Abstract
Purpose
Gadoxetic acid-enhanced MRI (Gd-EOB-MRI) shows higher sensitivity for colorectal liver metastases (CRLM) than contrast-enhanced computed tomography (CECT). However, the details of false-positive lesions for each imaging modality are unknown.
Methods
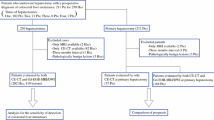
Cases undergoing hepatectomy for CRLM following a preoperative evaluation with both CECT and Gd-EOB-MRI between July 2008 and December 2016 were reviewed. The false-positive and false-negative rates were assessed for each modality, and the characteristics of false-positive lesions were evaluated.
Results
We evaluated 275 partial hepatectomies in 242 patients without preoperative chemotherapy. Among the 275 hepatectomies, 546 lesions were recognized by CECT and/or Gd-EOB-MRI. The false-positive rates for CECT and Gd-EOB-MRI were 4% (18/422) and 7% (37/536), respectively. The size of false-positive lesions was significantly smaller than that of correctly diagnosed lesions (median: 28 mm [3–120 mm] vs 7.6 mm [320 mm], P < 0.001). Compared with the 233 correctly diagnosed lesions ≤ 20 mm in diameter, false-positive lesions were more frequently located near the liver surface or vasculobiliary structures than true lesions (33/37 [89%] vs 149/233 [64%], respectively; P = 0.0021).
Conclusion
Gd-EOB-MRI had a 7% false-positive rate. A small size and tumor location near the surface or near vasculobiliary structures were associated with false positivity.




Similar content being viewed by others
References
Albrecht MH, Wichmann JL, Müller C, Schreckenbach T, Sakthibalan S, Hammerstingl R, et al. Assessment of colorectal liver metastases using MRI and CT: impact of observer experience on diagnostic performance and inter-observer reproducibility with histopathological correlation. Eur J Radiol. 2014;83:1752–8.
Kim HJ, Lee SS, Byun JH, Kim JC, Yu CS, Park SH, et al. Incremental value of liver MR imaging in patients with potentially curable colorectal hepatic metastasis detected at CT: a prospective comparison of diffusion-weighted imaging, gadoxetic acid-enhanced MR imaging, and a combination of both MR techniques. Radiology. 2015;274:712–22.
Kim YK, Park G, Kim CS, Yu HC, Han YM. Diagnostic efficacy of gadoxetic acid-enhanced MRI for the detection and characterisation of liver metastases: comparison with multidetector-row CT. Br J Radiol. 2012;85:539–47.
Sofue K, Tsurusaki M, Murakami T, Onoe S, Tokue H, Shibamoto K, et al. Does gadoxetic acid-enhanced 3.0T MRI in addition to 64-detector-row contrast-enhanced CT provide better diagnostic performance and change the therapeutic strategy for the preoperative evaluation of colorectal liver metastases? Eur Radiol. 2014;24:2532–9.
Colagrande S, Castellani A, Nardi C, Lorini C, Calistri L, Filippone A. The role of diffusion-weighted imaging in the detection of hepatic metastases from colorectal cancer: a comparison with unenhanced and Gd-EOB-DTPA enhanced MRI. Eur J Radiol. 2016;85:1027–34.
Granata V, Fusco R, de Lutio di Castelguidone E, Avallone A, Palaia R, Delrio P, et al. Diagnostic performance of gadoxetic acid-enhanced liver MRI versus multidetector CT in the assessment of colorectal liver metastases compared to hepatic resection. BMC Gastroenterol. 2019;19(1):129.
Tanaka M, Kishi Y, Esaki M, Nara S, Miyake M, Hiraoka N, et al. Feasibility of routine application of gadoxetic acid-enhanced MRI in combination with diffusion-weighted MRI for the preoperative evaluation of colorectal liver metastases. Ann Surg Oncol. 2016;23:3991–8.
Ba-Ssalamah A, Uffmann M, Saini S, Bastati N, Herold C, Schima W. Clinical value of MRI liver-specific contrast agents: a tailored examination for a confident non-invasive diagnosis of focal liver lesions. Eur Radiol. 2009;19:342–57.
Koh DM, Scurr E, Collins DJ, Pirgon A, Kanber B, Karanjia N, et al. Colorectal hepatic metastases: quantitative measurements using single-shot echo-planar diffusion-weighted MR imaging. Eur Radiol. 2006;16:1898–905.
Taouli B, Koh DM. Diffusion-weighted MR imaging of the liver. Radiology. 2010;254:47–66.
