Abstract
Aims
To explore the correlation between visceral adipose tissue and albuminuria, and whether there is interaction between visceral adipose tissue and diabetes on albuminuria.
Methods
The study subjects were adult subjects (age ≥ 18 years) from the National Health and Nutrition Examination Surveys (NHANES) database of the USA in 2017–2018. Visceral fat area (VFA) was measured by dual-energy X-ray absorptiometry (DXA). Subjects were divided into three groups according to VFA: low (VFA 0–60cm2), medium (VFA 60–120 cm2) and high (VFA ≥ 120 cm2). Albuminuria was defined as urinary albumin-to-creatinine ratio (UACR) ≥ 30 mg/g. The statistical analysis software used is STATA 17.0.
Results
Data pertaining to 2965 participants (2706 without albuminuria) were included in the analysis. High VFA is an independent risk factor for albuminuria (OR 1.367, 95% CI 1.023–1.827). In the low-VFA group, there is no significant association between diabetes and albuminuria (OR 1.415, 95% CI 0.145–13.849). In the medium-VFA group, diabetes is an independent risk factor for albuminuria (OR 2.217, 95% CI 1.095–4.488). In the high-VFA group, diabetes is also an independent risk factor for albuminuria (OR 5.150, 95% CI 3.150–8.421). There is an additive interaction between high VFA (VFA ≥ 120 cm2) and diabetes on the effect of albuminuria (RERI 3.757, 95% CI 0.927–6.587, p = 0.009), while no multiplication interaction (OR 1.881, 95% CI 0.997–1.023, p = 0.141).
Conclusions
High VFA may represent an independent risk factor for albuminuria. The amount of visceral fat may affect the effect of diabetes on albuminuria. The higher the visceral fat, the stronger the correlation between diabetes and albuminuria should be present. We suppose an additive interaction between VFA and diabetes on the effect of albuminuria.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As one of the common chronic diseases, diabetes is a global public health problem, which brings great challenges to human health. Diabetic nephropathy, one of the chronic microvascular complications of diabetes, causes a great impact on the expectancy and quality of life of diabetic patients. Albuminuria is one of the early manifestations of diabetic nephropathy. In the overall population, diabetes is an independent risk factor for albuminuria, which has been confirmed by numerous studies [1, 2].
Obesity is a condition characterized by insulin resistance, contributing to an elevated risk of type 2 diabetes mellitus [3]. Additionally, obesity plays a role in the progression of type 2 diabetes from the early stages of the disease [4]. Obesity and its metabolic complications also play an important role in the onset and progression of chronic kidney disease (CKD) [5, 6]. However, not all types of adipose tissue contribute equally to kidney injury. Individuals who predominantly store fat in the abdominal area (especially visceral area) tend to have higher risk of metabolic abnormality, such as type 2 diabetes and cardiovascular disease. It was demonstrated by recent studies that visceral adipose tissue (VAT) is more strongly associated with kidney injury [7,8,9], insulin resistance [10, 11] and cardiovascular disease [12] in several clinical conditions, compared with subcutaneous adipose tissue (SAT).
Previous studies have shown that both diabetes and VAT are closely related to albuminuria, however, few studies have focused on the interaction between diabetes and VAT in the risk of albuminuria. The aim of this study was to verify the association between VFA and albuminuria and to further explore the interaction between diabetes and high VFA in the risk of albuminuria.
Methods
Population
NHANES is a population-based, cross-sectional survey aimed to accomplish data collection about the health and nutrition of the U.S. residents. The survey was approved by the National Center for Health Statistics (NCHS) institutional review board, and all subjects signed written informed consent.
Data of subjects in the American NHANES 2017–2018 survey cycle were analyzed. NHANES 2017–2018 data are publicly available and can be accessed online (https://www.cdc.gov). Individuals lack relevant examinations or relevant data were excluded from the analyses. The analyses of the present study were limited to adult individuals, which means all participants were 18 years of age or older.
