Abstract
Background
The use of intraoperative ultrasound (iUS) has increased in the last 15 years becoming a standard tool in many neurosurgical centers. Our aim was to assess the utility of routine use of iUS during various types of intracranial surgery. We reviewed our series to assess ultrasound visibility of different pathologies and iUS applications during the course of surgery.
Materials and methods
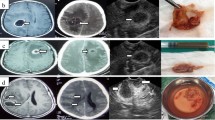
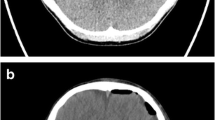
This is a retrospective review of 162 patients who underwent intracranial surgery with assistance of the iUS guidance system (SonoWand). Pathologic categories were neoplastic (135), vascular (20), infectious (2), and CSF related (5). Ultrasound visibility was assessed using the Mair classification, a four-tiered grading system that considers the echogenicity of the lesion and its border visibility (from 0 to 3; grade 0, pathology not visible; grade 3, visible with clear border with normal tissue). iUS applications included lesion localization, approach planning to deep-seated lesions, and lesion removal.
Results
All pathologies were visible on iUS except one aneurysm. On average, extra-axial tumors were identified more easily and had clearer limits compared to intra-axial tumors (extra-axial 17% grade 2, 83% grade 3; intra-axial 5.5% grade 1, 46.5% grade 2, 48% grade 3). iUS provided precise and safe transcortical trajectories to deep-seated lesions (71 patients; tumors, hemangiomas, ICHs); iUS was judged to be less useful to approach skull base tumors and aneurysms. iUS was used to judge extent of resection in 152 cases; surgical artifacts reduced sonographic visibility in 25 cases: extent of resection was correctly checked in 127 patients (53 gliomas, 15 metastases, 39 meningiomas, 4 schwannomas, 4 sellar region tumors, 6 hemangiomas, 3 AVMs, 2 abscesses).
Conclusions
iUS was highly sensitive in detecting all types of pathology, was safe and precise in planning trajectories to intraparenchymal lesions (including minimally mini-invasive approaches), and was accurate in checking extent of resection in more than 80% of cases. iUS is a versatile and feasible tool; it could improve safety and its use may be considered in routine intracranial surgery.






Similar content being viewed by others
Abbreviations
- HGG:
-
High-grade glioma
- LGG:
-
Low-grade glioma
- ICH:
-
Intracerebral hematoma
- AVM:
-
Artero-venous malformation
- US:
-
Ultrasound
- iUS:
-
Intraoperative US
- CECT:
-
Contrast-enhanced CT scan
References
Chacko AG, Kumar NK, Chacko G, Athyal R, Rajshekhar V (2003) Intraoperative ultrasound in determining the extent of resection of parenchymal brain tumours—a comparative study with computed tomography and histopathology. Acta Neurochir 145(9):743–748
Coburger J, König RW (2016). Intraoperative findings in brain tumor surgery. In: Prada F, Solbiati L, Martegani A, Di Meco F, editors. Intraoperative ultrasound (IOUS) in neurosurgery. From standard-B-mode to elastosonography. Switzerland Springer, pp 41–59
Gerganov VM, Samii A, Akbarian A, Stieglitz L, Samii M, Fahlbusch R (2009) Reliability of intraoperative high-resolution 2D ultrasound as an alternative to high-field strength MR imaging for tumor resection control: a prospective comparative study. J Neurosurg 2009 111(3):512–519
Gerganov VM, Samii A, Giordano M, Samii M, Fahlbusch R (2011) Two-dimensional high-end ultrasound imaging compared to intraoperative MRI during resection of low-grade gliomas. J Clin Neurosci 18(5):669–673
Goren O, Monteith SJ, Hadani M, Bakon M, Harnof S (2013) Modern intraoperative imaging modalities for the vascular neurosurgeon treating intracerebral hemorrhage. Neurosurg Focus 34(5):E2
Gronningsaeter A, Kleven A, Ommedal S, Aarseth TE, Lie T, Lindseth F, Langø T, Unsgård G (2000) SonoWand, an ultrasound-based neuronavigation system. Neurosurgery 47(6):1373–1379
Jakola AS, Reinertsen I, Selbekk T, Solheim O, Lindseth F, Gulati S, Unsgård G (2014) Three-dimensional ultrasound-guided placement of ventricular catheters. World Neurosurg 82(3–4):536.e5–536.e9
