Abstract
Purpose
Nutritional scores have been reported to be useful prognostic factors for various cancers. This study evaluated the usefulness of the preoperative controlling nutritional status (CONUT) score as a predictor of recurrence of non-small cell lung cancer (NSCLC).
Methods
The present study included 422 patients with stage I–IIIA NSCLC who underwent complete resection at Tohoku University Hospital between January 2010 and December 2016. The patients were divided into the low-CONUT and high-CONUT groups based on their CONUT scores. Overall survival (OS), recurrence-free survival (RFS), and cumulative recurrence rates in the low- and high-CONUT groups were evaluated retrospectively.
Results
One hundred forty-seven patients (34.8%) were assigned to the high-CONUT group. The high-CONUT group had a significantly worse performance status, pleural invasion, vascular invasion, and lung metastasis. In the whole cohort, the low-CONUT group showed better overall survival, recurrence-free survival, and a low cumulative recurrence rate in comparison to the high-CONUT group. There was no significant difference in prognosis or recurrence between the low- and high-CONUT groups after propensity score matching.
Conclusion
Patients with a high CONUT score may be at high risk of recurrence because of the high frequency of pleural invasion, vascular invasion, and lung metastasis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Non-small cell lung cancer (NSCLC) is the leading cause of cancer-related death worldwide. The 5-year overall survival (OS) rates for patients with pathological stage IA1/IA2/IA3/IB early-stage lung cancer are 90%, 85%, 80%, and 73%, respectively. There is still room for improvement [1]. Lung cancer staging, which indicates disease progression and malignancy, is determined using the TNM classification. However, even among patients with the same stage of the disease, there is wide variation in the rate of recurrence after resection. Therefore, the current TNM staging system, based on pathological findings, may be inadequate for predicting the risk of recurrence.
In addition to the factors included in the TNM classification, several other risk factors for recurrence have been reported. Pathological findings such as histological differentiation, vascular invasion, lymphatic invasion, and pleural invasion have been reported as poor prognostic factors for disease-free survival (DFS) [2,3,4]. As for clinical factors, tumor markers such as carcinoembryonic antigen and the standardized uptake value of positron emission tomography (PET) of the primary lesions, have also been reported to be risk factors for recurrence [5, 6]. To improve the prognosis of early-stage NSCLC, it is important to identify other risk factors for recurrence.
In recent years, the efficacy of several immune checkpoint inhibitors (ICIs) against advanced lung cancer has been confirmed, including nivolumab (Ono Pharmaceutical, Osaka, Japan), a PD-1 inhibitor [7]. This trend has also influenced perioperative therapy for NSCLC. The results of some trials, such as the Impower010 and Checkmate816 trials, have been reported [8, 9]. All showed favorable results. ICIs restore the host’s immune functions against cancer cells by impeding immune escape mechanisms. In basic research, the importance of regulatory T cells in suppressing anticancer immunity was already demonstrated in the late 1990s [10, 11]. Therefore, the patient’s general condition, including their immune status, may be closely related to cancer progression and recurrence.
The controlling nutritional status (CONUT), which consists of the sum of the scores for albumin, total cholesterol, and lymphocyte count, has been reported to be an indicator of the immune-nutritional status [12]. The usefulness of the CONUT score as a prognostic factor in NSCLC has been reported [13,14,15], but its effectiveness is primarily observed in DFS, OS, and cancer-specific survival. Undernourished patients without cancer may have a poor prognosis, and the relevance of the CONUT score to recurrence is unclear. This study aimed to clarify the impact of the CONUT score on the risk of recurrence in patients with completely resected NSCLC.
Methods
Ethical statement
The institutional review board of Tohoku University Hospital in Sendai, Japan, approved this retrospective review of a prospective database (approval date: September 28, 2020; approval code: 2021-1-912-1) and waived the requirement for informed consent.
