Abstract
Aims
The Italian Titration Approach Study (ITAS) demonstrated comparable HbA1c reductions and similarly low hypoglycaemia risk at 6 months in poorly controlled, insulin-naïve adults with T2DM who initiated self- or physician-titrated insulin glargine 300 U/mL (Gla-300) in the absence of sulphonylurea/glinide. The association of patient characteristics with glycaemic and hypoglycaemic outcomes was assessed.
Methods
This post hoc analysis investigated whether baseline patient characteristics and previous antihyperglycaemic drugs were associated with HbA1c change and hypoglycaemia risk in patient- versus physician-managed Gla-300 titration.
Results
HbA1c change, incidence of hypoglycaemia (any type) and nocturnal rates were comparable between patient- and physician-managed arms in all subgroups. Hypoglycaemia rates across subgroups (0.03 to 3.52 events per patient-year) were generally as low as observed in the full ITAS population. Small increases in rates of 00:00–pre-breakfast and anytime hypoglycaemia were observed in the ≤ 10-year diabetes duration subgroup in the patient- versus physician-managed arm (heterogeneity of effect; p < 0.05).
Conclusions
Comparably fair glycaemic control and similarly low hypoglycaemia risk were achieved in almost all patient subgroups with patient- versus physician-led Gla-300 titration. These results reinforce efficacy and safety of Gla-300 self-titration across a range of phenotypes of insulin-naïve people with T2DM.
Clinical trial registration
EudraCT 2015-001167-39
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In Italy, approximately 50% of people with type 2 diabetes (T2DM) have glycated haemoglobin (HbA1c) above the commonly recommended target of 7.0% (53 mmol/mol) [1]. Poor glycaemic control can be attributed to various causes including, but not limited to, delay in basal insulin (BI) initiation as well as its titration [2]. The latter may be due to a lack of time or resources available to the healthcare team, infrequent clinic visits, fear of injections, worries about hypoglycaemia, concerns about weight gain and clinical inertia [2]. Providing appropriate tools and support to allow people with diabetes to self-titrate their BI can improve glycaemic outcomes and benefit psychological well-being by allowing them to feel more in control of their condition [3, 4].
The Italian Titration Approach Study (ITAS) has shown that, with the assistance of a specialist diabetes nurse, people with T2DM who are insulin naïve and have poor glycaemic control can initiate and self-titrate their insulin glargine 300 U/mL (Gla-300) dose with comparable HbA1c reductions and comparably low risk of hypoglycaemia versus physician-managed dose titration, in the absence of sulphonylureas (SU)/glinides [5]. The aim of the current post hoc subgroup analysis was to examine whether the results of ITAS are affected by baseline patient characteristics, such as age, renal function, diabetes duration, body mass index (BMI), HbA1c and previous therapy.
Materials and methods
In this post hoc analysis, the main study endpoints in ITAS (change in HbA1c, incidence and rates of hypoglycaemia at week 24) were assessed in the following subgroups of patients: age (< 65 and ≥ 65 years), class of estimated glomerular filtration rate (eGFR; < 60 and ≥ 60 ml/min/1.73 m2), known diabetes duration (≤ 10 and > 10 years), BMI (< 30 and ≥ 30 kg/m2), HbA1c at baseline (≤ 8.5 and > 8.5% [≤ 69/ > 69 mmol/mol]) and number/type of previous antihyperglycaemic drugs (only metformin, metformin plus other antihyperglycaemic drug or no prior metformin) (Table 1).
The study design and results of ITAS have been previously reported [5, 6]. Briefly, ITAS (EudraCT number: 2015-001167-39) was an Italian national, multicentre, phase IV, 24-week, open-label, randomised (1:1), parallel-group study (EudraCT number: 2015-001167-39), in insulin-naïve adults (≥ 18 years of age) with T2DM for ≥ 1 year and poor glycaemic control (HbA1c ≥ 7.5 and ≤ 10% [≤ 53/ ≤ 86 mmol/mol]) on oral antihyperglycaemic drugs (OADs). SU/glinide treatment was discontinued at randomisation. The primary aim of ITAS was to assess non-inferiority in the change in HbA1c over 24 weeks when Gla-300 dose titration was managed by the patient (with nurse assistance) or the physician, both using the same BI dose algorithm (Supplementary Table 1). Secondary outcomes included the incidence of ≥ 1 confirmed (≤ 70 mg/dL [≤ 3.9 mmol/L]) and/or severe hypoglycaemia, nocturnal (events in the time interval 00:00–05:59 h, as well as 00:00–pre-breakfast) [7, 8], or at any time of day (24 h), as well as the annualised rate of hypoglycaemic events. Severe hypoglycaemia was defined as an event that required the assistance of another person to actively administer carbohydrate or glucagon or to perform other resuscitative actions.