In the present study, respondents were categorized by ethnicity into white, black, Hispanic, Asian and other races. Body mass index (BMI) was calculated by dividing body weight in kg by square of height in meters. NHANES provides data for three consecutive blood pressure (BP) measurements and we used the second one to avoid deviation caused by emotional tension, physical activities or other factors that can make influence on blood pressure.
Determination of visceral fat areas
In 2017–2018, whole body DXA scans were administered in the NHANES mobile examination center (MEC). The NHANES whole body scans through DXA provide nationally representative data on abdominal soft tissue composition and fat distribution of respondents. Visceral adipose tissue (VAT) were defined by the Hologic APEX software which was used in the scan analysis. Fat of visceral area inside abdominal cavity were measured at the approximate interspace location of L4 and L5 vertebra. Subjects were divided into three groups according to VFA: low (VFA 0 ~ 60cm2), medium (VFA 60 ~ 120 cm2) and high (VFA ≥ 120 cm2).
Definition of albuminuria
Urinary albumin was measured using the latex agglutination method. Urinary albumin-to-creatinine ratio (UACR) was calculated by dividing the urinary albumin in milligram (mg) by urinary creatinine in gram. In the present study, albuminuria was defined as UACR ≥ 30 mg/g [13].
Definition of diabetes
In the present study, individuals meeting any of the following conditions were diagnosed as diabetic patients: (1) confirmed history of diabetes diagnosis in questionnaire; (2) HbA1c level ≥ 6.5%; (3) fasting glucose level ≥ 7.0 mmol/L [14]. In NHANES, defining diabetes type through questionnaires or laboratory data is challenging. Therefore, we did not make a specific classification of diabetes patients or exclude those with type 1 diabetes in the study.
Statistical analysis
The NHANES used a complex, multistage, probability sampling design to select participants representative of non-institutionalized US civilian, so we take this into account in our analyses by using sample weights to adjust for the unequal probability of selection into the survey and to adjust for the possible bias resulting from nonresponse according to NHANES analytic guidelines. The Kolmogorov–Smirnov method was performed to evaluate the data distribution. Continuous variables were represented as mean ± standard deviation (SD) for normally distributed data or medians (interquartile ranges, IQR) for abnormally distributed data. Chi-squared test, Mann–Whitney U-test or independent t-test was applied to evaluate the between-group differences when appropriate. Categorical variables were represented as frequency (percentage), and Chi-squared test was performed to compare the differences between groups. Logistic regression was performed to adjust for potential confounders when appropriate.
Logistic regression analysis was used to evaluated interactive effect between candidate risk factors on dependent variables on both a multiplicative scale and additive scales [15]. Relative excess risk due to the interaction (RERI) was used to evaluate the interaction based on the additive scale [16]. RERI is the excess risk due to the interaction relative to the risk without exposure, and it was interpreted no additive interaction between candidate variables if the 95% CI of RERI contained 0.
p Values < 0.05 was considered to be indicative of statistical significance. All statistical analyses were performed by using the STATA 17.0 software.
Results
Baseline characteristics of the study population are summarized in Table 1. Data pertaining to 2965 participants (2706 without albuminuria) were included in the analysis. Individuals in the albuminuria group were significantly older and had higher BMI, VFA, systolic blood pressure (SBP), diastolic blood pressure, total triglyceride (TG), UA and HbA1c but lower serum creatinine and high-density lipoprotein cholesterol (HDL-c) than individuals without albuminuria (p < 0.05 for all). In the albuminuria group, the proportion of diabetes was higher (p < 0.001) as expected. There was no significant difference in the proportion of male and current smoker between the two groups.