Patients
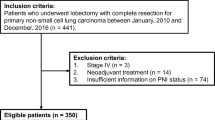
Between January 2010 and December 2016, 564 patients underwent lung resection for NSCLC at Tohoku University Hospital. Patients with pathological stages I–IIIA were included. Patients who received preoperative treatment or had a deficient preoperative CONUT score were excluded. This resulted in a total of 422 patients (Fig. 1). The selection of surgical procedure and the administration of platinum-based adjuvant chemotherapy were determined by the treating physician based on the guidelines for lung cancer treatment. Patients were regularly evaluated at three-month intervals for the first 2 years, and typically at 6-month intervals thereafter. Follow-up evaluations included a physical examination, chest radiography, blood examination (including tumor markers), and chest computed tomography (CT). Further evaluations, including brain magnetic resonance imaging (MRI) and PET/CT, were performed whenever symptoms or signs of recurrence were detected. All patients were followed-up for at least 5 years after surgery. Recurrence was diagnosed based on compatible physical examination and diagnostic imaging findings, and histological confirmation was obtained when clinically indicated.
Clinicopathologic evaluations
All patient information was extracted from electronic medical records and databases, and clinical and pathological staging was reassessed according to the eighth edition of the TNM classification [1]. Histological typing was performed according to the World Health Organization classification [16]. The preoperative nutritional status was scored and evaluated using the CONUT score, which represents the sum of the scores for albumin, total cholesterol, and lymphocyte count [12] based on preoperative blood tests. The CONUT score is an index that evaluates the nutritional status. It is calculated as the sum of scores for albumin (0 to 6), total cholesterol (0 to 3), and lymphocyte count (0 to 3). CONUT scores of 0–1, 2–4, 5–8, and 9–12 are classified as normal, mild, moderate, and severe, respectively. In the present study, we classified patients with CONUT scores of 0–1 (normal nutrition) into the low-CONUT group, and those with scores of ≥ 2 (low nutrition) into the high-CONUT group based on previous reports.
Statistical analysis
OS was defined as the period from surgery to death from any cause or the date of the last follow-up examination. Recurrence-free survival (RFS) was defined as the period from surgery to recurrence, death from any cause, or censorship at the final follow-up examination. The cumulative recurrence rate (CRR) was defined as the period from surgery to recurrence or censored at the last follow-up examination. Patient characteristics were summarized using frequencies and descriptive statistics, such as medians and ranges. OS, RFS, and CRR were estimated using the Kaplan–Meier method. Hazard ratios (HRs) and confidence intervals (CIs) were estimated using univariate and multivariate proportional hazard models.
To eliminate as much bias as possible, propensity score matching (PSM) was performed, with age, sex, performance status (PS), pathological stage, pleural invasion, lymphatic invasion, vascular invasion, and pulmonary metastasis included as covariates. A total of 270 patients were included in the propensity score-matched cohort (Fig. 2).
All statistical analyses were performed using JMP Pro version 17.1.0 (SAS Institute, Cary, NC, USA). Statistical significance was set at p < 0.05, without adjustment for multiple tests.
Results
Patient characteristics
The clinicopathological characteristics of the patients (male, n = 236; female, n = 186; median age, 69 years; range 22–96) are shown in Tables 1 and 2. There were 45 patients with PS ≥ 1, 278 were ever-smokers, 350 underwent lobectomy, 313 had adenocarcinoma, 107 had other histologic types, and 309, 73, and 40 had pathological stages I, II, and III, respectively. One hundred four patients had pleural invasion, 156 had vascular invasion, 114 had lymphatic invasion, and 13 had pulmonary metastasis. Recurrence was observed in 102 patients. The high-CONUT group had a significantly poorer PS and increased rates of pleural invasion, vascular invasion, and lung metastasis.
Survival analysis
The median follow-up period was 5.7 years for all patients and 6.2 years for censored patients. Patients with low CONUT scores tended to have better OS than those with high CONUT scores in the whole cohort (HR, 0.659; 95% CI 0.428–1.014; p = 0.04) (Fig. 3). Patients with low CONUT scores also had better RFS than those with high CONUT scores (HR, 0.665; 95% CI 0.470–0.940; p = 0.02). In addition, patients with low CONUT scores had a better CRR than those with high CONUT scores (HR, 0.662; 95% CI 0.447–0.980; p = 0.04). In the multivariate analysis for CRR, pathological stage and pleural invasion were independent prognostic factors, while CONUT score was not (Table 3).
