Neurosurgery 76:714–720; discussion 720. https://doi.org/10.1227/NEU.0000000000000712
Krieg SM, Lioumis P, Makela JP, Wilenius J, Karhu J, Hannula H, Savolainen P, Lucas CW, Seidel K, Laakso A, Islam M, Vaalto S, Lehtinen H, Vitikainen AM, Tarapore PE, Picht T (2017) Protocol for motor and language mapping by navigated TMS in patients and healthy volunteers; workshop report. Acta Neurochir 159:1187–1195. https://doi.org/10.1007/s00701-017-3187-z
Kombos T, Suess O, Kern BC, Funk T, Hoell T, Kopetsch O, Brock M (1999) Comparison between monopolar and bipolar electrical stimulation of the motor cortex. Acta Neurochir 141:1295–1301
Liu H, Au-Yeung SS (2014) Reliability of transcranial magnetic stimulation induced corticomotor excitability measurements for a hand muscle in healthy and chronic stroke subjects. J Neurol Sci 341:105–109. https://doi.org/10.1016/j.jns.2014.04.012
Mäkela JP, Vitikainen AM, Lioumis P, Paetau R, Ahtola E, Kuusela L, Valanne L, Blomstedt G, Gaily E (2013) Functional plasticity of the motor cortical structures demonstrated by navigated TMS in two patients with epilepsy. Brain Stimul 6:286–291. https://doi.org/10.1016/j.brs.2012.04.012
Medical Research Council (1975) Aids to the examination of the peripheral nervous system. Memorandum No. 45. Her Majesty’s Stationery Office, London
Mills KR, Boniface SJ, Schubert M (1992) Magnetic brain stimulation with a double coil: the importance of coil orientation. Electroencephalogr Clin Neurophysiol 85:17–21
Moser T, Bulubas L, Sabih J, Conway N, Wildschutz N, Sollmann N, Meyer B, Ringel F, Krieg SM (2017) Resection of navigated transcranial magnetic stimulation-positive prerolandic motor areas causes permanent impairment of motor function. Neurosurgery 81:99–110. https://doi.org/10.1093/neuros/nyw169
Münchau A, Bloem BR, Irlbacher K, Trimble MR, Rothwell JC (2002) Functional connectivity of human premotor and motor cortex explored with repetitive transcranial magnetic stimulation. J Neurosci 22:554–561
Penfield W, Welch K (1951) The supplementary motor area in the cerebral cortex of man; a clinical and experimental study. AMA Arch Neurol Psychiatry 66(3):289–317
Picht T, Mularski S, Kuehn B, Vajkoczy P, Kombos T, Suess O (2009) Navigated transcranial magnetic stimulation for preoperative functional diagnostics in brain tumor surgery. Neurosurgery 65:93–98; discussion 98-99. https://doi.org/10.1227/01.NEU.0000348009.22750.59
Pigorini A, Casali AG, Casarotto S, Ferrarelli F, Baselli G, Mariotti M, Massimini M, Rosanova M (2011) Time-frequency spectral analysis of TMS-evoked EEG oscillations by means of Hilbert-Huang transform. J Neurosci Methods 198(2011):236–245
Rossi S, Hallett M, Rossini PM, Pascual-Leone A, Safety of TMSCG (2009) Safety, ethical considerations, and application guidelines for the use of transcranial magnetic stimulation in clinical practice and research. Clin Neurophysiol 120:2008–2039. https://doi.org/10.1016/j.clinph.2009.08.016
Rossini PM, Barker AT, Berardelli A, Caramia MD, Caruso G, Cracco RQ, Dimitrijevic MR, Hallett M, Katayama Y, Lucking CH et al (1994) Non-invasive electrical and magnetic stimulation of the brain, spinal cord and roots: basic principles and procedures for routine clinical application. Report of an IFCN committee. Electroencephalogr Clin Neurophysiol 91:79–92
Rothwell J (2009) Chapter 4 meet the brain. In. International review of neurobiology. pp 51-65. https://doi.org/10.1016/s0074-7742(09)86004-2
Ruohonen J, Karhu J (2010) Navigated transcranial magnetic stimulation. Neurophysiol Clin 40:7–17. https://doi.org/10.1016/j.neucli.2010.01.006
Salo KST, Vaalto SMI, Mutanen TP, Stenroos M, Illmoniemi RJ (2018) Individual activation patterns after the stimulation of different motor areas: a transcranial magnetic stimulation–electroencephalography study. Brain Connectivity 8(7):420–428
Schag CC, Heinrich RL, Ganz PA (1984) Karnofsky performance status revisited: reliability, validity, and guidelines. J Clin Oncol 2:187–193
Schluter ND, Rushworth MF, Passingham RE, Mills KR (1998) Temporary interference in human lateral premotor cortex suggests dominance for the selection of movements. A study using transcranial magnetic stimulation. Brain 121(Pt 5):785–799
Schmidt S, Cichy RM, Kraft A, Brocke J, Irlbacher K, Brandt SA (2009) An initial transient-state and reliable measures of corticospinal excitability in TMS studies. Clin Neurophysiol 120:987–993. https://doi.org/10.1016/j.clinph.2009.02.164