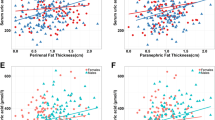
As shown in Table 2, after adjusting for confounding factors such as age, sex, race, smoking, and blood pressure, diabetes was an independent risk factor for albuminuria. But when we grouped all subjects according to visceral fat area, diabetes had a different effect on albuminuria among the different groups. In the high-VFA group, diabetes was an independent risk factor for albuminuria (OR 5.150, 95% CI 3.150–8.421, p < 0.001). In the medium-VFA group, diabetes was still an independent risk factor for albuminuria (OR 2.217, 95% CI 1.095–4.488, p < 0.001). While in the low-VFA group, there was no significant association between diabetes and albuminuria (OR 1.415, 95% CI 0.145–13.849, p = 0.765) (Fig. 1).
After adjusting for confounding factors such as age, sex, race, diabetes, smoking, and blood pressure, VFA was an independent risk factor for albuminuria. While in diabetes group, VFA was not associated with albuminuria (OR 1.702, 95% CI 0.971–2.983, p = 0.063). In non-diabetes group, VFA was not associated with albuminuria either (OR 1.259, 95% CI 0.888–1.786, p = 0.196) (Table 3).
Results of interaction analysis are shown in Table 4. Subjects were divided into four groups according to VFA and diabetes: low VFA (< 120 cm2) without diabetes, low VFA with diabetes, high VFA (≥ 120 cm2) without diabetes, high VFA with diabetes, with the first group as the reference group. Compared to the control group, individuals with high VFA but without diabetes have a higher risk of albuminuria (OR 1.516, 95% CI 1.038–2.216, p = 0.032) after adjusting for age, sex and race. Individuals with low VFA and diabetes have a higher risk of albuminuria (OR 2.315, 95% CI 1.217–4.404, p = 0.011). Individuals with high VFA and diabetes have the highest risk of albuminuria (OR 6.763, 95% CI 4.334–10.554, p < 0.001). Interaction analysis shows that there is an additive interaction between diabetes and VFA on albuminuria (RERI 3.757, 95% CI 0.927–6.587, p = 0.009), and there is no multiplicative interaction between diabetes and VFA on albuminuria (OR 1.881, 95% CI 0.997–1.023, p = 0.141).
Discussion
In low-VFA population, diabetes was not related to albuminuria, while in subjects with medium or high VFA, diabetes was an independent risk factor for albuminuria, consistent with conventional opinion [1, 2]. Among individuals with high VFA (VFA ≥ 120 cm2), diabetes had the strongest effect on albuminuria. The association of diabetes with albuminuria was discrepant in participants with different level of VFA, indicating that visceral fat and diabetes combined additively on pathophysiological changes of kidney. According to our results, diabetes may not be independent risk factor for albuminuria in people with low visceral fat, while there were sufficient evidences that albuminuria is a common complication of lean type 1 diabetes [1, 2]. There are some factors that may confound the present results, such as duration of the disease, treatment, and the presence of other complications (e.g. retinopathy). More studies are needed to confirm or disprove these findings in the future.
It is interesting that similar findings appeared in an Asian study. Bouchi and colleagues found there was a stronger association between blood pressure and albuminuria in individuals with high visceral adiposity than those with low visceral adiposity (β 0.263, p = 0.001 versus β 0.140, p = 0.080). Authors made an inference that visceral adiposity could modify the association of blood pressure with albuminuria [17]. Based on the findings of the above study and our study, we can speculate that visceral fat is involved in regulating the association of multiple metabolic factors with kidney outcomes.
Conventionally we used BMI to assess adiposity, while there are some noteworthy limitations for BMI to assess adiposity. The value of central adiposity measurement is highlighted in studies showing that patients with low or normal BMI but elevated waist circumference, also known as abdominal obesity or sarcopenic obesity, are at the highest risk of end-stage renal disease (ESRD) and death [18,19,20]. Studies have demonstrated that visceral adipose tissue is a major contributor to cardiovascular disease and kidney function decline [21,22,23]. Conversely, fat storage preferential in the lower body depot may serve as a metabolic buffer, protecting other tissues from lipotoxicity [21]. Thereby in the present study, we chose VFA as adiposity metric to probe into the effect of specific type of obesity, that is visceral fat accumulation on albuminuria and its interaction with diabetes.