Propensity score matching
After propensity score matching, there were 135 patients each in the low-CONUT and high-CONUT groups. The clinicopathological characteristics of the patients after PSM (male, n = 71; female, n = 64; median age, 70 years; range 22–86 years) are shown in Table 1. There were no significant differences in patient characteristics between the low-CONUT and high-CONUT groups.
There were no significant differences in OS, RFS, or CRR between patients with low and high CONUT scores after PSM (OS: HR 0.846, 95% CI 0.513–1.393, p = 0.51; RFS: HR 0.933, 95% CI 0.625–1.393, p = 0.74; CRR: HR 1.032, 95% CI 0.658–1.619, p = 0.89) (Figs. 3 and 4).
Discussion
In recent years, the evaluation of nutritional status as a prognostic factor for cancer has attracted attention. For example, the prognostic nutritional index, a nutritional assessment, has been reported to be a prognostic factor for various solid tumors [17, 18]. Indicators such as the neutrophil-to-lymphocyte ratio have also been reported to be associated with the prognosis of lung cancer [19]. The CONUT score is a prognostic marker for several cancers [20,21,22,23]. The CONUT score was also reported to be a prognostic factor in lung cancer [13, 24]. However, most of these studies used survival as the endpoint. The nutritional status is a reflection of overall health, even in patients without cancer, and is likely to be affected by non-cancer diseases. Therefore, the use of survival as an endpoint may not assess the true cancer prognosis. In this study, we evaluated the usefulness of the CONUT score as a prognostic factor using the cumulative recurrence rate rather than survival as the endpoint.
In our study, the high-CONUT group had significantly higher rates of pleural invasion, vascular invasion, and pulmonary metastasis. This may be attributed to suppressed anticancer immunity in patients with high CONUT scores because the nutritional status has been reported to be related to the immune status [25]. Another possibility is that the high malignancy of cancer is responsible for the nutritional status of patients with high CONUT scores. Further studies are warranted to confirm these findings.
In the whole cohort, the OS, RFS, and CRR were significantly worse in patients with high CONUT scores, as previously reported. However, the pathological grade of the cancer was also high in patients with high CONUT scores, and we added a PSM analysis to eliminate bias as much as possible. As a result, the CONUT score was not an independent prognostic factor for OS, RFS, or CRR. Therefore, nutritional assessment using the CONUT score may be a predictor of the systemic status after pulmonary resection, rather than the prognosis of cancer.
The CONUT score was not identified as a risk factor for recurrence in the present study. Although several reports have examined the association between the CONUT score and OS or RFS [13,14,15], few have examined the association between the CONUT score and the recurrence rate in patients with lung cancer. Shoji et al. reported that in pathologic stage I NSCLC, the group with high CONUT scores had significantly shorter OS, RFS, and cancer-specific survival in comparison to the group with low CONUT scores [14]. However, their study population was limited to patients with early-stage lung cancer, and only included 138 cases. They also did not consider the differences in characteristics between the low- and high-CONUT groups. We used PSM to eliminate bias as much as possible, and we believe this is why our results differ from those of previous studies.
Limitations
The present study was associated with several limitations. First, although PSM eliminated selection bias as much as possible, this was a retrospective study and a selection bias could not be completely eliminated. In addition, 114 patients were missing preoperative total cholesterol values, and the CONUT score could not be calculated for these patients. This may have resulted in a selection bias. Due to the limitations of this retrospective study, a prospective observational study may be necessary for an accurate evaluation. Second, this was a single-center study. To confirm the relationship between the CONUT score and the pathological grading of lung cancer, the results of this study need to be validated in multiple centers.
Conclusions
This study suggests a relationship between the CONUT score and the pathological grading of lung cancer. Patients with a poor nutritional status, as judged by the CONUT score, may be at high risk for recurrence owing to the high frequency of pleural invasion, vascular invasion, and lung metastasis. It is necessary to establish optimal perioperative treatment strategies, including neoadjuvant chemotherapy with molecularly targeted agents and ICIs and to select appropriate surgical techniques for such patients.