All participants provided written informed consent. The clinical trial protocol was approved by the appropriate local ethics committees and IRB/IEC. The study was conducted in accordance with the Declaration of Helsinki and the ICH guidelines for Good Clinical Practice (GCP) [9].
Statistical analysis
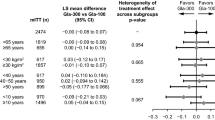
Change in HbA1c at week 24 was analysed in each subgroup using the same model described for the main study analysis, i.e. a linear mixed-effect model (LMEM) for repeated measures with titration approach and centre as fixed effects and the HbA1c baseline value as covariate. For the primary study endpoint, homogeneity of the treatment effect among subgroups was assessed by including a subgroup by-treatment interaction in the LMEM.
Hypoglycaemia incidences were calculated as the proportion of patients with ≥ 1 hypoglycaemia over study period. Besides, the corresponding relative risk with the 95% confidence intervals (CI) by endpoint in each subgroup was presented. The Breslow–Day test was used to evaluate whether the risk of hypoglycaemic event was consistent (homogeneous) across the levels in each subgroup.
The hypoglycaemic events were analysed by means of a binomial (NB) regression analysis to obtain model-based estimates of annual rate (events per patient-year), rate ratios and p values for the treatment heterogeneity effect.
Differences in treatment effects across subgroups were only considered relevant if significant heterogeneity was observed (p < 0.05); however, due to the post hoc nature of this analysis, the inferential statistical tests will be used only for exploratory purposes.
Results
Baseline characteristics
Baseline characteristics of the overall ITAS population have been presented previously [5, 6]. The distribution of subgroups was balanced between treatment arms (Table 1), and sample size was also generally well balanced among subgroups within treatment arms with the exceptions of the eGFR < 60 mL/min/1.73 m2 and no prior metformin subgroups, which were noticeably smaller.
Glycaemic control
HbA1c change at 6 months was comparable between the patient- and physician-managed arms, regardless of patient subgroup (Fig. 1, Supplementary Table 2). No evidence of heterogeneity of treatment effect was observed across any subgroup (p ≥ 0.05). The least squares (LS) mean differences (95% CI) between the patient- and physician-managed arms in each subgroup are reported in Fig. 1 and Supplementary Table 2.
Hypoglycaemia
Incidence of confirmed (≤ 70 mg/dL [≤ 3.9 mmol/L]) and/or severe hypoglycaemic events
The risk of experiencing ≥ 1 nocturnal (00:00–05:59 h) or 00:00–pre-breakfast (expanded nocturnal window) confirmed (≤ 70 mg/dL [≤ 3.9 mmol/L]) and/or severe hypoglycaemic event was low in all subgroups, as already shown in ITAS [5]. Incidence of hypoglycaemia was unaffected by any of the assessed patient subgroups, with no evidence of heterogeneity of treatment effect observed (p ≥ 0.05). The relative risks (95% CI) of these nocturnal events in the patient-managed arm compared with the physician-managed arms are reported for each subgroup in Fig. 2a, b. Similarly, the incidence of any time confirmed (≤ 70 mg/dL [≤ 3.9 mmol/L]) and/or severe hypoglycaemia was not affected by any of the patient subgroups investigated (Fig. 2c). Severe hypoglycaemia in ITAS occurred in three out of 355 patients with a total of four events (two patients in the physician-managed arm) yielding a cumulative incidence of 0.8% [5].
Incidence of confirmed (≤ 70 mg/dL, ≤ 3.9 mmol/L) and/or severe hypoglycaemia [(a) nocturnal (00:00–05:59 h), (b) 00:00 h–pre-breakfast, (c) any time] over 24 weeks in the subgroups of the ITAS population, and differences between treatments (patient- and physician-managed BI titration). BMI, body mass index; CI, confidence intervals; eGFR, estimated glomerular filtration rate; NC, not calculable. p values derived from a Breslow–Day test of homogeneity
Annualised rate of confirmed (≤ 70 mg/dL [≤ 3.9 mmol/L]) and/or severe hypoglycaemic events
The number of hypoglycaemic events and patient time at risk used to calculate the annualised rate of events are shown in Supplementary Table 3. Hypoglycaemia rates across subgroups were as low as observed in the full ITAS population [5].
