Abstract
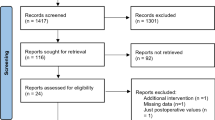
The aim of the present study was to summarize the effectiveness of amino acid supplementation on muscle strength, muscle volume, and functional capacity in patients undergoing total knee arthroplasty. For this, in November 2022, a search was carried out in the PubMed, Cochrane Library, and EMBASE databases, identifying a total of 2182 documents, of which only 4 were included in the present review. The included studies had 148 participants (47 men and 101 women), with a minimum age of 53 and a maximum of 92 years, and supplementation times of 13 to 30 days (1 to 3 times a day). For the results, in relation to muscle performance, when comparing the control and experimental groups, greater muscle atrophy was observed in the pre- and post-moments of the control group, in relation to the experimental group. In addition, studies suggest a good tendency for muscle mass gain, and improvement in the functional capacities of patients who used supplementation. Therefore, the use of amino acids after TKA surgery reduces muscle atrophy, which preserves muscle mass and leads to better performance in tests of strength and functional capacity, when compared to the use of a placebo.

Similar content being viewed by others
References
Le Stum M, Gicquel T, Dardenne G, Le Goff-Pronost M, Stindel E, Clavé A (2022) Total knee arthroplasty in France: male-driven rise in procedures in 2009–2019 and projections for 2050. Orthop Traumatol Surg Res 109:103463
Grazina R, Andrade R, Bastos R et al (2018) Clinical management in early OA. Adv Exp Med Biol 1059:111–135
Richards MM, Maxwell JS, Weng L, Angelos MG, Golzarian J (2016) Intra-articular treatment of knee osteoarthritis: from anti-inflammatories to products of regenerative medicine. Phys Sportsmed 44(2):101–108
Komatsu DE, Uddin SMZ, Gordon C et al (2022) Acute postoperative pain and dorsal root ganglia transcriptomic signatures following total knee arthroplasty (TKA) in rats: an experimental study. PLoS ONE 17(12):e0278632
Bakırhan S, Unver B, Elibol N, Karatosun V (2022) Fear of movement and other associated factors in older patients with total knee arthroplasty. Ir J Med Sci 192(5):2217
Paravlic AH, Meulenberg CJ, Drole K (2022) The time course of quadriceps strength recovery after total knee arthroplasty is influenced by body mass index, sex, and age of patients: systematic review and meta-analysis. Front Med 9:865412
Paravlic AH, Kovač S, Pisot R, Marusic U (2020) Neurostructural correlates of strength decrease following total knee arthroplasty: a systematic review of the literature with meta-analysis. Bosn J basic Med Sci 20(1):1–12
Christensen JC, Mizner RL, Foreman KB, Marcus RL, Pelt CE, LaStayo PC (2018) Quadriceps weakness preferentially predicts detrimental gait compensations among common impairments after total knee arthroplasty. J Orthop Res 36(9):2355–2363
Labanca L, Bonsanto F, Raffa D, Orlandi Magli A, Benedetti MG (2022) Does adding neuromuscular electrical stimulation to rehabilitation following total knee arthroplasty lead to a better quadriceps muscle strength recovery? A systematic review. Int J Rehabil 45(2):118–125
Skoffer B, Maribo T, Mechlenburg I, Hansen PM, Søballe K, Dalgas U (2016) Efficacy of preoperative progressive resistance training on postoperative outcomes in patients undergoing total knee arthroplasty. Arthritis Care Res (Hoboken) 68(9):1239–1251
Burgess LC, Phillips SM, Wainwright TW (2018) What is the role of nutritional supplements in support of total hip replacement and total knee replacement surgeries? A systematic review. Nutrients 10(7):820
Dreyer HC, Volpi E (2005) Role of protein and amino acids in the pathophysiology and treatment of sarcopenia. J Am Coll Nutr 24(2):140S-145S
Boese CK, Centeno L, Walters RW (2017) Blood conservation using tranexamic acid is not superior to epsilon-aminocaproic acid after total knee arthroplasty. J Bone Jt Surg Am 99(19):1621–1628
Churchill JL, Puca KE, Meyer E, Carleton M, Anderson MJ (2017) Comparing ε-aminocaproic acid and tranexamic acid in reducing postoperative transfusions in total knee arthroplasty. J Knee Surg 30(5):460–466
Li Z, Sun X, Li W, Zhang M (2021) Tranexamic acid versus epsilon-aminocaproic acid in total knee arthroplasty: a meta-analysis. J Healthc Eng. https://doi.org/10.1155/2021/1758066
