Abstract
Purposes
The relationship between the results of bacterial drainage fluid cultures in the early postoperative period after liver resection and the development of surgical site infections (SSIs) is unclear. We evaluated the diagnostic value of bacterial cultures of drainage fluid obtained on postoperative day (POD) 1 after liver resection.
Methods
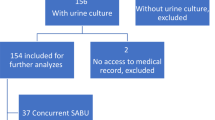
The cases of all consecutive patients who underwent elective liver resection from January 2014 to December 2016 were analyzed. The association between a positive culture result and the development of SSIs was analyzed.
Results
A total of 195 consecutive patients were studied. Positive drainage fluid cultures were obtained in 6 patients (3.1%). A multivariate analysis revealed that a positive drainage fluid culture was an independent risk factor for SSIs (odds ratio: 8.04, P = 0.035), and combined resection of the gastrointestinal tract was a risk factor for a positive drainage fluid culture (P = 0.006). Among the patients who did not undergo procedures involving the gastrointestinal tract, there was no association between drainage fluid culture positivity and SSIs.
Conclusions
The detection of positive culture results for drainage fluid collected on POD 1 after liver resection was associated with SSIs. However, among patients who did not undergo procedures involving the gastrointestinal tract, it was not a predictor of SSIs.
Similar content being viewed by others
References
Wu CC, Yeh DC, Lin MC, Liu TJ, P’Eng FK. Improving operative safety for cirrhotic liver resection. Br J Surg. 2001;88(2):210–15 (PubMed PMID: 11167869. Epub 2001/02/13. eng).
Ciria R, Cherqui D, Geller DA, Briceno J, Wakabayashi G. Comparative Short-term Benefits of Laparoscopic Liver Resection: 9000 Cases and Climbing. Ann Surg. 2016;263(4):761–77 (PubMed PMID: 26700223. Epub 2015/12/25. eng).
Kokudo T, Uldry E, Demartines N, Halkic N. Risk factors for incisional and organ space surgical site infections after liver resection are different. World J Surg. 2015;39(5):1185–92 (PubMed PMID: 25561190. Epub 2015/01/07. eng).
Sadamori H, Yagi T, Shinoura S, Umeda Y, Yoshida R, Satoh D, et al. Risk factors for organ/space surgical site infection after hepatectomy for hepatocellular carcinoma in 359 recent cases. J Hepatobiliary Pancreat Sci. 2013;20(2):186–96 (PubMed PMID: 22273719. Epub 2012/01/26. eng).
Rahbari NN, Elbers H, Koch M, Kirchberg J, Dutlu M, Mehrabi A, et al. Bilirubin level in the drainage fluid is an early and independent predictor of clinically relevant bile leakage after hepatic resection. Surgery. 2012;152(5):821–31 (PubMed PMID: 22657729. Epub 2012/06/05. eng).
Sun HC, Qin LX, Lu L, Wang L, Ye QH, Ren N, et al. Randomized clinical trial of the effects of abdominal drainage after elective hepatectomy using the crushing clamp method. Br J Surg. 2006;93(4):422–6 (PubMed PMID: 16491462. Epub 2006/02/24. eng).
Liu CL, Fan ST, Lo CM, Wong Y, Ng IO, Lam CM, et al. Abdominal drainage after hepatic resection is contraindicated in patients with chronic liver diseases. Ann Surg. 2004;239(2):194–201 (PubMed PMID: 14745327. Pubmed Central PMCID: PMC1356212. Epub 2004/01/28. eng).
Squires MH 3rd, Lad NL, Fisher SB, Kooby DA, Weber SM, Brinkman A, et al. Value of primary operative drain placement after major hepatectomy: a multi-institutional analysis of 1,041 patients. J Am Coll Surg. 2015;220(4):396–402 (PubMed PMID: 25724607. Epub 2015/03/01. eng).
Kyoden Y, Imamura H, Sano K, Beck Y, Sugawara Y, Kokudo N, et al. Value of prophylactic abdominal drainage in 1269 consecutive cases of elective liver resection. J Hepatobiliary Pancreat Sci. 2010;17(2):186–92 (PubMed PMID: 19727544. Epub 2009/09/04. eng).
Tanaka K, Kumamoto T, Nojiri K, Takeda K, Endo I. The effectiveness and appropriate management of abdominal drains in patients undergoing elective liver resection: a retrospective analysis and prospective case series. Surg Today. 2013;43(4):372–80 (PubMed PMID: 22797963. Epub 2012/07/17. eng).
Yamazaki S, Takayama T, Moriguchi M, Mitsuka Y, Okada S, Midorikawa Y, et al. Criteria for drain removal following liver resection. Br J Surg. 2012;99(11):1584–90 (PubMed PMID: 23027077. Epub 2012/10/03. eng).