Arita J, Ono Y, Takahashi M, Inoue Y, Takahashi Y, Matsueda K, et al. Routine preoperative liver-specific magnetic resonance imaging does not exclude the necessity of contrast-enhanced intraoperative ultrasound in hepatic resection for colorectal liver metastasis. Ann Surg. 2015;262:1086–91.
Leen E, Ceccotti P, Moug SJ, Glen P, MacQuarrie J, Angerson WJ, et al. Potential value of contrast-enhanced intraoperative ultrasonography during partial hepatectomy for metastases: an essential investigation before resection? Ann Surg. 2006;243:236–40.
Yamamoto J, Sugihara K, Kosuge T, Takayama T, Shimada K, Yamasaki S, et al. Pathologic support for limited hepatectomy in the treatment of liver metastases from colorectal cancer. Ann Surg. 1995;221:74–8.
Asato N, Tsurusaki M, Sofue K, Hieda Y, Katsube T, Kitajima K, et al. Comparison of gadoxetic acid-enhanced dynamic MR imaging and contrast-enhanced computed tomography for preoperative evaluation of colorectal liver metastases. Jpn J Radiol. 2017;35:197–205.
Muhi A, Ichikawa T, Motosugi U, Sou H, Nakajima H, Sano K, et al. Diagnosis of colorectal hepatic metastases: comparison of contrast-enhanced CT, contrast-enhanced US, superparamagnetic iron oxide-enhanced MRI, and gadoxetic acid-enhanced MRI. J Magn Reson Imaging. 2011;34:326–35.
Scharitzer M, Ba-Ssalamah A, Ringl H, Kölblinger C, Grünberger T, Weber M, et al. Preoperative evaluation of colorectal liver metastases: comparison between gadoxetic acid-enhanced 3.0-T MRI and contrast-enhanced MDCT with histopathological correlation. Eur Radiol. 2013;23:2187–96.
Sivesgaard K, Larsen LP, Sørensen M, Kramer S, Schlander S, Amanavicius N, et al. Diagnostic accuracy of CE-CT, MRI and FDG PET/CT for detecting colorectal cancer liver metastases in patients considered eligible for hepatic resection and/or local ablation. Eur Radiol. 2018;28:4735–47.
Nordlinger B, Guiguet M, Vaillant JC, Balladur P, Boudjema K, Bachellier P, Association Française de Chirurgie, et al. Surgical resection of colorectal carcinoma metastases to the liver. A prognostic scoring system to improve case selection, based on 1568 patients. Cancer. 1996;77:1254–62.
Fong Y, Fortner J, Sun RL, Brennan MF, Blumgart LH. Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg. 1999;230:309–18 (discussion 18–21).
Nagashima I, Takada T, Matsuda K, Adachi M, Nagawa H, Muto T, et al. A new scoring system to classify patients with colorectal liver metastases: proposal of criteria to select candidates for hepatic resection. J Hepatobiliary Pancreat Surg. 2004;11:79–83.
Beppu T, Sakamoto Y, Hasegawa K, Honda G, Tanaka K, Kotera Y, et al. A nomogram predicting disease-free survival in patients with colorectal liver metastases treated with hepatic resection: multicenter data collection as a Project Study for Hepatic Surgery of the Japanese Society of Hepato-Biliary-Pancreatic Surgery. J Hepatobiliary Pancreat Sci. 2012;19:72–84.
Jhaveri KS, Fischer SE, Hosseini-Nik H, Sreeharsha B, Menezes RJ, Gallinger S, et al. Prospective comparison of gadoxetic acid-enhanced liver MRI and contrast-enhanced CT with histopathological correlation for preoperative detection of colorectal liver metastases following chemotherapy and potential impact on surgical plan. HPB (Oxford). 2017;19:992–1000.
Acknowledgements
We thank LC, MD, MA, and JC, DVM, from Edanz (https://jp.edanz.com/ac) for editing drafts of this manuscript and AK from the Division of Biostatistics, National Cancer Center, Japan, for giving advice regarding the statistical analyses.
Funding
This work was supported by the Practical Research for Innovative Cancer Control (No. 16ck0106211s0101) from the Japan Agency for Medical Research and Development (AMED).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yamada, S., Kishi, Y., Miyake, M. et al. Characteristics of false-positive lesions in evaluating colorectal liver metastases on gadoxetic acid-enhanced magnetic resonance imaging. Surg Today 52, 1178–1184 (2022). https://doi.org/10.1007/s00595-022-02451-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-022-02451-5