Abbreviations
- NSCLC:
-
Non-small cell lung carcinoma
- OS:
-
Overall survival
- DFS:
-
Disease free survival
- PET:
-
Positron emission tomography
- ICI:
-
Immune checkpoint inhibitor
- CONUT:
-
Controlling nutritional status
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- RFS:
-
Recurrence-free survival
- CRR:
-
Cumulative recurrence rate
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
- PSM:
-
Propensity score matching
- PS:
-
Performance status
References
Goldstraw P, Chansky K, Crowley J, Rami-Porta R, Asamura H, Eberhardt WE, et al. The IASLC lung cancer staging project: proposals for revision of the TNM stage groupings in the forthcoming (eighth) edition of the TNM classification for lung cancer. J Thorac Oncol. 2016;11:39–51.
Inoue M, Minami M, Sawabata N, Utsumi T, Kadota Y, Shigemura N, et al. Clinical outcome of resected solid-type small-sized c-stage IA non-small cell lung cancer. Eur J Cardiothorac Surg. 2010;37:1445–9.
Shoji F, Haro A, Yoshida T, Ito K, Morodomi Y, Yano T, et al. Prognostic significance of intratumoral blood vessel invasion in pathologic stage IA non-small cell lung cancer. Ann Thorac Surg. 2010;89:864–9.
Maeda R, Yoshida J, Ishii G, Hishida T, Nishimura M, Nagai K. Risk factors for tumor recurrence in patients with early-stage (stage I and II) non-small cell lung cancer: patient selection criteria for adjuvant chemotherapy according to the seventh edition TNM classification. Chest. 2011;140:1494–502.
Kawachi R, Tsukada H, Nakazato Y, Takei H, Furuyashiki G, Koshi-ishi Y, et al. Early recurrence after surgical resection in patients with pathological stage I non-small cell lung cancer. Thorac Cardiovasc Surg. 2009;57:472–5.
Shiono S, Abiko M, Sato T. Positron emission tomography/computed tomography and lymphovascular invasion predict recurrence in stage I lung cancers. J Thorac Oncol. 2011;6:43–7.
Borghaei H, Gettinger S, Vokes EE, Chow LQM, Burgio MA, de Castro CJ, et al. Five-year outcomes from the randomized, phase III trials CheckMate 017 and 057: nivolumab versus docetaxel in previously treated non-small-cell lung cancer. J Clin Oncol. 2021;39:723–33.
Forde PM, Spicer J, Lu S, Provencio M, Mitsudomi T, Awad MM, et al. Neoadjuvant nivolumab plus chemotherapy in resectable lung cancer. N Engl J Med. 2022;386:1973–85.
Felip E, Altorki N, Zhou C, Csoszi T, Vynnychenko I, Goloborodko O, et al. Adjuvant atezolizumab after adjuvant chemotherapy in resected stage IB-IIIA non-small-cell lung cancer (IMpower010): a randomised, multicentre, open-label, phase 3 trial. Lancet. 2021;398:1344–57.
Shimizu J, Yamazaki S, Sakaguchi S. Induction of tumor immunity by removing CD25+CD4+ T cells: a common basis between tumor immunity and autoimmunity. J Immunol. 1999;163:5211–8.
Onizuka S, Tawara I, Shimizu J, Sakaguchi S, Fujita T, Nakayama E. Tumor rejection by in vivo administration of anti-CD25 (interleukin-2 receptor alpha) monoclonal antibody. Cancer Res. 1999;59:3128–33.
de Ulibarri JI, Gonzalez-Madrono A, de Villar NG, Gonzalez P, Gonzalez B, Mancha A, et al. CONUT: a tool for controlling nutritional status. First validation in a hospital population. Nutr Hosp. 2005;20:38–45.
Toyokawa G, Kozuma Y, Matsubara T, Haratake N, Takamori S, Akamine T, et al. Prognostic impact of controlling nutritional status score in resected lung squamous cell carcinoma. J Thorac Dis. 2017;9:2942–51.
Shoji F, Haratake N, Akamine T, Takamori S, Katsura M, Takada K, et al. The preoperative controlling nutritional status score predicts survival after curative surgery in patients with pathological stage I non-small cell lung cancer. Anticancer Res. 2017;37:741–7.
