Abstract
Purpose
Bacteremia occurring after extensive hepatic resection and biliary reconstruction (Hx + Bx) for biliary cancer is a critical infectious complication. This study evaluated postoperative bacteremia and examined the potential usefulness of surveillance cultures.
Methods
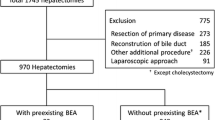
We retrospectively reviewed 179 patients who underwent Hx + Bx for biliary cancer from January 2008 to December 2018 in our department.
Results
Bacteremia occurred in 41 (23.0%) patients. Patients with bacteremia had a longer operation time and more frequent intraoperative transfusion and more frequently developed organ/space surgical site infection (SSI) than those without bacteremia. The most frequently isolated bacterial species from blood cultures were Enterococcus faecium (29.3%), Enterobacter cloacae (24.4%), and Enterococcus faecalis (22.0%). The SIRS duration of bacteremia associated with organ/space SSI was significantly longer than that of other infectious complications (median 96 h vs. 48 h; p = 0.043). Bacteremia associated with organ/space SSI occurred most often by postoperative day (POD) 30. The concordance rate of bacterial species between blood and surveillance cultures within POD 30 was 67–82%.
Conclusions
Bacteremia associated with organ/space SSI required treatment for a long time and typically occurred by POD 30. Postoperative surveillance cultures obtained during this period may be useful for selecting initial antibiotic therapy because of their high concordance rate with blood cultures.


Similar content being viewed by others
Abbreviations
- Hx + Bx:
-
Extensive hepatic resection and biliary reconstruction
- SSI:
-
Surgical site infection
- POD:
-
Postoperative day
- HPB:
-
Hepato-pancreato-biliary
- SIRS:
-
Systemic inflammatory response syndrome
- ISGPF:
-
International Study Group on Pancreatic Fistula Definition
- TG18:
-
Tokyo Guidelines 2018
- PTPE:
-
Percutaneous transhepatic portal vein embolization
- ENBD:
-
Endoscopic naso-biliary drainage
- ERB:
-
Endoscopic retrobiliary drainage
- PTBD:
-
Percutaneous transhepatic biliary drainage
- SSI:
-
Surgical site infection
- MRSA:
-
Methicillin-resistant Staphylococcus aureus
- MRSE:
-
Methicillin-resistant Staphylococcus epidermidis
References
Hirano S, Kondo S, Tanaka E, Shichinohe T, Tsuchikawa T, Kato K, et al. Outcome of surgical treatment of hilar cholangiocarcinoma: a special reference to postoperative morbidity and mortality. J Hepatobiliary Pancreat Sci. 2010;17:455–62.
Nagino M, Ebata T, Yokoyama Y, Igami T, Sugawara G, Takahashi Y, et al. Evolution of surgical treatment for perihilar cholangiocarcinoma: a single-center 34-year review of 574 consecutive resections. Ann Surg. 2013;258:129–40.
Van Gulik T, Kloek J, Ruys A, Busch O, Van Tienhoven G, Lameris J, et al. Multidisciplinary management of hilar cholangiocarcinoma (Klatskin tumor): extended resection is associated with improved survival. Eur J Surg Oncol. 2011;37:65–71.
Young AL, Igami T, Senda Y, Adair R, Farid S, Toogood GJ, et al. Evolution of the surgical management of perihilar cholangiocarcinoma in a Western centre demonstrates improved survival with endoscopic biliary drainage and reduced use of blood transfusion. HPB. 2011;13:483–93.
De Jong MC, Marques H, Clary BM, Bauer TW, Marsh JW, Ribero D, et al. The impact of portal vein resection on outcomes for hilar cholangiocarcinoma: a multi-institutional analysis of 305 cases. Cancer. 2012;118:4737–47.
Neuhaus P, Thelen A, Jonas S, Puhl G, Denecke T, Veltzke-Schlieker W, et al. Oncological superiority of hilar en bloc resection for the treatment of hilar cholangiocarcinoma. Ann Surg Oncol. 2012;19:1602–8.
Shigeta H, Nagino M, Kamiya J, Uesaka K, Sano T, Yamamoto H, et al. Bacteremia after hepatectomy: an analysis of a single-center, 10-year experience with 407 patients. Langenbeck’s Arch Surg. 2002;387:117–24.
Yang PS, Liu CP, Hsu YC, Chen CF, Lee CC, Cheng SP. A novel prediction model for bloodstream infections in hepatobiliary-pancreatic surgery patients. World J Surg. 2019;43:1294–302.
Raman G, Avendano E, Berger S, Menon V. Appropriate initial antibiotic therapy in hospitalized patients with gram-negative infections: systematic review and meta-analysis. BMC Infect Dis. 2015;15:395.
Marquet K, Liesenborgs A, Bergs J, Vleugels A, Claes N. Incidence and outcome of inappropriate in-hospital empiric antibiotics for severe infection: a systematic review and meta-analysis. Crit Care. 2015;19:63.