Wormald R, Evans J (2018) What makes systematic reviews systematic and why are they the highest level of evidence? Ophthalmic Epidemiol 25(1):27–30
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71
Curtis BM, Barrett BJ, Parfrey PS (2021) Randomized controlled trials 1: design. Methods Mol Biol 2249:193–211
Cumpston M, Li T, Page MJ et al (2019) Updated guidance for trusted systematic reviews a new edition of the cochrane handbook for systematic reviews of interventions. In: Cochrane Database Systematic Reviews. 10: ED000142
Gagnier JJ, Mullins M, Huang H et al (2017) A systematic review of measurement properties of patient-reported outcome measures used in patients undergoing total knee arthroplasty. J Arthroplast 32(5):1688-1697.e7
Reynaud V, Verdilos A, Pereira B, Boisgard S, Costes F, Coudeyre E (2020) Core outcome measurement instruments for clinical trials of total knee arthroplasty: a systematic review. J Clin Med 9(8):2439
Ma L-L, Wang Y-Y, Yang Z-H, Huang D, Weng H, Zeng X-T (2020) Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: what are they and which is better? Mil Med Res 7(1):7
Moseley AM, Rahman P, Wells GA et al (2019) Agreement between the cochrane risk of bias tool and physiotherapy evidence database (PEDro) scale: a meta-epidemiological study of randomized controlled trials of physical therapy interventions. PLoS ONE 14(9):e0222770
Foley NC, Bhogal SK, Teasell RW, Bureau Y, Speechley MR (2006) Estimates of quality and reliability with the physiotherapy evidence-based database scale to assess the methodology of randomized controlled trials of pharmacological and nonpharmacological interventions. Phys Ther 86(6):817–824
Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M (2003) Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther 83(8):713–721
Ueyama H, Kanemoto N, Minoda Y, Taniguchi Y, Nakamura H, Chitranjan S (2020) Ranawat Award: perioperative essential amino acid supplementation suppresses rectus femoris muscle atrophy and accelerates early functional recovery following total knee arthroplasty: a prospective double-blind randomized controlled tri. Bone Joint J. https://doi.org/10.1302/0301-620X.102B6.BJJ-2019-1370.R1
Roy BD, de Beer J, Harvey D, Tarnopolsky MA (2005) Creatine monohydrate supplementation does not improve functional recovery after total knee arthroplasty. Arch Phys Med Rehabil 86(7):1293–1298
Nishizaki K, Ikegami H, Tanaka Y, Imai R, Matsumura H (2015) Effects of supplementation with a combination of ß-hydroxy-ß-methyl butyrate, L-arginine, and L-glutamine on postoperative recovery of quadriceps muscle strength after total knee arthroplasty. Asia Pac J Clin Nutr 24(3):412–420
Dreyer HC, Strycker LA, Senesac HA et al (2013) Clinical medicine essential amino acid supplementation in patients following total knee arthroplasty. J Clin Investig 123(11):4654
Dideriksen K, Reitelseder S, Holm L (2013) Influence of amino acids, dietary protein, and physical activity on muscle mass development in humans. Nutrients 5(3):852–876
Millward DJ (2003) An adaptive metabolic demand model for protein and amino acid requirements. Br J Nutr 90(2):249–260
Dreyer HC, Owen EC, Strycker LA et al (2018) Essential amino acid supplementation mitigates muscle atrophy after total knee arthroplasty: a randomized, double-blind, placebo-control trial. JBJS Open Access 3(2):e0006
Brown K, Kachelman J, Topp R et al (2009) Predictors of functional task performance among patients scheduled for total knee arthroplasty. J Strength Cond Res 23(2):436–443
Funding
This study had no financial support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors declare that they have no conflict of interest.
Ethical approval
As this is a systematic review, an Ethics Committee was not required for this type of study. We are carrying out an ECR on the subject, this one with an approved Ethics Committee.
Informed consent
As this is a systematic review, an Informed Consent was not required for this type of study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
de Souza Borges, J.H., Junior, P.L., de Brito, F.F. et al. Effects of amino acid supplementation on muscle mass, muscle performance and functional capacity in subjects undergoing total knee arthroplasty: a systematic review of randomized clinical trials. Eur J Orthop Surg Traumatol 34, 1717–1729 (2024). https://doi.org/10.1007/s00590-023-03824-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-023-03824-3