Abstract
Background
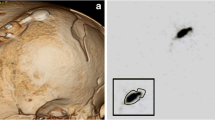
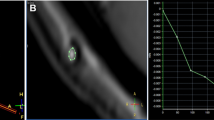
Obstruction is a common cause of ventriculo-peritoneal shunt failure. Head computed tomography and plain x-ray examinations of shunt tubing (“shunt series”) are routinely used in patients readmitted for reemerging symptoms but are of limited value. The validity of shunt series can be improved by applying contrast agent into the system (contrast-enhanced shunt series, a.k.a. a “shuntogram” or “shuntography”). We hypothesized that contrast-enhanced shunt series have a high predictive value for shunt revision surgeries.
Methods
We retrospectively re-evaluated 107 contrast-enhanced shunt series and reviewed the patient histories. We defined outcome parameters for calculating the utility of a pathological contrast-enhanced shunt series in predicting revision surgery.
Results
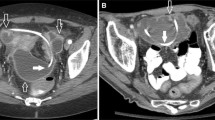
Of 107 contrast-enhanced shunt series, 41 examinations were positive for obstruction, mainly of the ventricular (36.5 %) and the peritoneal catheter (48.8 %). Within 30 days, 35 successful revision surgeries and 3 revision surgeries without resolution of symptoms were performed. In two cases the shunt tubing was found to be patent. Sixty-six negative examinations resulted in two revision surgeries, in addition to ten surgeries not attempting to restore patency. After 30 days, the specificity of contrast-enhanced shunt series for shunt failure identification was calculated at 92.8 %, the sensitivity at 94.7 %, the positive predictive value at 87.8 %, and the negative predictive value at 97.0 %.
Conclusions
The contrast-enhanced shunt series method is a highly specific examination with a negative predictive value exceeding that of head computed tomography and plain shunt series. Compared to radionuclide marker studies, contrast-enhanced shunt series demonstrate better spatiotemporal resolution, enabling focused local surgical repair.




Similar content being viewed by others
Abbreviations
- CSF:
-
cerebrospinal fluid
- HCP:
-
hydrocephalus
- HCT:
-
head computed tomography
- NPH:
-
normal pressure hydrocephalus
- PACS:
-
picture archive and communication system
References
Buchanan CC, Hernandez EA, Anderson JM, Dye JA, Leung M, Buxey F, Bergsneider M, Afsar-Manesh N, Pouratian N, Martin NA (2014) Analysis of 30-day readmissions among neurosurgical patients: surgical complication avoidance as key to quality improvement. J Neurosurg 121(1):170–175
Wong JM, Ziewacz JE, Ho AL, Panchmatia JR, Bader AM, Garton HJ, Laws ER, Gawande AA (2012) Patterns in neurosurgical adverse events: cerebrospinal fluid shunt surgery. Neurosurg Focus 33(5):E13
Johanson CE (2011) Clinical Evaluation of adult hydrocephalus. In: Winn HR (ed) Youmans neurological surgery. Elsevier, Philadelphia, pp 487–514
Griffey RT, Ledbetter S, Khorasani R (2007) Yield and utility of radiographic “shunt series” in the evaluation of ventriculo-peritoneal shunt malfunction in adult emergency patients. Emerg Radiol 13(6):307–311
Lehnert BE, Rahbar H, Relyea-Chew A, Lewis DH, Richardson ML, Fink JR (2011) Detection of ventricular shunt malfunction in the ED: relative utility of radiography, CT, and nuclear imaging. Emerg Radiol 18(4):299–305
Vassilyadi M, Tataryn ZL, Alkherayf F, Udjus K, Ventureyra EC (2010) The necessity of shunt series. J Neurosurg Pediatr 6(5):468–473
Mater A, Shroff M, Al-Farsi S, Drake J, Goldman RD (2008) Test characteristics of neuroimaging in the emergency department evaluation of children for cerebrospinal fluid shunt malfunction. CJEM 10(2):131–135
Iskandar BJ, McLaughlin C, Mapstone TB, Grabb PA, Oakes WJ (1998) Pitfalls in the diagnosis of ventricular shunt dysfunction: radiology reports and ventricular size. Pediatrics 101(6):1031–1036
Chern JJ, Macias CG, Jea A, Curry DJ, Luerssen TG, Whitehead WE (2010) Effectiveness of a clinical pathway for patients with cerebrospinal fluid shunt malfunction. J Neurosurg Pediatr 6(4):318–324
Thompson EM, Wagner K, Kronfeld K, Selden NR (2014) Using a 2-variable method in radionuclide shuntography to predict shunt patency. J Neurosurg 121(6):1504–1507
