Abstract
Objective
The aim was to study the prevalence of secondary adrenal insufficiency before and after surgery for non-functioning pituitary adenomas, as well as determine risk factors for developing secondary adrenal insufficiency. A secondary aim was to determine adequate p-cortisol response to a 1-μg Short Synacthen Test after surgery.
Design
Longitudinal cohort study.
Methods
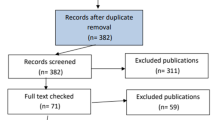
One hundred seventeen patients (52/65 females/males, age 59 years) undergoing primary surgery for clinically non-functioning pituitary adenomas were included. P-cortisol was measured in morning blood samples. Three months after surgery, a Short Synacthen Test was performed.
Results
All tumours were macroadenomas (mean size 26.9 mm, range 13–61 mm). The surgical indications were visual impairment (93), tumour growth (16), pituitary apoplexy (6) and headache (2). Before surgery, 17% of the patients had secondary adrenal insufficiency (SAI), decreasing to 15% 3 months postoperatively. Risk of SAI was increased in patients operated for pituitary apoplexy (p < 0.001), while age, sex, tumour size and complication rate were not different from the remaining cohort. Three months after surgery, all patients with baseline p-cortisol ≥ 172 nmol/l (6.2 μg/dl) and peak p-cortisol during Short Synacthen Test ≥ 320 nmol/l (11.6 μg/dl) tapered cortisone unproblematically. In patients with intact hypothalamic-pituitary-adrenal axis, p-cortisol peaked < 500 nmol/l (18.1 μg/dl) during Short Synacthen Test in 48% of patient.
Conclusion
Pituitary surgery is safe and transsphenoidal surgery rarely causes new SAI. Relying solely on morning p-cortisol for diagnosing secondary adrenal insufficiency gives false positives and the Short Synacthen Test remains useful. A peak p-cortisol ≥ 320 during (11.6 μg/dl) Short Synacthen Test indicates a sufficient response, while < 309 nmol/l (11.2 μg/dl) indicates secondary adrenal insufficiency.

Similar content being viewed by others
References
Abdu TAM, Elhadd TA, Neary R, Clayton RN (1999) Comparison of the low dose short Synacthen test (1 μg), the conventional dose short Synacthen test (250 μg), and the insulin tolerance test for assessment of the hypothalamo-pituitary-adrenal axis in patients with pituitary disease. J Clin Endocrinol Metab 84(3):838–843
Agustsson TT, Baldvinsdottir T, Jonasson JG, Olafsdottir E, Steinthorsdottir V, Sigurdsson G, Thorsson AV, Carroll PV, Korbonits M, Benediktsson R (2015) The epidemiology of pituitary adenomas in Iceland, 1955–2012: a nationwide population-based study. Eur J Endocrinol 173(5):655–664
Ajlan A, Almufawez KA, Albakr A, Katznelson L, Harsh GR (2018) Adrenal axis insufficiency after endoscopic transsphenoidal resection of pituitary adenomas. World Neurosurg 112:e869–e875
Barker FG, Klibanski A, Swearingen B (2003) Transsphenoidal surgery for pituitary tumors in the United States, 1996–2000: mortality, morbidity, and the effects of hospital and surgeon volume. J Clin Endocrinol Metab 88(10):4709–4719
Briet C, Salenave S, Bonneville J-F, Laws ER, Chanson P (2015) Pituitary apoplexy. Endocr Rev 36(6):622–645
Caputo C, Sutherland T, Farish S, McNeill P, Ng KW, Inder WJ (2013) Gender differences in presentation and outcome of nonfunctioning pituitary macroadenomas. Clin Endocrinol 78(4):564–570
Charmandari E, Nicolaides NC, Chrousos GP (2014) Adrenal insufficiency. Lancet 383(9935):2152–2167
Chen L, White WL, Spetzler RF, Xu B (2011) A prospective study of nonfunctioning pituitary adenomas: presentation, management, and clinical outcome. J Neuro-Oncol 102(1):129–138
Dallapiazza RF, Grober Y, Starke RM, Laws ER, Jane JA (2015) Long-term results of endonasal endoscopic transsphenoidal resection of nonfunctioning pituitary macroadenomas. Neurosurgery 76(1):42–53
Dekkers OM, van der Klaauw AA, Pereira AM, Biermasz NR, Honkoop PJ, Roelfsema F, Smit JWA, Romijn JA (2006) Quality of life is decreased after treatment for nonfunctioning pituitary macroadenoma. J Clin Endocrinol Metab 91(9):3364–3369
Dekkers OM, Pereira AM, Roelfsema F, Voormolen JHC, Neelis KJ, Schroijen MA, Smit JWA, Romijn JA (2006) Observation alone after transsphenoidal surgery for nonfunctioning pituitary macroadenoma. J Clin Endocrinol Metab 91(5):1796–1801
Dekkers OM, Pereira AM, Romijn JA (2008) Treatment and follow-up of clinically nonfunctioning pituitary macroadenomas. J Clin Endocrinol Metab 93(10):3717–3726
Fatemi N, Dusick JR, Mattozo C, McArthur DL, Cohan P, Boscardin J, Wang C, Swerdloff RS, Kelly DF (2008) Pituitary hormonal loss and recovery after transsphenoidal adenoma removal. Neurosurgery 63(4):709–719
Fernandez-Rodriguez E, Lopez-Raton M, Andujar P, Martinez-Silva IM, Cadarso-Suarez C, Casanueva FF, Bernabeu I (2013) Epidemiology, mortality rate and survival in a homogeneous population of hypopituitary patients. Clin Endocrinol 78(2):278–284
