Abstract
Aims
Gestational diabetes mellitus (GDM) occurs in 5–15% of pregnancies, and lower maternal educational attainment has been associated with higher risk of GDM. We aimed to determine if maternal education level is associated with persistent post-partum glucose metabolism disorders in women with GDM.
Methods
Retrospective cohort study of women with GDM followed in 25 Portuguese health institutions between 2008 and 2012. Educational attainment was categorised into four levels. Prevalence of post-partum glucose metabolism disorders (type 2 diabetes mellitus, increased fasting plasma glucose or impaired glucose tolerance) was compared and adjusted odds ratios calculated controlling for confounders using logistic regression.
Results
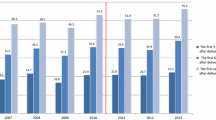
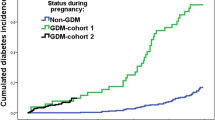
We included 4490 women diagnosed with GDM. Educational level ranged as follows: 6.8% (n = 307) were at level 1 (≤ 6th grade), 34.6% (n = 1554) at level 2 (6–9th grade), 30.4% (n = 1364) at level 3 (10–12th grade) and 28.2% (n = 1265) at level 4 (≥ university degree). At 6 weeks post-partum re-evaluation, 10.9% (n = 491) had persistent glucose metabolism disorders. Educational levels 1 and 2 had a higher probability of persistent post-partum glucose metabolism disorders when compared to level 4 (OR = 2.37 [1.69;3.32], p < 0.001 and OR = 1.39 [1.09;1.76], p = 0.008, for level 1 and 2, respectively), an association that persisted in multivariable logistic regression adjusting for confounders (level 1 OR = 2.25 [1.53;3.33], p < 0.001; level 2 OR = 1.43 [1.09;1.89], p = 0.01).
Conclusions
Persistent post-partum glucose metabolism disorders are frequent in women with GDM and associated with lower maternal educational level. Interventions aimed at this risk group may contribute towards a decrease in prevalence of post-partum glucose metabolism disorders.



Similar content being viewed by others
References
Kampmann U, Madsen LR, Skajaa GO, Iversen DS, Moeller N, Ovesen P (2015) Gestational diabetes: a clinical update. World J Diabetes 6(8):1065–1072. https://doi.org/10.4239/wjd.v6.i8.1065
Metzger BE, Lowe LP, Dyer AR, Trimble ER, Chaovarindr U, Coustan DR et al (2008) Hyperglycemia and adverse pregnancy outcomes. N Engl J Med 358(19):1991–2002. https://doi.org/10.1056/NEJMoa0707943
Di Cianni G, Miccoli R, Volpe L, Lencioni C, Del Prato S (2003) Intermediate metabolism in normal pregnancy and in gestational diabetes. Diabetes Metab Res Rev 19(4):259–270. https://doi.org/10.1002/dmrr.390
Gorgal R, Goncalves E, Barros M, Namora G, Magalhaes A, Rodrigues T et al (2012) Gestational diabetes mellitus: a risk factor for non-elective cesarean section. J Obstet Gynaecol Res 38(1):154–159. https://doi.org/10.1111/j.1447-0756.2011.01659.x
Mitanchez D, Yzydorczyk C, Simeoni U (2015) What neonatal complications should the pediatrician be aware of in case of maternal gestational diabetes? World J Diabetes 6(5):734–743. https://doi.org/10.4239/wjd.v6.i5.734
Simeoni U, Barker DJ (2009) Offspring of diabetic pregnancy: long-term outcomes. Semin Fetal Neonatal Med 14(2):119–124. https://doi.org/10.1016/j.siny.2009.01.002
Yogev C, Hod C, Oats M et al (2010) Hyperglycemia and Adverse Pregnancy Outcome (HAPO) study: preeclampsia. Am J Obstet Gynecol 202(3):255 e1–255 e7. https://doi.org/10.1016/j.ajog.2010.01.024
Kim C, Newton KM, Knopp RH (2002) Gestational diabetes and the incidence of type 2 diabetes: a systematic review. Diabetes Care 25(10):1862–1868
Expert Committee on the Diagnosis and Classification of Diabetes Mellitus (2003) Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care 26(Suppl 1):S5–S20. https://doi.org/10.2337/diacare.26.2007.S5
Grundy SM, Benjamin IJ, Burke GL, Chait A, Eckel RH, Howard BV et al (1999) Diabetes and cardiovascular disease: a statement for healthcare professionals from the American Heart Association. Circulation 100(10):1134–1146
Nathan DM, Davidson MB, DeFronzo RA, Heine RJ, Henry RR, Pratley R et al (2007) Impaired fasting glucose and impaired glucose tolerance: implications for care. Diabetes Care 30(3):753–759. https://doi.org/10.2337/dc07-9920
Lee AJ, Hiscock RJ, Wein P, Walker SP, Permezel M (2007) Gestational diabetes mellitus: clinical predictors and long-term risk of developing type 2 diabetes: a retrospective cohort study using survival analysis. Diabetes Care 30(4):878–883. https://doi.org/10.2337/dc06-1816
Magliano DJ, Barr EL, Zimmet PZ, Cameron AJ, Dunstan DW, Colagiuri S et al (2008) Glucose indices, health behaviors, and incidence of diabetes in Australia: the Australian Diabetes, Obesity and Lifestyle Study. Diabetes Care 31(2):267–272. https://doi.org/10.2337/dc07-0912