No heterogeneity of treatment effect was observed for nocturnal (00:00–05.59 h) rates of hypoglycaemia in any subgroup (Fig. 3a). Statistically significant heterogeneity was observed for rates of the expanded window of nocturnal hypoglycaemia (00:00–pre-breakfast) in the subgroup of patients with disease duration ≤ 10 years due to higher rates of hypoglycaemic events in the patient-managed arm compared with the physician-managed arm (Fig. 3b). Similar results were observed for rates of any time hypoglycaemia in the same subgroup (Fig. 3c).
Annualised rates of confirmed (≤ 70 mg/dL, ≤ 3.9 mmol/L) and/or severe hypoglycaemia [(a) nocturnal (00:00–05:59 h), (b) 00:00 h–pre-breakfast, (c) any time] over 24 weeks in the subgroups of the ITAS population, and differences between treatments (patient- and physician-managed BI titration). BMI, body mass index; CI, confidence intervals; eGFR, estimated glomerular filtration rate; NC, not calculable. Annual rates presented as events per patient-year. Estimates and p values derived from a negative binomial (NB) regression model
Discussion
ITAS has previously shown that insulin-naïve people with T2DM, uncontrolled on OADs and/or non-insulin injectables can effectively and safely self-titrate Gla-300 (in the absence of SU/glinides treatment), with no differences in terms of HbA1c reduction or risk of hypoglycaemia versus physician-managed titration [5]. The results of the present post hoc sub-analysis show that the improvement in glycaemic control was superimposable, and the incidence of hypoglycaemia was similarly low and not different between patient- and physician-managed titration of Gla-300 arms, regardless of age, renal function, diabetes duration, glycaemic control, BMI and metformin as the only treatment. The only statistically significant difference detected between the patient- and physician-managed arms was the annualised rate of hypoglycaemia (00:00 h–pre-breakfast, any time) in the subgroups with diabetes duration ≤ 10 years, which was higher in the patient-managed arm. However, the rates of non-severe hypoglycaemia were low and severe hypoglycaemia was virtually absent as observed in ITAS [5]. These results of similar incidence but greater rates of hypoglycaemia might be interpreted as a signal of more aggressive BI titration by some individual patients with shorter diabetes duration versus physicians. It is worth noting that a shorter diabetes duration has been reported as an indicator of greater likelihood to achieve HbA1c < 7.0% in a large global population [10]. The small increase in rates of hypoglycaemia observed only in the diabetes duration subgroup of patient-managed titration in the present post hoc analysis of ITAS in the context of similar incidence should be weighted versus the advantage for the patients who effectively reduce HbA1c with self-management of BI. One might imagine that implementation of BI self-management by patients might reduce the barriers of access to this treatment, which is simple, efficacious and safe, but time-consuming for physicians and expensive for the healthcare system.
Of note, in the present study BMI was not associated with different risks of hypoglycaemia between patient- and physician-managed titration. However, a lower BMI was associated with greater risk of hypoglycaemia in the total ITAS population, i.e. both patient- and physician-managed groups, as recently indicated in a study where lower BMI and lower C-peptide were associated with higher risk of hypoglycaemia upon initiation of BI in insulin-naïve people [11].
A number of trials have compared patient- versus physician-managed titration of Gla-300 with results largely consistent with the ITAS study [4, 12, 13]. Among these studies, the TAKE CONTROL trial, which investigated a mixed population of insulin-naïve and insulin-treated patients who continued SU/glinides, also included a post hoc subgroup analysis [4]. In this study, in subgroup < 65 and ≥ 65 years of age there was no heterogeneity of treatment effect for either HbA1c reduction or incidence of any time hypoglycaemia, consistent with the results of the present ITAS subgroup analysis [14]. However, TAKE CONTROL did not report annualised rates of hypoglycaemia.
Limitations of the present study include the post hoc nature of the sub-analysis which remains an hypothesis-generating observation to be confirmed in ad hoc randomised controlled trials, and the numerical imbalance in the subgroups of eGFR (< vs. ≥ 60 ml/min/1.73 m2) and previous diabetes medication (metformin only, metformin + other and no prior metformin). Strength of this exploratory analysis derives from the clinical need to establish the applicability of the results of ITAS to subgroups of patients with quite different phenotypes, commonly observed in diabetes clinics. In this respect, the importance of subgroups analysis of glycaemic outcomes with BI initiation has recently been emphasised [15].
