Abstract
Aims
The use of statins has been associated with an increased risk of new-onset diabetes. The characteristics of the population could influence this association. The objective of this study was to determine the risk of new-onset diabetes with the use of statins in patients in primary prevention, with an assessment of the results according to the baseline risk of developing diabetes of the included population.
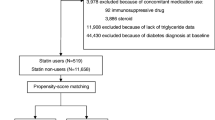
Methods
We performed an updated meta-analysis including randomized trials of statin therapy in primary prevention settings that report new-onset diabetes. The rate of new cases of diabetes in the control arms was estimated for each study. The studies were classified into two groups (low rate: < 7.5 events per 1000 patients-year; high rate; ≥ 7.5 events per 1000 patients-year). The fixed-effects model was performed.
Results
Eight studies (70,453 patients) were included. Globally, statin therapy was associated with an increased risk of new-onset diabetes (OR 1.1; 95% CI 1.0–1.2, I2 35%). When we analyzed the studies according to the baseline diabetes risk in the control groups, the results showed that there was a greater risk only in the studies with a high baseline rate (OR 1.2; 95% CI 1.1–1.3, I2 0%; interaction p value = 0.01).
Conclusion
Globally, the use of statins in patients in primary prevention was associated with an increased risk of new-onset diabetes. In the stratified analysis, this association was observed only in the group of studies with a high baseline rate of events.






Similar content being viewed by others
Availability of data and material
The data underlying this article are available in the article and in its online supplementary material.
References
Zhang X, Xing L, Jia X, Pang X, Xiang Q, Zhao X et al (2020) Comparative lipid-lowering/increasing efficacy of 7 statins in patients with dyslipidemia, cardiovascular diseases, or diabetes mellitus: systematic review and network meta-analyses of 50 randomized controlled trials. Cardiovasc Ther 2020:3987065. https://doi.org/10.1155/2020/3987065
Jaam M, Al-Naimi HN, Haddad MM, Abushanab D, Al-Badriyeh D (2023) Comparative efficacy and safety among high-intensity statins. Systematic review and meta-analysis. J Comp Eff Res 12(3):e220163. https://doi.org/10.57264/cer-2022-0163
Sattar N, Preiss D, Murray HM, Welsh P, Buckley BM, de Craen AJ et al (2010) Statins and risk of incident diabetes: a collaborative meta-analysis of randomised statin trials. Lancet 375(9716):735–742. https://doi.org/10.1016/S0140-6736(09)61965-6
Preiss D, Seshasai SR, Welsh P, Murphy SA, Ho JE, Waters DD et al (2011) Risk of incident diabetes with intensive-dose compared with moderate-dose statin therapy: a meta-analysis. JAMA 305(24):2556–2564. https://doi.org/10.1001/jama.2011.860
Navarese EP, Bufon A, Andreotti F, Kozinski M, Welton N, Fabiszak T et al (2013) Meta-analysis of impact of different types and doses of statins on new onset diabetes mellitus. Am J Cardiol 111(8):1123–1130. https://doi.org/10.1016/j.amjcard.2012.12.037
Seo WW, Seo SI, Kim Y, Yoo JJ, Shin WG, Kim J et al (2022) Impact of pitavastatin on new-onset diabetes mellitus compared to atorvastatin and rosuvastatin: a distributed network analysis of 10 real-world databases. Cardiovasc Diabetol 21(1):82. https://doi.org/10.1186/s12933-022-01524-6
Ridker PM, Danielson E, Fonseca FAH, Genest J, Gotto AM Jr, Kastelein JJP et al (2008) Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med 359(21):2195–2207. https://doi.org/10.1056/NEJMoa0807646
Chobot A, Górowska-Kowolik K, Sokołowska M, Jarosz-Chobot P (2018) Obesity and diabetes-Not only a simple link between two epidemics. Diabetes Metab Res Rev 34(7):e3042. https://doi.org/10.1002/dmrr.3042
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. https://doi.org/10.1136/bmj.n71
National Diabetes Statistics Report (2020) https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf. Accessed 30 July 2023
Sterne JAC, Savovic J, Page MJ, Elbers RG, Blencowe NS, Boutron I et al (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 28(366):l4898. https://doi.org/10.1136/bmj.l4898