Bouthoorn SH, Silva LM, Murray SE, Steegers EA, Jaddoe VW, Moll H et al (2015) Low-educated women have an increased risk of gestational diabetes mellitus: the Generation R Study. Acta Diabetol 52(3):445–452. https://doi.org/10.1007/s00592-014-0668-x
Carpenter MW, Coustan DR (1982) Criteria for screening tests for gestational diabetes. Am J Obstet Gynecol 144(7):768–773
World Health Organization (2014) Diagnostic criteria and classification of hyperglycaemia first detected in pregnancy: a World Health Organization Guideline. Diabetes Res Clin Pract 103(3):341–363. https://doi.org/10.1016/j.diabres.2013.10.012
Metzger BE, Gabbe SG, Persson B, Buchanan TA, Catalano PA, Damm P et al (2010) International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care 33(3):676–682. https://doi.org/10.2337/dc09-1848
Rasmussen KM, Yaktine AL (eds) (2009) Weight gain during pregnancy—reexamining the guidelines. Washington (DC): National Academies Press (US)
Dores JM, Magalhães A, Carvalheiro M (2017) Relatório de Consenso sobre a Diabetes e Gravidez. Portuguese General-Directorate of Health. 2011. http://www.saudereprodutiva.dgs.pt/ficheiros-de-upload-diversos/relatorio-de-consenso-pdf.aspx
Ferrara A, Peng T, Kim C (2009) Trends in postpartum diabetes screening and subsequent diabetes and impaired fasting glucose among women with histories of gestational diabetes mellitus: a report from the Translating Research Into Action for Diabetes (TRIAD) Study. Diabetes Care 32(2):269–274. https://doi.org/10.2337/dc08-1184
Bennett WL, Ennen CS, Carrese JA, Hill-Briggs F, Levine DM, Nicholson WK et al (2011) Barriers to and facilitators of postpartum follow-up care in women with recent gestational diabetes mellitus: a qualitative study. J Womens Health (Larchmt) 20(2):239–245. https://doi.org/10.1089/jwh.2010.2233
Pastore I, Chiefari E, Vero R, Brunetti A (2017) Postpartum glucose intolerance: an updated overview. Endocrine. https://doi.org/10.1007/s12020-017-1388-0
White IR, Royston P, Wood AM (2011) Multiple imputation using chained equations: issues and guidance for practice. Stat Med 30(4):377–399. https://doi.org/10.1002/sim.4067
Coustan DR, Carpenter MW, O’Sullivan PS, Carr SR (1993) Gestational diabetes: predictors of subsequent disordered glucose metabolism. Am J Obstet Gynecol 168(4):1139–1144 (discussion 44–5)
Kjos SL, Buchanan TA, Greenspoon JS, Montoro M, Bernstein GS, Mestman JH (1990) Gestational diabetes mellitus: the prevalence of glucose intolerance and diabetes mellitus in the first two months post partum. Am J Obstet Gynecol 163(1 Pt 1):93–98
Schaefer-Graf UM, Buchanan TA, Xiang AH, Peters RK, Kjos SL (2002) Clinical predictors for a high risk for the development of diabetes mellitus in the early puerperium in women with recent gestational diabetes mellitus. Am J Obstet Gynecol 186(4):751–756
Nielsen LR, Ekbom P, Damm P, Glumer C, Frandsen MM, Jensen DM et al (2004) HbA1c levels are significantly lower in early and late pregnancy. Diabetes Care 27(5):1200–1201
Wild S, Roglic G, Green A, Sicree R, King H (2004) Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care 27(5):1047–1053
Karve A, Hayward RA (2010) Prevalence, diagnosis, and treatment of impaired fasting glucose and impaired glucose tolerance in nondiabetic U.S. adults. Diabetes Care 33(11):2355–2359. https://doi.org/10.2337/dc09-1957
American Diabetes Association (2015) 5. Prevention or delay of type 2 diabetes. Diabetes Care 38(Suppl 1):S31–S32. https://doi.org/10.2337/dc15-S008
Acknowledgements
We thank the multidisciplinary teams of obstetricians and diabetologists of Portuguese health institutions who collected patient data for the National Registry of Gestational Diabetes. In addition, we would like to acknowledge the alumni and faculty of the Harvard Medical School—Portugal Clinical Scholars Research Training Programme for useful scientific discussions. DP was partially supported by Fundação para a Ciência e Tecnologia under the Program for doctoral training in clinical research for medical interns (SFRH/SINT/95317/2013).
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
All procedures in this study were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
For this type of study using retrospective and anonymised data, participants’ written consent was not required.
Additional information
Managed by Massimo Federici.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gante, I., Ferreira, A.C., Pestana, G. et al. Maternal educational level and the risk of persistent post-partum glucose metabolism disorders in women with gestational diabetes mellitus. Acta Diabetol 55, 243–251 (2018). https://doi.org/10.1007/s00592-017-1090-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-017-1090-y