Abstract
Purpose
The perforation of the upper gastrointestinal tract is still associated with a high risk of complications and mortality. We aimed to evaluate the optimal treatment and post-treatment complications for this condition.
Methods
This was a retrospective, single-center study conducted between 2010 and 2019. We analyzed 50 patients with intraperitoneal free air caused by peptic ulcer (44 cases) or cancer (six cases).
Results
All patients initially received either conservative therapy (n = 7) or surgery (n = 43). The nonsurgically cured patients were significantly younger and had mild peritonitis and also had a shorter hospital stay. Two patients were converted to surgery due to worsening symptoms, and one of them was elderly and had a long perforation-to-treatment time. Regarding postoperative complications, patients with Grade II–V (n = 21) were significantly older and had a poorer physical status, longer perforation-to-surgery time, and higher preoperative CRP and lactate than those with Grade 0–I (n = 24). Multivariable analyses identified elevated preoperative lactate as an independent risk factor for postoperative complications. The patients with noncurative surgery for perforated advanced gastric cancer all died within 1 year after surgery.
Conclusions
Consideration should be given to the nonsurgical indications in elderly and delayed treatment patients and the postoperative outcomes of patients with preoperatively elevated lactate levels.

Similar content being viewed by others
References
Lanas A, Chan FKL. Peptic ulcer disease. Lancet. 2017;390:613–24.
Søreide K, Thorsen K, Harrison EM, Bingener J, Møller MH, Ohene-Yeboah M, et al. Perforated peptic ulcer. Lancet. 2015;386:1288–98.
Møller MH, Adamsen S, Thomsen RW, Møller AM, Peptic Ulcer Perforation (PULP) trial group. Multicentre trial of a perioperative protocol to reduce mortality in patients with peptic ulcer perforation. Br J Surg. 2011;98:802–10.
Ignjatovic N, Stojanov D, Djordjevic M, Ignjatovic J, Benedeto Stojanov D, Milojkovic B. Perforation of gastric cancer—What should the surgeon do? Bosn J Basic Med Sci. 2016;16:222–6.
Søreide K, Thorsen K, Søreide JA. Strategies to improve the outcome of emergency surgery for perforated peptic ulcer. Br J Surg. 2014;101:e51–64.
Thorsen K, Glomsaker TB, von Meer A, Søreide K, Søreide JA. Trends in diagnosis and surgical management of patients with perforated peptic ulcer. J Gastrointest Surg. 2011;15:1329–35.
Suriya C, Kasatpibal N, Kunaviktikul W, Kayee T. Diagnostic indicators for peptic ulcer perforation at a tertiary care hospital in Thailand. Clin Exp Gastroenterol. 2011;4:283–9.
Lim CH, Vani D, Shah SG, Everett SM, Rembacken BJ. The outcome of suspected upper gastrointestinal bleeding with 24-hour access to upper gastrointestinal endoscopy: a prospective cohort study. Endoscopy. 2006;38:581–5.
Bertleff MJ, Lange JF. Perforated peptic ulcer disease: a review of history and treatment. Dig Surg. 2010;27:161–9.
Grassi R, Romano S, Pinto A, Romano L. Gastro-duodenal perforations: conventional plain film, US and CT findings in 166 consecutive patients. Eur J Radiol. 2004;50:30–6.
Tarasconi A, Coccolini F, Biffl WL, Tomasoni M, Ansaloni L, Picetti E, et al. Perforated and bleeding peptic ulcer: WSES guidelines. World J Emerg Surg. 2020;15:3.
Satoh K, Yoshino J, Akamatsu T, Itoh T, Kato M, Kamada T, et al. Evidence-based clinical practice guidelines for peptic ulcer disease 2015. J Gastroenterol. 2016;51:177–94.
Guyatt GH, Oxman AD, Kunz R, Falck-Ytter Y, Vist GE, Liberati A, et al. Going from evidence to recommendations. BMJ. 2008;336:1049–51.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–6.
Chung KT, Shelat VG. Perforated peptic ulcer - an update. World J Gastrointest Surg. 2017;9:1–12.
Crofts TJ, Park KG, Steele RJ, Chung SS, Li AK. A randomized trial of nonoperative treatment for perforated peptic ulcer. N Engl J Med. 1989;320:970–3.
Buck DL, Vester-Andersen M, Møller MH, Danish Clinical Register of Emergency Surgery. Surgical delay is a critical determinant of survival in perforated peptic ulcer. Br J Surg. 2013;100:1045–9.
Møller MH, Adamsen S, Thomsen RW, Møller AM. Preoperative prognostic factors for mortality in peptic ulcer perforation: a systematic review. Scand J Gastroenterol. 2010;45:785–805.