Viechtbauer W (2010) Conducting meta-analyses in R with the metaphor package. J Stat Soft 36(3):1–48. https://doi.org/10.18637/jss.v036.i03
Shepherd J, Cobbe SM, Ford I, Isles CG, Lorimer AR, MacFarlane PW et al (1995) Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. West of scotland coronary prevention study group. N Engl J Med 333(20):1301–1307. https://doi.org/10.1056/NEJM199511163332001
Downs JR, Clearfield M, Weis S, Whitney E, Shapiro DR, Beere PA et al (1998) Primary prevention of acute coronary events with lovastatin in men and women with average cholesterol levels: results of AFCAPS/TexCAPS. Air Force/texas coronary atherosclerosis prevention study. JAMA 279(20):1615–1622. https://doi.org/10.1001/jama.279.20.1615
Yusuf S, Bosch J, Dagenais G, Zhu J, Xavier D, Liu L et al (2016) Cholesterol lowering in intermediate-risk persons without cardiovascular disease. N Engl J Med 374(21):2021–2031. https://doi.org/10.1056/NEJMoa1600176
Sever PS, Dahlöf B, Poulter NR, Wedel H, Beevers G, Caulfield M et al (2003) Prevention of coronary and stroke events with atorvastatin in hypertensive patients who have average or lower-than-average cholesterol concentrations, in the anglo-scandinavian cardiac outcomes trial-lipid lowering arm (ASCOT-LLA): a multicentre randomised controlled trial. Lancet 361(9364):1149–1158. https://doi.org/10.1016/S0140-6736(03)12948-0
ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group (2002) Major outcomes in moderately hypercholesterolemic, hypertensive patients randomized to pravastatin vs usual care: the antihypertensive and lipid-lowering treatment to prevent heart attack trial (ALLHAT-LLT). JAMA 288(23):2998–3007. https://doi.org/10.1001/jama.288.23.2998
Nakamura H, Arakawa K, Itakura H, Kitabatake A, Goto Y, Toyota T et al (2006) Primary prevention of cardiovascular disease with pravastatin in Japan (MEGA Study): a prospective randomised controlled trial. Lancet 368(9542):1155–1163. https://doi.org/10.1016/S0140-6736(06)69472-5
Grinspoon SK, Fitch KV, Zanni MV, Fichtenbaum CJ, Umbleja T, Aberg JA et al (2023) Pitavastatin to prevent cardiovascular disease in HIV infection. N Engl J Med 389(8):687–699. https://doi.org/10.1056/NEJMoa2304146
Patti G, Spinoni EG, Grisafi L, Mehran R, Mennuni M (2023) Safety and efficacy of very low LDL-cholesterol intensive lowering: a meta-analysis and meta-regression of randomized trials. Eur Heart J Cardiovasc Pharmacother 9(2):138–147. https://doi.org/10.1093/ehjcvp/pvac049
Chiu SW, Pratt CM, Feinn R, Chatterjee S (2020) Proprotein convertase Subtilisin/Kexin Type 9 inhibitors and ezetimibe on risk of new-onset diabetes: a systematic review and meta-analysis of large, double-blinded randomized controlled trials. J Cardiovasc Pharmacol Ther 25(5):409–417. https://doi.org/10.1177/1074248420924983
Masson W, Lobo M, Lavalle-Cobo A, Masson G, Molinero G (2020) Effect of bempedoic acid on new onset or worsening diabetes: a meta-analysis. Diabetes Res Clin Pract 168:108369. https://doi.org/10.1016/j.diabres.2020.108369
Filippatos TD, Panagiotopoulou T, Tzavella E, Elisaf MS (2018) Hypolipidemic drugs and diabetes mellitus-mechanisms and data from genetic trials. J Cardiovasc Pharmacol Ther 23:187–191. https://doi.org/10.1177/1074248418757011
Ference BA, Robinson JG, Brook RD, Catapano AL, Chapman MJ, Neff DR et al (2016) Variation in PCSK9 and HMGCR and risk of cardiovascular disease and diabetes. N Engl J Med 375:2144–2153. https://doi.org/10.1056/NEJMoa1604304
Schmidt AF, Swerdlow DI, Holmes MV, Patel RS, Fairhurst-Hunter Z, Lyall DM et al (2017) PCSK9 genetic variants and risk of type 2 diabetes: a mendelian randomisation study. Lancet Diabetes Endocrinol 5:97–105. https://doi.org/10.1016/S2213-8587(16)30396
Swerdlow DI, Preiss D, Kuchenbaecker KB, Holmes MV, Engmann JEL, Shah T et al (2015) HMG-coenzyme a reductase inhibition, type 2 diabetes, and bodyweight: evidence from genetic analysis and randomised trials. Lancet 385(9965):351–361. https://doi.org/10.1016/S0140-6736(14)61183-1
Besseling J, Kastelein JJP, Defesche JC, Hutten BA, Hovingh GK (2015) Association between familial hypercholesterolemia and prevalence of type 2 diabetes mellitus. JAMA 313(10):1029–3106. https://doi.org/10.1001/jama.2015.1206