Filipsson H, Monson JP, Koltowska-Häggström M, Mattsson A, Johannsson G (2006) The impact of glucocorticoid replacement regimens on metabolic outcome and comorbidity in hypopituitary patients. J Clin Endocrinol Metab 91(10):3954–3961
Freda PU, Beckers AM, Katznelson L, Molitch ME, Montori VM, Post KD, Vance ML (2011) Pituitary incidentaloma: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 96(4):894–904
Gonzálbez J, Villabona C, Ramón J, Navarro MA, Giménez O, Ricart W, Soler J (2000) Establishment of reference values for standard dose short synacthen test (250 μg), low dose short Synacthen test (1 μg) and insulin tolerance test for assessment of the hypothalamo–pituitary–adrenal axis in normal subjects. Clin Endocrinol 53(2):199–204
Greenman Y, Ouaknine G, Veshchev I, Reider-Groswasser II, Segev Y, Stern N (2003) Postoperative surveillance of clinically nonfunctioning pituitary macroadenomas: markers of tumour quiescence and regrowth. Clin Endocrinol 58(6):763–769
Halvorsen H, Ramm-Pettersen J, Josefsen R, Rønning P, Reinlie S, Meling T, Berg-Johnsen J, Bollerslev J, Helseth E (2014) Surgical complications after transsphenoidal microscopic and endoscopic surgery for pituitary adenoma: a consecutive series of 506 procedures. Acta Neurochir 156(3):441–449
Hammarstrand C, Ragnarsson O, Hallén T, Andersson E, Skoglund T, Nilsson AG, Johannsson G, Olsson DS (2017) Higher glucocorticoid replacement doses are associated with increased mortality in patients with pituitary adenoma. Eur J Endocrinol 177(3):251–256
Jahangiri A, Wagner JR, Pekmezci M, Hiniker A, Chang EF, Kunwar S, Blevins L, Aghi MK (2013) A comprehensive long-term retrospective analysis of silent corticotrophic adenomas vs hormone-negative adenomas. Neurosurgery 73(1):8–18
Klose M, Lange M, Kosteljanetz M, Poulsgaard L, Feldt-Rasmussen U (2005) Adrenocortical insufficiency after pituitary surgery: an audit of the reliability of the conventional short Synacthen test. Clin Endocrinol 63(5):499–505
Lindholm J, Kehlet H (1987) Re-evaluation of the clinical value of the 30 min ACTH test in assessing the hypothalamic-pituitary-adrenocortical function. Clin Endocrinol 26(1):53–59
Mayenknecht J, Diederich S, Bähr V, Plöckinger U, Oelkers W (1998) Comparison of low and high dose corticotropin stimulation tests in patients with pituitary disease. J Clin Endocrinol Metab 83(5):1558–1562
Nomikos P, Ladar C, Fahlbusch R, Buchfelder M (2004) Impact of primary surgery on pituitary function in patients with non-functioning pituitary adenomas—a study on 721 patients. Acta Neurochir 146(1):27–35
Puar THK, Stikkelbroeck NMML, Smans LCCJ, Zelissen PMJ, Hermus ARMM (2016) Adrenal crisis: still a deadly event in the 21st century. Am J Med 129(3):339.e1–339.e9
Regal M, Páramo C, Sierra JM, García-Mayor RV (2001) Prevalence and incidence of hypopituitarism in an adult Caucasian population in northwestern Spain. Clin Endocrinol 55(6):735–740
Tjörnstrand A, Gunnarsson K, Evert M, Holmberg E, Ragnarsson O, Rosén T, Filipsson Nyström H (2014) The incidence rate of pituitary adenomas in western Sweden for the period 2001–2011. Eur J Endocrinol 171(4):519–526
Tomlinson J, Holden N, Hills R, Wheatley K, Clayton R, Bates A, Sheppard M, Stewart P (2001) Association between premature mortality and hypopituitarism. Lancet 357(9254):425–431
Webb SM, Rigla M, Wägner A, Oliver B, Bartumeus F (1999) Recovery of hypopituitarism after neurosurgical treatment of pituitary adenomas. J Clin Endocrinol Metab 84(10):3696–3700
Wei L, MacDonald TM, Walker BR (2004) Taking glucocorticoids by prescription is associated with subsequent cardiovascular disease. Ann Intern Med 141(10):764
Acknowledgements
We thank Kari Abelsen and Ansgar Heck for assistance and support. This study was based on routine practice at the Section of Specialized Endocrinology, Rikshospitalet, Oslo University Hospital in Oslo, and did not receive additional funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements) or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the hospital authority, regional ethics committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Comments
This is a welcome update regarding the most recent and most logical method of post operative assessment of adrenal insufficiency and the need for and calibration of cortisol replacement therapy, assessed initially and over time.
E.R. Laws
Boston, MA, USA
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Pituitaries
Rights and permissions
About this article
Cite this article
Kolnes, A.J., Øystese, K.A., Dahlberg, D. et al. Cut-off values for sufficient cortisol response to low dose Short Synacthen Test after surgery for non-functioning pituitary adenoma. Acta Neurochir 162, 845–852 (2020). https://doi.org/10.1007/s00701-019-04068-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-019-04068-z