Hokuto D, Nomi T, Yasuda S, Kawaguchi C, Yoshikawa T, Ishioka K, et al. The safety of the early removal of prophylactic drainage after liver resection based solely on predetermined criteria: a propensity score analysis. HPB (Oxf). 2017;19(4):359–64 (PubMed PMID: 28117230. Epub 2017/01/25. eng).
Migita K, Takayama T, Matsumoto S, Wakatsuki K, Tanaka T, Ito M, et al. Impact of bacterial culture positivity of the drainage fluid during the early postoperative period on the development of intra-abdominal abscesses after gastrectomy. Surg Today. 2014;44(11):2138–45 (PubMed PMID: 24633956. Epub 2014/03/19. eng).
Sugiura T, Mizuno T, Okamura Y, Ito T, Yamamoto Y, Kawamura I, et al. Impact of bacterial contamination of the abdominal cavity during pancreaticoduodenectomy on surgical-site infection. Br J Surg. 2015;102(12):1561–6 (PubMed PMID: 26206386. Epub 2015/07/25. eng).
Hokuto D, Nomi T, Kawaguchi C, Yoshikawa T, Yasuda S, Obara S, et al. The administration of celecoxib as an analgesic after liver resection is safe. Dig Surg. 2017;34(2):108–13 (PubMed PMID: 27640209. Epub 2016/09/19. eng).
Hokuto D, Nomi T, Yamato I, Yasuda S, Obara S, Nakajima Y. Impact of mechanical bowel preparation on postoperative outcomes after liver resection for patients with hepatocellular carcinoma: a single-center retrospective cohort study. Dig Surg. 2016;33(1):51–7 (PubMed PMID: 26587899. Epub 2015/11/21. eng).
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13 (PubMed PMID: 15273542. Pubmed Central PMCID: PMC1360123. Epub 2004/07/27. eng).
Koch M, Garden OJ, Padbury R, Rahbari NN, Adam R, Capussotti L, et al. Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the International Study Group of Liver Surgery. Surgery. 2011;149(5):680–8 (PubMed PMID: 21316725. Epub 2011/02/15. eng).
Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for prevention of surgical site infection, 1999. Hospital infection control practices advisory committee. Infect Control Hosp Epidemiol. 1999;20(4):250–78 (quiz 79–80. PubMed PMID: 10219875. Epub 1999/04/29. eng).
Rahbari NN, Garden OJ, Padbury R, Brooke-Smith M, Crawford M, Adam R, et al. Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery. 2011;149(5):713–24 (PubMed PMID: 21236455. Epub 2011/01/18. eng).
Yamada T, Yoshii T, Egawa S, Takada R, Hirai T, Inose H, et al. Drain tip culture is not prognostic for surgical site infection in spinal surgery under prophylactic use of antibiotics. Spine (Phila Pa 1976). 2016;41(14):1179–84 (PubMed PMID: 26890956. Epub 2016/02/19. eng).
Kobayashi K, Imagama S, Ito Z, Ando K, Yagi H, Hida T, et al. Is a drain tip culture required after spinal surgery? Clin Spine Surg. 2016;30(8):356–9.
Takada R, Jinno T, Koga D, Hirao M, Muneta T, Okawa A. Is drain tip culture prognostic of surgical site infection? Results of 1380 drain tip cultures in total hip arthroplasty. J Arthroplasty. 2015;30(8):1407–9 (PubMed PMID: 25770862. Epub 2015/03/17. eng).
Silberhumer GR, Paty PB, Temple LK, Araujo RL, Denton B, Gonen M, et al. Simultaneous resection for rectal cancer with synchronous liver metastasis is a safe procedure. Am J Surg. 2015;209(6):935–42 (PubMed PMID: 25601556. Pubmed Central PMCID: PMC4603659. Epub 2015/01/21. eng).
Mayo SC, Pulitano C, Marques H, Lamelas J, Wolfgang CL, de Saussure W, et al. Surgical management of patients with synchronous colorectal liver metastasis: a multicenter international analysis. J Am Coll Surg. 2013;216(4):707–16 (discussion 16–8. PubMed PMID: 23433970. Pubmed Central PMCID: PMC3994665. Epub 2013/02/26. eng).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
KI, DH, TN, SY, TY, YM, TA, KN, MN, KN, NI, and MS have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Ishioka, K., Hokuto, D., Nomi, T. et al. Significance of bacterial culturing of prophylactic drainage fluid in the early postoperative period after liver resection for predicting the development of surgical site infections. Surg Today 48, 625–631 (2018). https://doi.org/10.1007/s00595-018-1629-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-018-1629-8