Schmidt S, Fleischmann R, Bathe-Peters R, Irlbacher K, Brandt SA (2013) Evolution of premotor cortical excitability after cathodal inhibition of the primary motor cortex: a sham-controlled serial navigated TMS study. PLoS One 8:e57425. https://doi.org/10.1371/journal.pone.0057425
Shah KB, Hayman LA, Chavali LS, Hamilton JD, Prabhu SS, Wangaryattawanich P, Kumar VA, Kumar AJ (2015) Glial tumors in brodmann area 6: spread pattern and relationships to motor areas. Radiographics 35:793–803. https://doi.org/10.1148/rg.2015140207
Shimoyama I, Ninchoji T, Uemura K (1990) The finger-tapping test. A quantitative analysis. Arch Neurol 47:681–684
Takahashi S, Jussen D, Vajkoczy P, Picht T (2012) Plastic relocation of motor cortex in a patient with LGG (low grade glioma) confirmed by NBS (navigated brain stimulation). Acta Neurochir 154:2003–2008; discussion 2008. https://doi.org/10.1007/s00701-012-1492-0
Teitti S, Maatta S, Saisanen L, Kononen M, Vanninen R, Hannula H, Mervaala E, Karhu J (2008) Non-primary motor areas in the human frontal lobe are connected directly to hand muscles. Neuroimage 40:1243–1250. https://doi.org/10.1016/j.neuroimage.2007.12.065
Van de Ruit M, Grey MJ (2016) The TMS map scales with increased stimulation intensity and muscle activation. Brain Topogr 29(1):56–66. https://doi.org/10.1007/s10548-015-0447-1
Young NA, Collins CE, Kaas JH (2013) Cell and neuron densities in the primary motor cortex of primates. Front Neural Circuits 7:30. https://doi.org/10.3389/fncir.2013.00030
Yousry T, Schmid U, Alkadhi H, Schmidt D, Peraud A, Buettner A, Winkler P (1997) Localization of the motor hand area to a knob on the precentral gyrus. A new landmark. Brain 120:141–157
Funding
Matters of Activity. Image Space Material. An Interdisciplinary Laboratory Cluster of Excellence at the Humboldt-Universität zu Berlin (sponsor number EXC 2025/1) with financial support from the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation) supported the research. The sponsor had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Data collection was conducted in accordance with the ethical standards set forth by the ethics commission of the Charité University Hospital in Berlin (EA 2/135/14), local ethics committees, and the Declaration of Helsinki.
Conflict of interest
Thomas Picht has served as a speaker for a TMS manufacturer (Nexstim Oy) but is not a contracted consultant. All other authors certify that they have no affiliations with or involvement in any organisation or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Ethics Commission of the Charité University Hospital and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Comments
Navigated TMS is increasingly used as a preoperative tool to map cortical areas involved in motor and speech functions. It has long been postulated, and recently also shown, that pathological processes, such as intra-axial tumours and epileptogenic lesions within eloquent cortex, may induce plastic changes resulting in transfer of function away from the original sites to nearby, less affected cortical regions. While intraoperative direct cortical stimulation remains the gold standard method for mapping the functional cortex, we and others have found nTMS as a very useful tool in predicting the most likely positive stimulation sites, thereby facilitating both the planning of the surgery and the actual intraoperative mapping. It is certainly comforting for the neurosurgeon to be prepared to expect positive stimulation sites in regions that might be unexpected based only on classical anatomical landmarks, and avoiding unnecessary confusion in the operating room also saves valuable time during surgery.
This work from a very experienced nTMS research team is important in describing a potential source of error during nTMS mapping - without care, one might interpret the results as plastic changes in a situation where there is none! Studies like this are very important to advance our understanding and applicability of nTMS as a preoperative mapping technique.
Aki Laakso and Pantelis Lioumis
Helsinki, Finland
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Brain Tumors
Rights and permissions
About this article
Cite this article
Mirbagheri, A., Schneider, H., Zdunczyk, A. et al. NTMS mapping of non-primary motor areas in brain tumour patients and healthy volunteers. Acta Neurochir 162, 407–416 (2020). https://doi.org/10.1007/s00701-019-04086-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-019-04086-x