In conclusion, the present post hoc analysis of ITAS indicates that comparable glycaemic control and similarly low risk of hypoglycaemia were achieved with patient- and physician-managed Gla-300 titration, irrespective of assessed patient subgroups that were well balanced within treatment arms, except for the eGFR < 60 mL/min/1.73m2 and no prior metformin subgroups, which were noticeably smaller. A slightly higher rate of hypoglycaemia in the patient-managed arm than the physician-managed arm was detected in those with shorter disease duration, which deserves further investigation. Overall, the results suggest that in place of physician-managed titration of BI, patient-managed titration may be effective and generally safe across the several clinical varieties of T2DM phenotype. Thus, these findings agree with specific and effective reinforcement of diabetes self-management education and support [16] for earlier and more popular initiation and titration of BI.
Availability of data and material
Proposals relating to the data access should be directed to the corresponding author. To gain access, data requestors will need to sign a data access agreement.
Abbreviations
- BI:
-
Basal insulin
- BMI:
-
Body mass index
- Gla-300:
-
Insulin glargine 300 U/mL
- HbA1c :
-
Glycated haemoglobin
- GCP:
-
Good Clinical Practice
- ITAS:
-
Italian Titration Approach Study
- LMEM:
-
Linear mixed-effect model
- OADs:
-
Oral antihyperglycaemic drugs
- SU:
-
Sulphonylureas
- T2DM:
-
Type 2 diabetes
References
AMD. Evaluation of AMD indicators of quality of type 1 and 2 diabetes care in Italy. J AMD (2018). http://www.jamd.it/archivio-annali-amd/.
Russell-Jones D, Pouwer F, Khunti K (2018) Identification of barriers to insulin therapy and approaches to overcoming them. Diabetes Obes Metab 20:488–496
Captieux M, Pearce G, Parke HL, Epiphaniou E, Wild S, Taylor SJC et al (2018) Supported self-management for people with type 2 diabetes: a meta-review of quantitative systematic reviews. BMJ Open 8:e024262
Russell-Jones D, Dauchy A, Delgado E, Dimitriadis G, Frandsen HA, Popescu L et al (2019) Take control: a randomized trial evaluating the efficacy and safety of self- versus physician-managed titration of insulin glargine 300 U/mL in patients with uncontrolled type 2 diabetes. Diabetes Obes Metab 21:1615–1624
Bonadonna RC, Giaccari A, Buzzetti R, Perseghin G, Cucinotta D, Avogaro A et al (2020) Comparable efficacy with similarly low risk of hypoglycaemia in patient- versus physician-managed basal insulin initiation and titration in insulin-naïve type 2 diabetic subjects: the Italian Titration Approach Study (ITAS). Diabetes/Metabolism Res Rev 36:e3304
Bonadonna RC, Giaccari A, Buzzetti R, Aimaretti G, Cucinotta D, Avogaro A et al (2019) Italian Titration approach study (ITAS) with insulin glargine 300 U/mL in insulin-naive type 2 diabetes: design and population. Nutr Metab Cardiovasc Dis 29:496–503
Bolli GB, Wysham C, Fisher M, Chevalier S, Cali AMG, Leroy B et al (2019) A post-hoc pooled analysis to evaluate the risk of hypoglycaemia with insulin glargine 300 U/mL (Gla-300) versus 100 U/mL (Gla-100) over wider nocturnal windows in individuals with type 2 diabetes on a basal-only insulin regimen. Diabetes Obes Metab 21:402–407
Riddle MC, Bolli GB, Avogaro A, Gimenez Alvarez M, Merino-Trigo A, Boelle-Le Corfec E et al (2018) Assessment of hypoglycaemia during basal insulin therapy: Temporal distribution and risk of events using a predefined or an expanded definition of nocturnal events. Diabetes Metab 44:333–340
World Medical A (2013) World Medical Association Declaration of Helsinki. Ethical principles for medical research involving human subjects. https://www.wma.net/policies-post/wma-declaration-of-helsinkiethical-principles-for-medical-research-involving-human-subjects/
Owens DR, Landgraf W, Frier BM, Zhang M, Home PD, Meneghini L et al (2019) Commencing insulin glargine 100 U/mL therapy in individuals with type 2 diabetes: determinants of achievement of HbA1c goal less than 7.0. Diabetes Obes Metab 21:321–329
Bolli GB, Landgraf W, Bosnyak Z, Melas-Melt L, Home PD (2020) Hypoglycaemia risk with insulin glargine 300 U/mL compared with glargine 100 U/mL across different baseline fasting C-peptide levels in insulin-naive people with type 2 diabetes: A post hoc analysis of the EDITION 3 trial. Diabetes Obes Metab 22:1664–1669