Previous studies have suggested that visceral fat accumulation evaluating by cumulative average visceral adiposity index (VAI) is independently associated with increased urinary albumin excretion [24, 25]. Most recently, Zhou et al. conducted a study in 10,132 participants from China, which showed that higher cumulative average VAI was associated with a higher risk of progression of renal disease in patients with type 2 diabetes mellitus [26]. The VAI used in these previous studies to quantify visceral fat was calculated indirectly, using a formula that included BMI, waist circumference and other parameters, rather than directly measuring it. Research of Japanese scholars revealed that VFA by the bioelectrical impedance analysis method is also associated with an increase in UACR [27]. In this study, DXA was used to quantify visceral fat more directly and accurately, further verifying the conclusions of previous studies, that high visceral fat is a risk factor for adverse kidney outcomes.
There are several mechanisms that can explain the negative influence of visceral adiposity on kidney. In one aspect, non-specific inflammatory responses are regarded as key mechanism involved in central obesity-related target organ manifestations [28]. The dysregulated adipocytes and macrophages within visceral fat component are metabolically active and may secrete or regulate various adipokines and proinflammatory cytokines, such as leptin [29], adiponectin [30], resistin [31], visfatin [32, 33], and vascular endothelial growth factor [34, 35], which may lead to low-grade systemic inflammation, insulin resistance, dyslipidemia, and/or increased synthesis of vasoactive and fibrogenic substances, eventually leading to impairment of vascular endothelial cells and kidney function [36,37,38,39,40]. On the other hand, the excess visceral adipose tissue accumulated in and around the kidneys, may result in renal physical compression and raise intrarenal tissue pressure, which increase renal sympathetic nervous system (SNS) activity and sequentially activate the renin–angiotensin–aldosterone system (RAAS) [41, 42] and mineralocorticoid receptor [43]. Moreover, renal sinus fat accumulation is associated with glomerular hypertrophy and angiotensinogen produced in the renal tissue. Intratubular angiotensinogen stimulates the production of angiotensin II, which elevates blood pressure by acting on angiotensin II type 1 receptors [44]. These would combinedly cause gradual loss of nephrons [45].
VFA is closely associated with albuminuria in the whole population. In contrast, our subgroup analysis revealed that VFA was not associated with increased adjusted risk of albuminuria in participants with or without diabetes. These data emphasize the complex interplay between diabetes and obesity in the modulation of albuminuria.
We present an interaction analysis of diabetes with VFA on albuminuria in a large cohort stratified by baseline diabetes status and VFA category. Albuminuria was more common as VFA rose, but in the presence of diabetes, event rates were much greater. Indeed, participants with diabetes and low-VFA experienced higher adjusted event rates than high-VFA participants without diabetes. Eventually, our interaction analysis revealed a significant additive interaction between high visceral fat and diabetes with an increased risk of albuminuria. Even at an earlier stage, such interaction may be present. Previous study suggested a significant interaction between central obesity-related abnormal lipid metabolism and prediabetes, which exert a synergistic effect on microalbuminuria [46].
To the best of our knowledge, this is the first study trying to explore the interaction between VFA and diabetes on albuminuria. Moreover, not exhaustive enough but reliable database from NHANES and a relatively large sample size are strengths of this study.
