Abstract
Purpose
The aim of this study was to elucidate the association between pancreatic fistula (PF) and the sequential changes in the perioperative exocrine function after pancreatectomy.
Methods
The subjects were 96 patients who underwent a 13C-trioctanoin breath test before and 1 month after pancreatectomy, between 2006 and 2018. We retrospectively compared the pre- and postoperative fat absorption levels between patients with PF (PF group; n = 17) and without PF (non-PF group; n = 79) using the breath test.
Results
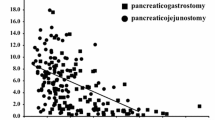
The preoperative level of 13C-trioctanoin absorption (%dose/h) was comparable between the non-PF and PF groups (36.5 vs. 36.9). In the non-PF group, 13C-trioctanoin absorption was significantly decreased after surgery in comparison to the preoperative setting (post-operative 28.5; pre-operative 36.5; p < 0.0001), whereas these values were comparable (post-operative 36.9; pre-operative 34.5; p = 0.129) in the PF group. Moreover, postoperative absorption in the PF group was significantly better than that in the non-PF group (34.5 vs. 28.5%, p = 0.0003). The maximum drain amylase level was significantly higher in patients with a 13C-trioctanoin absorption level (%dose/h) of ≥ 30 in comparison to patients with levels of < 30 (2502 vs. 398 U/L, p = 0.001).
Conclusion
PF did not exacerbate the pancreatic exocrine function in the early postoperative period, and the acceleration or preservation of the exocrine function after surgery may be an important cause of PF.



Similar content being viewed by others
Data availability
All the data generated or analyzed during this study are included within the article.
References
Kawai M, Kondo S, Yamaue H, Wada K, Sano K, Motoi F, et al. Predictive risk factors for clinically relevant pancreatic fistula analyzed in 1239 patients with pancreaticoduodenectomy: multicenter data collection as a project study of pancreatic surgery by the Japanese Society of Hepato-Biliary-Pancreatic Surgery. J Hepatobiliary Pancreat Sci. 2011;18(4):601–8.
Kusafuka T, Kato H, Iizawa Y, Noguchi D, Gyoten K, Hayasaki A, et al. Pancreas-visceral fat CT value ratio and serrated pancreatic contour are strong predictors of postoperative pancreatic fistula after pancreaticojejunostomy. BMC Surg. 2020;20(1):129.
Sugimoto M, Takahashi S, Kojima M, Kobayashi T, Gotohda N, Konishi M. In patients with a soft pancreas, a thick parenchyma, a small duct, and fatty infiltration are significant risks for pancreatic fistula after pancreaticoduodenectomy. J Gastrointest Surg. 2017;21(5):846–54.
Yasuda H, Takada T, Toyota N, Amano H, Yoshida M, Takada Y, et al. Limited pancreatectomy: significance of postoperative maintenance of pancreatic exocrine function. J Hepatobiliary Pancreat Surg. 2000;7(5):466–72.
Horiguchi A, Miyakawa S, Ishihara S, Ito M, Asano Y, Furusawa K, et al. Surgical design and outcome of duodenum-preserving pancreatic head resection for benign or low-grade malignant tumors. J Hepatobiliary Pancreat Sci. 2010;17(6):792–7.
Ito K. Duodenum preservation in pancreatic head resection to maintain pancreatic exocrine function (determined by pancreatic function diagnostant test and cholecystokinin secretion). J Hepatobiliary Pancreat Surg. 2005;12(2):123–8.
Yamaguchi K, Yokohata K, Nakano K, Ohtani K, Ogawa Y, Chijiiwa K, et al. Which is a less invasive pancreatic head resection: PD, PPPD, or DPPHR? Dig Dis Sci. 2001;46(2):282–8.
Kato H, Nakao A, Kishimoto W, Nonami T, Harada A, Hayakawa T, et al. 13C-labeled trioctanoin breath test for exocrine pancreatic function test in patients after pancreatoduodenectomy. Am J Gastroenterol. 1993;88(1):64–9.
Giuliani T, Andrianello S, Bortolato C, Marchegiani G, De Marchi G, Malleo G, et al. Preoperative fecal elastase-1 (FE-1) adds value in predicting post-operative pancreatic fistula: not all soft pancreas share the same risk—a prospective analysis on 105 patients. HPB (Oxford). 2020;22(3):415–21.
Wali PD, Loveridge-Lenza B, He Z, Horvath K. Comparison of fecal elastase-1 and pancreatic function testing in children. J Pediatr Gastroenterol Nutr. 2012;54(2):277–80.
Kang JH, Park JS, Yu JS, Chung JJ, Kim JH, Cho ES, et al. Prediction of pancreatic fistula after pancreatoduodenectomy by preoperative dynamic CT and fecal elastase-1 levels. PLoS ONE. 2017;12(5):e0177052.
Hirono S, Murakami Y, Tani M, Kawai M, Okada K, Uemura K, et al. Identification of risk factors for pancreatic exocrine insufficiency after pancreaticoduodenectomy using a 13C-labeled mixed triglyceride breath test. World J Surg. 2015;39(2):516–25.
Bassi C, Marchegiani G, Dervenis C, Sarr M, Hilal MA, Adham M, et al. The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery. 2017;161(3):584–91.
Miyakawa S, Hayakawa M, Horiguchi A, Mizuno K, Ishihara S, Niwamoto N, et al. Estimation of fat absorption with the 13C-trioctanoin breath test after pancreatoduodenectomy or pancreatic head resection. World J Surg. 1996;20(8):1024–8 (discussion 8-9).