Mair R, Heald J, Poeata I, Ivanov M (2013) A practical grading system of ultrasonographic visibility for intracerebral lesions. Acta Neurochir 155(12):2293–2298
Miller D, Benes L, Sure U (2011) Stand-alone 3D-ultrasound navigation after failure of conventional image guidance for deep-seated lesions. Neurosurg Rev 34(3):381–387
Miller D, Heinze S, Tirakotai W, Bozinov O, Sürücü O, Benes L, Bertalanffy H, Sure U (2007) Is the image guidance of ultrasonography beneficial for neurosurgical routine? Surg Neurol 67(6):579–587
Moiyadi AV, Shetty PM, Mahajan A, Udare A, Sridhar E (2013) Usefulness of three-dimensional navigable intraoperative ultrasound in resection of brain tumors with a special emphasis on malignant gliomas. Acta Neurochir 155(12):2217–2225
Rygh OM, Selbekk T, Torp SH, Lydersen S, Hernes TA, Unsgaard G (2008) Comparison of navigated 3D ultrasound findings with histopathology in subsequent phases of glioblastoma resection. Acta Neurochir 150(10):1033–1041
Sæther CA, Torsteinsen M, Torp SH, Sundstrøm S, Unsgård G, Solheim O (2012) Did survival improve after the implementation of intraoperative neuronavigation and3D ultrasound in glioblastoma surgery? A retrospective analysis of 192 primary operations. J Neurol Surg A Cent Eur Neurosurg 73(2):73–78
Shinoura N, Takahashi M, Yamada R (2006) Delineation of brain tumor margins using intraoperative sononavigation: implications for tumor resection. J Clin Ultrasound 34(4):177–183
Solheim O, Selbekk T, Lindseth F, Unsgård G (2009) Navigated resection of giant intracranial meningiomas based on intraoperative 3D ultrasound. Acta Neurochir 151(9):1143–1151
Solheim O, Selbekk T, Jakola AS, Unsgård G (2010) Ultrasound-guided operations in unselected high-grade gliomas—overall results, impact of image quality and patient selection. Acta Neurochir 152(11):1873–1886
Sosna J, Barth MM, Kruskal JB, Kane RA (2005) Intraoperative sonography for neurosurgery. J Ultrasound Med 24(12):1671–1682
Tronnier VM, Bonsanto MM, Staubert A, Knauth M, Kunze S, Wirtz CR (2001) Comparison of intraoperative MR imaging and 3D-navigated ultrasonography in the detection and resection control of lesions. Neurosurg Focus 10(2):E3
Unsgaard G, Gronningsaeter A, Ommedal S, Nagelhus Hernes TA (2002) Brain operations guided by real-time two-dimensional ultrasound: new possibilities as a result of improved image quality. Neurosurgery 51(2):402–411
Unsgaard G, Ommedal S, Muller T, Gronningsaeter A, Nagelhus Hernes TA (2002) Neuronavigation by intraoperative three-dimensional ultrasound: initial experience during brain tumor resection. Neurosurgery 50(4):804–812
Unsgaard G, Rygh OM, Selbekk T, Müller TB, Kolstad F, Lindseth F, Hernes TA (2006) Intra-operative 3D ultrasound in neurosurgery. Acta Neurochir 148(3):235–253
Unsgaard G, Selbekk T, Brostrup Müller T, Ommedal S, Torp SH, Myhr G, Bang J, Nagelhus Hernes TA (2005) Ability of navigated 3D ultrasound to delineate gliomas and metastases—comparison of image interpretations with histopathology. Acta Neurochir 147(12):1259–1269
Wang J, Liu X, Hou WH, Dong G, Wei Z, Zhou H, Duan YY (2008) The relationship between intra-operative ultrasonography and pathological grade in cerebral glioma. J Int Med Res 36(6):1426–1434
Woydt M, Krone A, Becker G, Schmidt K, Roggendorf W, Roosen K (1996) Correlation of intra-operative ultrasound with histopathologic findings after tumour resection in supratentorial gliomas. A method to improve gross total tumour resection. Acta Neurochir 138(12):1391–1398
Woydt M, Krone A, Soerensen N, Roosen K (2001) Ultrasound-guided neuronavigation of deep-seated cavernous haemangiomas: clinical results and navigation techniques. Br J Neurosurg 15(6):485–495
Acknowledgements
We would like to thank Dr. Justin Mascitelli (Neurosurgeon at Barrow Neurological Institute) for the English revision and for his precious intellectual support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Policicchio, D., Doda, A., Sgaramella, E. et al. Ultrasound-guided brain surgery: echographic visibility of different pathologies and surgical applications in neurosurgical routine. Acta Neurochir 160, 1175–1185 (2018). https://doi.org/10.1007/s00701-018-3532-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-018-3532-x