However, we must also acknowledge limitations. First of all, we did not exclude those with type 1 diabetes in the study. Given the different pathogenesis of type 1 diabetes and type 2 diabetes, this may have some impact on the findings to a certain extent. Second, our work is observational cross-sectional study, so we could not make causality inference. Third, NHANES only report whether taking prescription for hypertension, but no specific types of antihypertensive agents (RAAS inhibitors, CCB, et al.), so we can’t eliminate the impact of RAAS inhibitors on the results. Moreover, participants were recruited before widespread use of sodium–glucose cotransporter 2 (SGLT-2) inhibitors or mineralocorticoid receptor antagonist (finerenone), which improve renal outcomes. Therefore, event rates in participants with diabetes may be higher in our study than contemporary data. Fourth, in clinical practice, we conduct three UACR tests to diagnose or exclude albuminuria, while in NHANES, subjects undergo a one-time examination. Fifth, there is a bias of abdominal VAT measures of DXA compared with MRI, but the high rank correlation makes DXA a good alternative to MRI which is more complicated and time-consuming [47]. Hopefully, there will be studies verifying our findings through MRI in the future. Last but not least, adiposity estimates of DXA were often sex and race/ethnicity specific [48], future studies may conduct subgroup analysis according to specific estimates of sex and race, or validate our findings through broader populations.
Conclusions
High VFA may constitute an independent risk factor for albuminuria. The quantity of visceral fat could influence the impact of diabetes on albuminuria. The greater the visceral fat, the more pronounced the correlation between diabetes and albuminuria is expected to be. We suppose an additive interaction between VFA and diabetes on the effect of albuminuria.
References
Viberti GC, Pickup JC, Jarrett RJ, Keen H (1979) Effect of control of blood glucose on urinary excretion of albumin and beta2 microglobulin in insulin-dependent diabetes. N Engl J Med 300(12):638–641
Parving HH (1996) Initiation and progression of diabetic nephropathy. N Engl J Med 335(22):1682–1683
Després JP, Lemieux S, Lamarche B et al (1995) The insulin resistance-dyslipidemic syndrome: contribution of visceral obesity and therapeutic implications. Int J Obes Relat Metab Disord 19(Suppl 1):S76-86
Pulgaron ER, Delamater AM (2014) Obesity and type 2 diabetes in children: epidemiology and treatment. Curr Diab Rep 14(8):508
Cases A, Coll E (2005) Dyslipidemia and the progression of renal disease in chronic renal failure patients. Kidney Int Suppl 99:S87-93
Gyebi L, Soltani Z, Reisin E (2012) Lipid nephrotoxicity: new concept for an old disease. Curr Hypertens Rep 14(2):177–181
Foster MC, Hwang SJ, Massaro JM et al (2011) Association of subcutaneous and visceral adiposity with albuminuria: the Framingham Heart Study. Obesity (Silver Spring) 19(6):1284–1289
Hanai K, Babazono T, Nyumura I et al (2010) Involvement of visceral fat in the pathogenesis of albuminuria in patients with type 2 diabetes with early stage of nephropathy. Clin Exp Nephrol 14(2):132–136
Kim SR, Yoo JH, Song HC et al (2011) Relationship of visceral and subcutaneous adiposity with renal function in people with type 2 diabetes mellitus. Nephrol Dial Transplant 26(11):3550–3555
Preis SR, Massaro JM, Robins SJ et al (2010) Abdominal subcutaneous and visceral adipose tissue and insulin resistance in the Framingham heart study. Obesity (Silver Spring) 18(11):2191–2198
Du T, Yuan G, Zhang M et al (2014) Clinical usefulness of lipid ratios, visceral adiposity indicators, and the triglycerides and glucose index as risk markers of insulin resistance. Cardiovasc Diabetol 13:146
Britton KA, Massaro JM, Murabito JM et al (2013) Body fat distribution, incident cardiovascular disease, cancer, and all-cause mortality. J Am Coll Cardiol 62(10):921–925