Akamine T, Toyokawa G, Matsubara T, Kozuma Y, Haratake N, Takamori S, et al. Significance of the preoperative CONUT score in predicting postoperative disease-free and overall survival in patients with lung adenocarcinoma with obstructive lung disease. Anticancer Res. 2017;37:2735–42.
Travis WD, Brambilla E, Burke AP, Marx A, Nicholson AG. WHO classification of tumours of the lung, pleura, thymus and heart. 4th ed. Lyon: International Agency for Research on Cancer Press; 2015. p. 9–152.
Hsieh MC, Rau KM, Chiang PH, Sung MT, Lan J, Luo HL, et al. Impact of prognostic nutritional index on overall survival for patients with metastatic urothelial carcinoma. J Cancer. 2018;9:2466–71.
Feng Z, Wen H, Ju X, Bi R, Chen X, Yang W, et al. The preoperative prognostic nutritional index is a predictive and prognostic factor of high-grade serous ovarian cancer. BMC Cancer. 2018;18:883.
Diem S, Schmid S, Krapf M, Flatz L, Born D, Jochum W, et al. Neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) as prognostic markers in patients with non-small cell lung cancer (NSCLC) treated with nivolumab. Lung Cancer. 2017;111:176–81.
Kuroda D, Sawayama H, Kurashige J, Iwatsuki M, Eto T, Tokunaga R, et al. Controlling Nutritional Status (CONUT) score is a prognostic marker for gastric cancer patients after curative resection. Gastric Cancer. 2018;21:204–12.
Takagi K, Yagi T, Umeda Y, Shinoura S, Yoshida R, Nobuoka D, et al. Preoperative controlling nutritional status (CONUT) score for assessment of prognosis following hepatectomy for hepatocellular carcinoma. World J Surg. 2017;41:2353–60.
Ishihara H, Kondo T, Yoshida K, Omae K, Takagi T, Iizuka J, et al. Preoperative controlling nutritional status (CONUT) score as a novel predictive biomarker of survival in patients with localized urothelial carcinoma of the upper urinary tract treated with radical nephroureterectomy. Urol Oncol. 2017;35(539):e9–16.
Toyokawa T, Kubo N, Tamura T, Sakurai K, Amano R, Tanaka H, et al. The pretreatment controlling nutritional status (CONUT) score is an independent prognostic factor in patients with resectable thoracic esophageal squamous cell carcinoma: results from a retrospective study. BMC Cancer. 2016;16:722.
Shao J, Li J, Zhang XL, Wang G. Prognostic significance of the preoperative controlled nutritional status score in lung cancer patients undergoing surgical resection. Nutr Cancer. 2021;73:2211–8.
Soldati L, Di Renzo L, Jirillo E, Ascierto PA, Marincola FM, De Lorenzo A. The influence of diet on anti-cancer immune responsiveness. J Transl Med. 2018;16:75.
Acknowledgements
We would like to thank Editage (www.editage.com) for editing the English language of this article.
Funding
This study did not receive specific grants from public, commercial, or nonprofit funding agencies.
Author information
Authors and Affiliations
Contributions
Ken Onodera: conceptualization, methodology, investigation, resources, data curation, validation, formal analysis, writing—original draft, and visualization. Hirotsugu Notsuda: resources, writing—review and editing. Tatsuaki Watanabe: resources, writing—review and editing. Yui Watanabe: resources, writing—review and editing. Takaya Suzuki: resources, writing—review, and editing. Takashi Hirama: resources, writing—review and editing. Hisashi Oishi: resources, writing—review, and editing. Hiromichi Niikawa: resources, writing—review and editing. Masafumi Noda: resources, writing—review and editing. Yoshinori Okada: resources, writing—review and editing, supervision, project administration.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest in association with the present study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Onodera, K., Notsuda, H., Watanabe, T. et al. The CONUT score is associated with the pathologic grade in non-small cell lung cancer. Surg Today (2024). https://doi.org/10.1007/s00595-024-02860-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00595-024-02860-8