Langhi C, Cariou B (2010) Cholesterol metabolism and beta-cell function. Med Sci (Paris) 26(4):385–390. https://doi.org/10.1051/medsci/2010264385
Xia F, Xie L, Mihic A, Gao X, Chen Y, Gaisano HY et al (2008) Inhibition of cholesterol biosynthesis impairs insulin secretion and voltage-gated calcium channel function in pancreatic beta-cells. Endocrinology 149(10):5136–5145. https://doi.org/10.1210/en.2008-0161
Hafner M, Juvan P, Rezen T, Monostory K, Pascussi JM, Rozman D (2011) The human primary hepatocyte transcriptome reveals novel insights into atorvastatin and rosuvastatin action. Pharmacogenet Genomics 21(11):741–750. https://doi.org/10.1097/FPC.0b013e32834a5585
Nakata M, Nagasaka S, Kusaka I, Matsuoka H, Ishibashi S, Yada T (2006) Effects of statins on the adipocyte maturation and expression of glucose transporter 4 (SLC2A4): implications in glycaemic control. Diabetologia 49(8):1881–1892. https://doi.org/10.1007/s00125-006-0269-5
Khamseh ME, Malek M, Aghili R, Emami Z (2011) Sarcopenia and diabetes: pathogenesis and consequences. Br J Diabetes Vasc Dis 11:230–234. https://doi.org/10.1177/1474651411413644
Cho Y, Choe EY, Lee Y-H, Seo JW, Choi Y, Yun Y et al (2015) Risk of diabetes in patients treated with HMG-CoA reductase inhibitors. Metabolism 64(4):482–488. https://doi.org/10.1016/j.metabol.2014.09.008
Asgari S, Khalili D, Hosseinpanah F, Hadaegh F (2021) Prediction models for type 2 diabetes risk in the general population: a systematic review of observational studies. Int J Endocrinol Metab 19(3):e109206. https://doi.org/10.5812/ijem.109206
Shin J-A, Lee J-H, Lim S-Y, Ha H-S, Kwon H-S, Park Y-M et al (2013) Metabolic syndrome as a predictor of type 2 diabetes, and its clinical interpretations and usefulness. J Diabetes Investig 4(4):334–343. https://doi.org/10.1111/jdi.12075
Tsalamandris S, Antonopoulos AS, Oikonomou E, Papamikroulis G-A, Vogiatzi G, Papaioannou S et al (2019) The role of inflammation in diabetes: current concepts and future perspectives. Eur Cardiol 14(1):50–59. https://doi.org/10.15420/ecr.2018.33.1
Dregan A, Charlton J, Chowienczyk P, Gulliford MC (2014) Chronic inflammatory disorders and risk of type 2 diabetes mellitus, coronary heart disease, and stroke: a population-based cohort study. Circulation 130(10):837–844. https://doi.org/10.1161/CIRCULATIONAHA.114.009990
Nansseu JR, Bigna JJ, Kaze AD, Noubiap JJ (2018) Incidence and risk factors for prediabetes and diabetes mellitus among HIV-infected adults on antiretroviral therapy: a systematic review and meta-analysis. Epidemiology 29(3):431–441. https://doi.org/10.1097/EDE.0000000000000815
Lingvay I, Sumithran P, Cohen RV, le Roux CW (2022) Obesity management as a primary treatment goal for type 2 diabetes: time to reframe the conversation. Lancet 399:394–405. https://doi.org/10.1016/S0140-6736(21)01919-X
Hu FB (2011) Globalization of diabetes: the role of diet, lifestyle, and genes. Diabetes Care 34:1249–1257. https://doi.org/10.2337/dc11-0442
Yamagishi K, Iso H (2017) The criteria for metabolic syndrome and the national health screening and education system in Japan Epidemiol. Health 39:e2017003. https://doi.org/10.4178/epih.e2017003
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
WM and LB participated in the conception and design of the research. WM, LB and JPN participated in the data collection. The interpretation of the data and the statistical analysis was done by WM and ML. WM and LB drafted the manuscript. All authors performed a critical review of the final document. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Not applicable to this study (meta-analysis).
Human and animal rights
Not applicable to this study (meta-analysis).
Additional information
Managed by Antonio Secchi.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Masson, W., Lobo, M., Barbagelata, L. et al. Statins and new-onset diabetes in primary prevention setting: an updated meta-analysis stratified by baseline diabetes risk. Acta Diabetol 61, 351–360 (2024). https://doi.org/10.1007/s00592-023-02205-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-023-02205-w