Stevens PE, Levin A (2013) Kidney disease: improving global outcomes chronic kidney disease guideline development work group members. Evaluation and management of chronic kidney disease: synopsis of the kidney disease: improving global outcomes 2012 clinical practice guideline. Ann Int Med. 158(11):825–830
American Diabetes Association Professional Practice Committee (2022) 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2022. Diabetes Care 45(Suppl 1):17–38
Knol MJ, Vander Weele TJ, Groenwold RH et al (2011) Estimating measures of interaction on an additive scale for preventive exposures. Eur J Epidemiol 26(6):433–438
Yang X, Zhao H, Sui Y et al (2009) Additive interaction between the renin-angiotensin system and lipid metabolism for cancer in type 2 diabetes. Diabetes 58(7):1518–1525
Bouchi R, Ohara N, Asakawa M et al (2016) Is visceral adiposity a modifier for the impact of blood pressure on arterial stiffness and albuminuria in patients with type 2 diabetes. Cardiovasc Diabetol 15:10
Kramer H, Shoham D, McClure LA et al (2011) Association of waist circumference and body mass index with all-cause mortality in CKD: the REGARDS (Reasons for Geographic and Racial Differences in Stroke) Study. Am J Kidney Dis 58(2):177–185
Postorino M, Marino C, Tripepi G, Zoccali C (2009) CREDIT (Calabria registry of dialysis and transplantation) working group. Abdominal obesity and all-cause and cardiovascular mortality in end-stage renal disease. J Am Coll Cardiol 53(15):1265–1272
Kovesdy CP, Czira ME, Rudas A et al (2010) Body mass index, waist circumference and mortality in kidney transplant recipients. Am J Transplant 10(12):2644–2651
Neeland IJ, Poirier P, Després JP (2018) Cardiovascular and metabolic heterogeneity of obesity: clinical challenges and implications for management. Circulation 137(13):1391–1406
Katzmarzyk PT, Heymsfield SB, Bouchard C (2013) Clinical utility of visceral adipose tissue for the identification of cardiometabolic risk in white and African American adults. Am J Clin Nutr 97(3):480–486
Madero M, Katz R, Murphy R et al (2017) Comparison between different measures of body fat with kidney function decline and incident CKD. Clin J Am Soc Nephrol 12(6):893–903
Sun K, Lin D, Li F et al (2019) Visceral adiposity index is associated with increased urinary albumin excretion: a population-based study. Clin Nutr 38(3):1332–1338
Wen J, Yuan H (2020) Independent association between the visceral adiposity index and microalbuminuria in patients with newly diagnosed type 2 diabetes. Diabetes Metab Res Rev 36(1):e3198
Zhou C, Zhang Y, Yang S et al (2023) Associations between visceral adiposity index and incident nephropathy outcomes in diabetic patients: insights from the ACCORD trial. Diabetes Metab Res Rev 39(3):e3602
Tamba S, Nakatsuji H, Kishida K et al (2010) Relationship between visceral fat accumulation and urinary albumin-creatinine ratio in middle-aged Japanese men. Atherosclerosis 211(2):601–605
Ghigliotti G, Barisione C, Garibaldi S et al (2014) Adipose tissue immune response: novel triggers and consequences for chronic inflammatory conditions. Inflammation 37(4):1337–1353
Sharma K, Considine RV, Michael B et al (1997) Plasma leptin is partly cleared by the kidney and is elevated in hemodialysis patients. Kidney Int 51(6):1980–1985
Sharma K, Ramachandrarao S, Qiu G et al (2008) Adiponectin regulates albuminuria and podocyte function in mice. J Clin Invest 118(5):1645–1656
Axelsson J, Bergsten A, Qureshi AR et al (2006) Elevated resistin levels in chronic kidney disease are associated with decreased glomerular filtration rate and inflammation, but not with insulin resistance. Kidney Int 69(3):596–604
Malyszko J, Malyszko JS, Mysliwiec M (2009) Visfatin, a new adipocytokine, is predominantly related to inflammation/endothelial damage in kidney allograft recipients. Transplant Proc 41(1):150–153