Miyakawa S, Niwamoto N, Horiguchi A, Hanai T, Mizuno K, Ishihara S, et al. Fat absorption after pylorus-preserving pancreatoduodenectomy reconstructed with Billroth II pancreaticojejunostomy or Billroth I pancreaticogastrostomy. Hepatogastroenterology. 2000;47(31):264–8.
Mews P, Phillips P, Fahmy R, Korsten M, Pirola R, Wilson J, et al. Pancreatic stellate cells respond to inflammatory cytokines: potential role in chronic pancreatitis. Gut. 2002;50(4):535–41.
Roshani R, McCarthy F, Hagemann T. Inflammatory cytokines in human pancreatic cancer. Cancer Lett. 2014;345(2):157–63.
Hirono S, Kawai M, Okada KI, Miyazawa M, Kitahata Y, Hayami S, et al. Modified Blumgart mattress suture versus conventional interrupted suture in pancreaticojejunostomy during pancreaticoduodenectomy: randomized controlled trial. Ann Surg. 2019;269(2):243–51.
Satoi S, Yamamoto T, Yanagimoto H, Yamaki S, Kosaka H, Hirooka S, et al. Does modified Blumgart anastomosis without intra-pancreatic ductal stenting reduce post-operative pancreatic fistula after pancreaticojejunostomy? Asian J Surg. 2019;42(1):343–9.
Fujii T, Yamada S, Murotani K, Sugimoto H, Hattori M, Kanda M, et al. Modified Blumgart suturing technique for remnant closure after distal pancreatectomy: a propensity score-matched analysis. J Gastrointest Surg. 2016;20(2):374–84.
Fujii T, Sugimoto H, Yamada S, Kanda M, Suenaga M, Takami H, et al. Modified Blumgart anastomosis for pancreaticojejunostomy: technical improvement in matched historical control study. J Gastrointest Surg. 2014;18(6):1108–15.
Wallace CL, Georgakis GV, Eisenberg DP, Macaulay WP, Jimenez RE. Further experience with pancreatic stump closure using a reinforced staple line. Conn Med. 2013;77(4):205–10.
Ferrone CR, Warshaw AL, Rattner DW, Berger D, Zheng H, Rawal B, et al. Pancreatic fistula rates after 462 distal pancreatectomies: staplers do not decrease fistula rates. J Gastrointest Surg. 2008;12(10):1691–7 (discussion 7-8).
Azumi Y, Isaji S, Kato H, Nobuoka Y, Kuriyama N, Kishiwada M, et al. A standardized technique for safe pancreaticojejunostomy: pair-watch suturing technique. World J Gastrointest Surg. 2010;2(8):260–4.
Azumi Y, Isaji S. Stented pancreaticojejunostomy (with video). J Hepatobiliary Pancreat Sci. 2012;19(2):116–24.
Maemura K, Mataki Y, Kurahara H, Tanoue K, Kawasaki Y, Ijichi T, et al. The 1-year outcomes after pancreaticogastrostomy using vertical versus horizontal mattress suturing for gastric wrapping. Surg Today. 2020;51:511–9.
Eguchi H, Iwagami Y, Matsushita K, Tomimaru Y, Akita H, Noda T, et al. Randomized clinical trial of pancreaticogastrostomy versus pancreaticojejunostomy regarding incidence of delayed gastric emptying after pancreaticoduodenectomy. Langenbecks Arch Surg. 2020;405(7):921–8.
Kawai M, Yamaue H, Jang J-Y, Uesaka K, Unno M, Nakamura M, et al. Propensity score-matched analysis of internal stent vs external stent for pancreatojejunostomy during pancreaticoduodenectomy: Japanese-Korean cooperative project. Pancreatology. 2020;20(5):984–91.
Tani M, Kawai M, Hirono S, Ina S, Miyazawa M, Shimizu A, et al. A prospective randomized controlled trial of internal versus external drainage with pancreaticojejunostomy for pancreaticoduodenectomy. Am J Surg. 2010;199(6):759–64.
Casadei R, Ricci C, Ingaldi C, Alberici L, De Raffele E, Minni F. Comparison of Blumgart anastomosis with duct-to-mucosa anastomosis and invagination pancreaticojejunostomy after pancreaticoduodenectomy: a single-center propensity score matching analysis. J Gastrointest Surg. 2020;25:411–20.
Schrempf M, Anthuber M. Pancreaticojejunostomy: duct-to-mucosa anastomosis or invagination anastomosis? Chirurg. 2019;90:68 (Suppl 2).
Lyu Y, Li T, Wang B, Cheng Y, Zhao S. Selection of pancreaticojejunostomy technique after pancreaticoduodenectomy: duct-to-mucosa anastomosis is not better than invagination anastomosis: a meta-analysis. Medicine (Baltimore). 2018;97(40):e12621.
Van Buren G, Vollmer CM. The landmark series: mitigation of the postoperative pancreatic fistula. Ann Surg Oncol. 2020;28:1052–9.
Williams ST, Woltering EA, O’Dorisio TM, Fletcher WS. Effect of octreotide acetate on pancreatic exocrine function. Am J Surg. 1989;157(5):459–62.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Takahiko Higashiguchi and the other co-authors declare no conflicts of interest in association with the present study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Higashiguchi, T., Kato, H., Yasuoka, H. et al. A preserved pancreatic exocrine function after pancreatectomy may be a crucial cause of pancreatic fistula: paradoxical results of the 13C-trioctanoin breath test in the perioperative period. Surg Today 52, 580–586 (2022). https://doi.org/10.1007/s00595-021-02371-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-021-02371-w