Davies M, Bain S, Charpentier G, Flacke F, Goyeau H, Woloschak M et al (2019) A randomized controlled, treat-to-target study evaluating the efficacy and safety of insulin glargine 300 U/mL (Gla-300) administered using either device-supported or routine titration in people with type 2 diabetes. J Diabetes Sci Technol 13:881–889
Bajaj HS, Venn K, Ye C, Aronson R (2016) Randomized trial of long-acting insulin glargine titration web tool (LTHome) versus enhanced usual therapy of glargine titration (INNOVATE Trial). Diabetes Technol Ther 18:610–615
Strojek K, Bigot G, Bonnemaire M, Delgado E, Donicova V, Kvapil M et al (2018) Improved or comparable efficacy without increased hypoglycaemia with self- versus physician-led titration of insulin glargine 300 U/ml in age groups <65 or ≥65 years: TAKE CONTROL. Diabetologia 61(Suppl 1):S443
Haluzik M, Cheng A, Muller-Wieland D, Westerbacka J, Bosnyak Z, Lauand F et al (2020) Differential glycaemic control with basal insulin glargine 300 U/mL versus degludec 100 U/mL according to kidney function in type 2 diabetes: a subanalysis from the BRIGHT trial. Diabetes Obes Metab 22:1369–1377
Davies MJ, D’Alessio DA, Fradkin J, Kernan WN, Mathieu C, Mingrone G et al (2018) Management of hyperglycaemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 61:2461–2498
Acknowledgements
The authors thank the study participants, trial staff and investigators for their participation.
Funding
Open Access funding provided by Università Cattolica del Sacro Cuore. This work was supported by Sanofi, Milan, Italy. Editorial assistance was provided by Fishawack Communications Ltd., funded by Sanofi.
Author information
Authors and Affiliations
Contributions
AG, RCB, RB, GP, DC, CF, AA, GA and GBB participated as investigators and provided comments and input to all drafts of the manuscript and interpretation of the results. ML and VP provided comments and input to all drafts of the manuscript and interpretation of the results. All authors approved the final version to be published and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
Andrea Giaccari has received honoraria or consulting fees from Amgen, AstraZeneca, Boehringer Ingelheim, Eli Lilly, MSD, Sanofi and research funding from AstraZeneca. Riccardo C. Bonadonna has received honoraria or consulting fees from Sanofi, Merck Sharp & Dohme, Eli Lilly, Johnson & Johnson, Bristol-Myers Squibb, AstraZeneca and Janssen. Raffaella Buzzetti has received honoraria or consulting fees from Sanofi, Eli Lilly, AstraZeneca, Abbott and Novo Nordisk. Gianluca Perseghin has received honoraria or consulting fees from Novo Nordisk, Sanofi, Eli Lilly, AstraZeneca, Boehringer Ingelheim, Takeda, Abbott, Janssen and Merck Sharp & Dohme. Domenico Cucinotta has received honoraria or consulting fees from Eli Lilly, Novo Nordisk, Roche Diagnostics and Sanofi. Carmine Fanelli has received honoraria or consulting fees from Sanofi and non-financial support from Menarini. Angelo Avogaro has received honoraria or consulting fees from Novo Nordisk, Sanofi, Eli Lilly, AstraZeneca, Boehringer Ingelheim, Takeda and Servier and research funding from AstraZeneca and Vifor Pharma. Gianluca Aimaretti has received honoraria or consulting fees from Sanofi, AstraZeneca, IBSA Institut Biochimique and Novartis and research funding from Sanofi, AstraZeneca and Novo Nordisk. Monica Larosa is an employee of Sanofi and holds stocks/shares in Sanofi. Veronica Pagano is an employee of a CRO (OPIS s.r.l.) contracted by Sanofi. Geremia B. Bolli has received honoraria or consulting fees from Sanofi and Menarini and research funding and speakers’ bureau fees from Sanofi.
Ethical approval
The clinical trial protocol was approved by the appropriate local ethics committees and IRB/IEC. The study was conducted in accordance with the Declaration of Helsinki and the ICH guidelines for Good Clinical Practice (GCP).
Consent to participate
All participants provided written informed consent.
Consent for publication
All authors have reviewed the content of this manuscript and provided consent for publication.
Additional information
Managed By Massimo Porta.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Giaccari, A., Bonadonna, R.C., Buzzetti, R. et al. Similar glycaemic control and risk of hypoglycaemia with patient- versus physician-managed titration of insulin glargine 300 U/mL across subgroups of patients with T2DM: a post hoc analysis of ITAS. Acta Diabetol 58, 789–796 (2021). https://doi.org/10.1007/s00592-021-01675-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-021-01675-0