Blair K, AuCoin R, Kloiber R, Molnar CP (1989) The complementary role of plain radiographs and radionuclide shuntography in evaluating CSF-VP shunts. Clin Nucl Med 14(2):121–123
Bartynski WS, Valliappan S, Uselman JH, Spearman MP (2000) The adult radiographic shuntogram. AJNR Am J Neuroradiol 21(4):721–726
Chiewvit S, Nuntaaree S, Kanchaanapiboon P, Chiewvit P (2014) Assessment lumboperitoneal or ventriculoperitoneal shunt patency by radionuclide technique: a review experience cases. World J Nucl Med 13(2):75–84
Clyde BL, Albright AL (1995) Evidence for a patent fibrous tract in fractured, outgrown, or disconnected ventriculoperitoneal shunts. Pediatr Neurosurg 23(1):20–25
May CH, Aurisch R, Kornrumpf D, Vogel S (1999) Evaluation of shunt function in hydrocephalic patients with the radionuclide 99mTc-pertechnetate. Childs Nerv Syst 15(5):239–244, discussion 245
O’Brien DF, Taylor M, Park TS, Ojemann JG (2003) A critical analysis of ‘normal’ radionucleotide shuntograms in patients subsequently requiring surgery. Childs Nerv Syst 19(5-6):337–341
Vassilyadi M, Tataryn ZL, Matzinger MA, Briggs V, Ventureyra EC (2006) Radioisotope shuntograms at the Children’s Hospital of Eastern Ontario. Childs Nerv Syst 22(1):43–49
Chung JJ, Yu JS, Kim JH, Nam SJ, Kim MJ (2009) Intraabdominal complications secondary to ventriculoperitoneal shunts: CT findings and review of the literature. AJR Am J Roentgenol 193(5):1311–1317
Briggs JR, Hendry GM, Minns RA (1984) Abdominal ultrasound in the diagnosis of cerebrospinal fluid pseudocysts complicating ventriculoperitoneal shunts. Arch Dis Child 59(7):661–664
Kurwale NS, Agrawal D (2011) Phase-contrast magnetic resonance imaging of intracranial shunt tube: a valuable adjunct in the diagnosis of ventriculoperitoneal shunt malfunction. Clin Neurosurg 58:138–142
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this research.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements) or non-financial interest (such as personal or professional relationships, affiliations, knowledge or belief) in the subject matter or materials discussed in this manuscript.
Ethical approval
For this type of study formal consent is not required.
Additional information
Comments
Shunting dysfunctions represent very challenging issues in neurosurgery because of the heterogeneity of patients and hardware. Neurosurgeons are often required to solve life-treating situations at the last minute, frequently without the necessary information. However, the matter is underrepresented in the contemporary literature. Alternative methods, like injection of radionuclide markers or MRI or x-ray examinations, are penalized by low predictive values. In this context, the presented manuscript is welcome in order to present the authors’ results using an easy, cheap, and efficient method to identify the cause of shunting dysfunction, the so-called shuntography.
The authors retrospectively evaluated 133 contrast-enhanced shunt series over a 6.5-year time period. The study presents the typical heterogeneity of these patients: different pathologies, different shunts and valve types, and different age groups. Nevertheless, the authors performed a very exemplary analysis of the data resulting in four cases with false -egative and nine case of false-positive results; moreover, one patient experienced an allergic reaction in all probability caused by iopamidol, off-label for contrast-enhanced shunt series.
Very valuable are the three described pitfalls, the no-return valve in the prechamber, the risk of damaging the valve through forceful injection of the contrast agent, and the latency-mimicking risk.
In conclusion, the authors recommend performing contrast-enhanced shunt series instead of radionuclide tracer series, which reflects our clinical experience too. Overall, the authors should be congratulated for this straightforward study.
Lehel Török Neuruppin
Alex Alfieri Neuruppin
Rights and permissions
About this article
Cite this article
von Eckardstein, K.L., Kallenberg, K., Psychogios, MN. et al. Contrast-enhanced shunt series (“shuntography”) compare favorably to other shunt imaging modalities in detecting shunt occlusion. Acta Neurochir 159, 63–70 (2017). https://doi.org/10.1007/s00701-016-3007-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-016-3007-x