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315:801–10.
Roviello F, Rossi S, Marrelli D, De Manzoni G, Pedrazzani C, Morgagni P, et al. Perforated gastric carcinoma: a report of 10 cases and review of the literature. World J Surg Oncol. 2006;4:19.
Jwo SC, Chien RN, Chao TC, Chen HY, Lin CY. Clinicopathological features, surgical management, and disease outcome of perforated gastric cancer. J Surg Oncol. 2005;15(91):219–25.
Kotan C, Sumer A, Baser M, Kızıltan R, Carparlar MA. An analysis of 13 patients with perforated gastric carcinoma: a surgeon’s nightmare? World J Emerg Surg. 2008;3:17.
Tsujimoto H, Hiraki S, Sakamoto N, Yaguchi Y, Horio T, Kumano I. Outcome after emergency surgery in patients with a free perforation caused by gastric cancer. Exp Ther Med. 2010;1:199–203.
Kandel BP, Singh Y, Singh KP, Khakurel M. Gastric cancer perforation: experience from a tertiary care hospital. JNMA J Nepal Med Assoc. 2013;52:489–93.
Vărcuş F, Beuran M, Lica I, Turculet C, Cotarlet AV, Georgescu S. Laparoscopic repair for perforated peptic ulcer: a retrospective study. World J Surg. 2017;41:948–53.
Lo HC, Wu SC, Huang HC, Yeh CC, Huang JC, Hsieh CH. Laparoscopic simple closure alone is adequate for low risk patients with perforated peptic ulcer. World J Surg. 2011;35:1873–8.
Ates M, Sevil S, Bakircioglu E, Colak C. Laparoscopic repair of peptic ulcer perforation without omental patch versus conventional open repair. J Laparoendosc Adv Surg Tech A. 2007;17:615–9.
Gupta S, Kaushik R, Sharma R, Attri A. The management of large perforations of duodenal ulcers. BMC Surg. 2005;5:15.
Siow SL, Mahendran HA. Laparoscopic repair of perforated peptic ulcers: the sutured omental patch and focused sequential lavage technique. Surg Laparosc Endosc Percutan Tech. 2014;24:134–9.
Cirocchi R, Soreide K, Di Saverio S, Rossi E, Arezzo A, Zago M. Meta-analysis of perioperative outcomes of acute laparoscopic versus open repair of perforated gastroduodenal ulcers. J Trauma Acute Care Surg. 2018;85:417–25.
Bergström M, Arroyo Vázquez JA, Park PO. Self-expandable metal stents as a new treatment option for perforated duodenal ulcer. Endoscopy. 2013;45:222–5.
Alvarado-Aparicio HA, Moreno-Portillo M. Multimedia article: management of duodenal ulcer perforation with combined laparoscopic and endoscopic methods. Surg Endosc. 2004;18:1394.
Malhotra AK, Fabian TC, Katsis SB, Gavant ML, Croce MA. Blunt bowel and mesenteric injuries: the role of screening computed tomography. J Trauma. 2000;48:991–1000.
Yeung KW, Chang MS, Hsiao CP, Huang JF. CT evaluation of gastrointestinal tract perforation. Clin Imaging. 2004;28:329–33.
He L, Yu H, Shi L, He Y, Geng J, Wei Y, et al. Equity assessment of the distribution of CT and MRI scanners in China: a panel data analysis. Int J Equity Health. 2018;17:157.
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Sugase T and the other co-authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
595_2021_2247_MOESM4_ESM.pdf
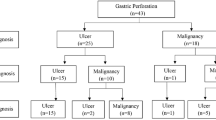
Supplementary file4 Supplemental Fig. 1 Participant flow diagram. Sixty-two consecutive patients who were diagnosed with a perforation of the upper gastrointestinal tract, stomach, or duodenum between 2010 and 2019 were identified from the electronic database at Kinan Hospital. The patients with retroperitoneal air (n=10), intestinal wall air (n=1), and those receiving best supportive care for advanced gastric cancer (n=1) were excluded; finally, the remaining 50 patients with intraperitoneal free air were analyzed. All patients received initial inpatient treatment that was categorized as either surgery (n = 43, 86%) or conservative therapy (n = 7, 14%) (PDF 14 KB)
Rights and permissions
About this article
Cite this article
Sugase, T., Michiura, T., Urabe, S. et al. Optimal treatment and complications of patients with the perforated upper gastrointestinal tract. Surg Today 51, 1446–1455 (2021). https://doi.org/10.1007/s00595-021-02247-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-021-02247-z