Kang CI, Kim SH, Park WB, Lee KD, Kim HB, Kim EC, et al. Bloodstream infections caused by antibiotic-resistant gram-negative bacilli: risk factors for mortality and impact of inappropriate initial antimicrobial therapy on outcome. Antimicrob Agents Chemother. 2005;49:760–6.
Ibrahim EH, Sherman G, Ward S, Fraser VJ, Kollef MH. The influence of inadequate antimicrobial treatment of bloodstream infections on patient outcomes in the ICU setting. Chest. 2000;118:146–55.
Noji T, Tanaka K, Matsui A, Nakanishi Y, Asano T, Nakamura T, et al. Transhepatic direct approach to the “limit of the division of the hepatic ducts” leads to a high r0 resection rate in perihilar cholangiocarcinoma. J Gastrointest Surg. 2021;25:2358–67.
Nakanishi Y, Hirano S, Okamura K, Tsuchikawa T, Nakamura T, Noji T, et al. Clinical and oncological benefits of left hepatectomy for Bismuth type I/II perihilar cholangiocarcinoma. Surg Today. 2021. https://doi.org/10.1007/s00595-021-02401-7.
Tamoto E, Hirano S, Tsuchikawa T, Tanaka E, Miyamoto M, Matsumoto J, et al. Portal vein resection using the no-touch technique with a hepatectomy for hilar cholangiocarcinoma. HPB (Oxford). 2014;16:56–61.
Okamura K, Tanaka K, Miura T, Nakanishi Y, Noji T, Nakamura T, et al. Randomized controlled trial of perioperative antimicrobial therapy based on the results of preoperative bile cultures in patients undergoing biliary reconstruction. J Hepatobiliary Pancr Sci. 2017;24:382–93.
Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Chest. 1992;101:1644–55.
Zilberberg MD, Shorr AF, Micek ST, Vazquez-Guillamet C, Kollef MH. Multi-drug resistance, inappropriate initial antibiotic therapy and mortality in Gram-negative severe sepsis and septic shock: a retrospective cohort study. Crit Care. 2014;18:596.
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250:187–96.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;B240:205–13.
Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol. 1999;20:250–78.
Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, et al. The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery. 2017;161:584–91.
Koch M, Garden OJ, Padbury R, Rahbari NN, Adam R, Capussotti L, et al. Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the International Study Group of Liver Surgery. Surgery. 2011;149:680–8.
Kiriyama S, Kozaka K, Takada T, Strasberg SM, Pitt HA, Gabata T, et al. Tokyo Guidelines 2018: diagnostic criteria and severity grading of acute cholangitis (with videos). J Hepatobiliary Pancreat Sci. 2018;25:17–30.
Nagino M, Nishio H, Ebata T, Yokoyama Y, Igami T, Nimura Y. Intrahepatic cholangiojejunostomy following hepatobiliary resection. Br J Surg. 2007;94:70–7.
Nakahira S, Shimizu J, Miyamoto A, Kobayashi S, Umeshita K, Ito T, et al. Proposal for a sub-classification of hepato-biliary-pancreatic operations for surgical site infection surveillance following assessment of results of prospective multicenter data. J Hepatobiliary Pancreat Sci. 2013;20:504–11.
Sakata J, Shirai Y, Tsuchiya Y, Wakai T, Nomura T, Hatakeyama K. Preoperative cholangitis independently increases in-hospital mortality after combined major hepatic and bile duct resection for hilar cholangiocarcinoma. Langenbecks Arch Surg. 2009;394:1065–72.
Nagino M, Kamiya J, Arai T, Nishio H, Ebata T, Nimura Y. One hundred consecutive hepatobiliary resections for biliary hilar malignancy: preoperative blood donation, blood loss, transfusion, and outcome. Surgery. 2005;137:148–55.
Abraham K, Dolman HS, Zimmerman LH, Faris J, Edelman DA, Baylor A, et al. Impact of inappropriate initial antibiotics in critically ill surgical patients with bacteremia. Am J Surg. 2016;211:593–8.
Davies SW, Efird JT, Guidry CA, Hranjec T, Metzger R, Swenson BR, et al. Does it matter if we get it right? Impact of appropriateness of empiric antimicrobial therapy among surgical patients. Shock. 2014;42:185–91.
Sugawara G, Ebata T, Yokoyama Y, Igami T, Takahashi Y, Takara D, et al. The effect of preoperative biliary drainage on infectious complications after hepatobiliary resection with cholangiojejunostomy. Surgery. 2013;153:200–10.
Acknowledgements
We would like to thank Editage (www.editage.com) for the English language editing. No financial support was received for this study.
Author information
Authors and Affiliations
Contributions
Study conception and design, analysis and interpretation of data and drafting of manuscript: JF and KT. Acquisition of data; JF, KT, YN, TN, and KO. All authors discussed or revised the manuscript and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Fukuda, J., Tanaka, K., Matsui, A. et al. Bacteremia after hepatectomy and biliary reconstruction for biliary cancer: the characteristics of bacteremia according to occurrence time and associated complications. Surg Today 52, 1373–1381 (2022). https://doi.org/10.1007/s00595-022-02462-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-022-02462-2