Song HK, Lee MH, Kim BK et al (2008) Visfatin: a new player in mesangial cell physiology and diabetic nephropathy. Am J Physiol Renal Physiol 295(5):F1485–F1494
Miyazawa-Hoshimoto S, Takahashi K, Bujo H, Hashimoto N, Saito Y (2003) Elevated serum vascular endothelial growth factor is associated with visceral fat accumulation in human obese subjects. Diabetologia 46(11):1483–1488
Shulman K, Rosen S, Tognazzi K, Manseau EJ, Brown LF (1996) Expression of vascular permeability factor (VPF/VEGF) is altered in many glomerular diseases. J Am Soc Nephrol 7(5):661–666
Imig JD, Ryan MJ (2013) Immune and inflammatory role in renal disease. Compr Physiol 3(2):957–976
Kurozumi A, Okada Y, Arao T, Tanaka Y (2016) Excess visceral adipose tissue worsens the vascular endothelial function in patients with type 2 diabetes mellitus. Intern Med 55(21):3091–3095
Kim SH, Després JP, Koh KK (2016) Obesity and cardiovascular disease: friend or foe. Eur Heart J 37(48):3560–3568
Wu CC, Liou HH, Su PF et al (2011) Abdominal obesity is the most significant metabolic syndrome component predictive of cardiovascular events in chronic hemodialysis patients. Nephrol Dial Transplant 26(11):3689–3695
Mathew AV, Okada S, Sharma K (2011) Obesity related kidney disease. Curr Diabetes Rev 7(1):41–49
Hall JE, do Carmo JM, da Silva AA, Wang Z, Hall ME (2015) Obesity-induced hypertension: interaction of neurohumoral and renal mechanisms. Circ Res 116(6):991–1006
Engeli S, Sharma AM (2001) The renin-angiotensin system and natriuretic peptides in obesity-associated hypertension. J Mol Med (Berl) 79(1):21–29
de Paula RB, da Silva AA, Hall JE (2004) Aldosterone antagonism attenuates obesity-induced hypertension and glomerular hyperfiltration. Hypertension 43(1):41–47
Fujioka H, Koike T, Imamura T et al (2023) Prognostic impact of renal sinus fat accumulation in patients with chronic kidney disease. Clin Exp Nephrol 27(7):613–621
Hall ME, do Carmo JM, da Silva AA et al (2014) Obesity, hypertension, and chronic kidney disease. Int J Nephrol Renovasc Disease 7:75–88
Choi JW, Oh IH, Lee CH, Park JS (2017) Effect of synergistic interaction between abnormal adiposity-related metabolism and prediabetes on microalbuminuria in the general population. PLoS ONE 12(7):e0180924
Reinhardt M, Piaggi P, DeMers B, Trinidad C, Krakoff J (2017) Cross calibration of two dual-energy X-ray densitometers and comparison of visceral adipose tissue measurements by iDXA and MRI. Obesity (Silver Spring) 25(2):332–337
Sneed NM, Morrison SA (2021) Body composition methods in adults with type 2 diabetes or at risk for T2D: a clinical review. Curr Diabetes Rep 21(5):14
Acknowledgements
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. These investigators received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
YL and DZ conceived and designed the experiments. YL performed the data analysis. YL wrote the manuscript. SC and XZ provided supervision. All authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. These investigators received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Ethical Standard Statement or Human and Animal Rights disclosure
All authors declare that this study on human subjects were conducted in accordance with the Declaration of Helsinki
Informed consent disclosure
The original survey was approved by the NCHS Research Ethics Review Board (ERB), and all participants provided written informed consent.
Additional information
Communicated by Massimo Federici.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liu, Y., Zhao, D., Chai, S. et al. Association of visceral adipose tissue with albuminuria and interaction between visceral adiposity and diabetes on albuminuria. Acta Diabetol 61, 909–916 (2024). https://doi.org/10.1007/s00592-024-02271-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-024-02271-8