Abstract
Background
Acute total hip arthroplasty (THA) may be an alternative or an adjuvant to internal fixation for surgical treatment of acetabular fractures. We investigate recent trends in the operative management of acetabular fractures. We hypothesize that the incidence of acute THA for acetabular fractures has increased over time.
Methods
4569 middle-aged (45–64 years) and older adults (≥ 65 years) who received acute operative management of an acetabular fracture within 3 weeks of admission between 2010 and 2020 were identified from the United States Nationwide Inpatient Sample database. Treatment was classified as open reduction internal fixation (ORIF), THA, or combined ORIF and THA (ORIF + THA). Patients were stratified by age ≥ 65 years old. Associations between demographic factors and the incidence of each procedure over the study period were modeled using linear regression.
Results
The relative incidence of treatments was 80.9% ORIF, 12.1% THA, and 7.0% ORIF + THA. Among patients aged 45–64 years old, THA increased 4.8% [R2 = 0.62; β1 = 0.6% (95% Confidence Interval (CI) 0.2–0.9%)] and ORIF + THA increased 2.6% [R2 = 0.73; β1 = 0.3% (95% CI 0.2–0.4%)], while the use of ORIF decreased 7.4% [R2 = 0.75; β1 = −0.9% (95% CI −1.2 to −0.5%)]. Among patients ≥ 65 years old, THA increased 16.5% [R2 = 0.87; β1 = 1.7% (95% CI 1.2–2.2%)] and ORIF + THA increased 5.0% [R2 = 0.38, β1 = 0.6% (95% CI 0.0–1.3%)], while ORIF decreased 21.5% [R2 = 0.75; β1 = −2.4% (95% CI −3.45 to −1.3%)].
Conclusion
The treatment of acetabular fractures with acute THA has increased in the last decade, particularly among older adults.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acetabular fractures in older patients are occurring more frequently and are associated with high rates of mortality and non-fatal complications [1,2,3]. These older patients often have pre-existing hip osteoarthritis, osteoporosis, and fracture characteristics predictive of post-traumatic arthritis [4, 5]. Surgical treatment options for older patients with acetabular fracture include open reduction internal fixation (ORIF), total hip arthroplasty (THA), or the combined used of ORIF and THA (ORIF + THA) [6, 7].
While ORIF has been the historical standard of care [6, 8, 9], recent evidence suggests that acute THA may provide better functional outcomes with fewer reoperations in older patients with acetabular fracture [10,11,12,13,14,15,16,17]. It is not known whether surgeons who treat acetabular fractures have changed their practice to perform arthroplasty more frequently. Our purpose is to investigate if the acute use of THA for acetabular fractures in middle-aged and older adults—patients for whom an elective total hip arthroplasty would represent a reasonable intervention for osteoarthritis—has increased over time. We hypothesize that the relative incidence of THA and ORIF + THA have increased in the last decade compared with ORIF as a standard of care. We further characterize facility, patient, and fracture characteristics that may be associated with the choice to manage acetabular fracture with THA as a primary treatment or with adjunctive ORIF.
Materials and methods
Data source
Adults ≥ 45 years of age treated for acetabular fracture within 3 weeks of admission between 2010 through 2020 were retrospectively identified from the Nationwide Inpatient Sample (NIS). The NIS is curated by the Healthcare Cost and Utilization Project (HCUP) and includes data on over 7 million hospital discharges per year [18, 19]. In 2012 the NIS included a 20% stratified sample of inpatient admissions across the United States, while prior to 2012 the NIS sampled 20% of discharges from participating hospitals. This methodologic change was intended to improve the precision of national estimates by reducing sampling error [20]. Deidentified publicly available data were used for this investigation, thus this study was exempt from Institutional Review Board review.
Study population
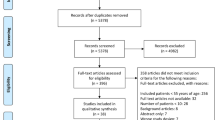
International Classification of Diseases Ninth Edition Clinical Modification (ICD-9-CM) and Tenth Edition Clinical Modification (ICD-10-CM) codes were used to identify patients with acetabular fractures (Supplementary Table S1). Operative treatments including open reduction internal fixation (ORIF), total hip arthroplasty (THA), and combined ORIF and THA (ORIF + THA) were identified using ICD-9 and ICD-10 procedure codes (PCS; Supplementary Table S2). Patients < 45 years old and those without recorded operative procedure or procedures > 3 weeks after admission were excluded to capture patients with acute injuries and those who are most likely to benefit from and be treated by acute THA [21,22,23].
A weighted sample estimate representing 22,795 adults met inclusion criteria (Supplementary Fig. S1). The relative incidence of each treatment was 80.9% ORIF, 12.1% THA, and 7.0% ORIF + THA. Patients receiving each treatment significantly differed by age, sex, insurance type, hospital size, hospital type, and comorbidities overall (Tables 1, 2, Supplemental Table S3-S4).
Study outcomes
The primary outcome was annual change in the incidence of ORIF, THA, and ORIF + THA. Secondary outcomes included hospital length of stay and national charge estimates for cost of hospital stay.
Statistical methods
Annual procedure incidence was modeled using linear regression on proportional changes in yearly cases. Patients were stratified by age 45–64 years (middle-aged) or ≥ 65 years (older adult). Further subgroup analysis considered the effects of sex and insurance type within age groups on treatment. Chow tests were conducted to determine differences in linear regression coefficients β across groups. Adjusted R2 was used to determine goodness-of-fit. Continuous and categorical variables were compared across unweighted treatment groups using one way analysis of variance and chi-squared, respectively. National charge estimates for hospital stay were derived using the NIS discharge weighting scheme which reflects a ratio of national discharges to discharges captured by NIS. Statistical analyses were performed using Stata Version 17.0 (College, Station, TX), reporting 2-sided p values with the level of significance for p < 0.050.
Results
Treatment by age
For patients aged ≥ 65 years, 5860 (65.8%) underwent ORIF, 1844 (20.8%) underwent THA, and 1162 (13.1%) underwent ORIF + THA. For patients aged 45–64 years, 12,588 (90.4%) underwent ORIF, 906 (6.5%) underwent THA, and 435 (3.1%) underwent ORIF + THA. We observed greater overall use of THA (20.8%) and ORIF + THA (13.1%) for patients ≥ 65 years with acetabular fracture versus greater use of ORIF (90.4%) in the 45–64 group (Table 1). The mean age of the ≥ 65 group was 76.1 years (95% confidence interval (CI) 75.8–76.5 years), with those undergoing ORIF (75.5 years; 95% CI 75.0–75.9 years) being significantly younger than those undergoing THA (77.6 years; 95% CI 77.6–78.3 years) or ORIF + THA (77.2 years; 95% CI 76.3–78.0 years) (p < 0.001) (Table 1). The mean age of the 45–64 group was 54.9 years (95% CI 54.7–55.1 years), with significantly younger patients undergoing ORIF (54.6 years; 54.3–54.8 years) than those undergoing THA (57.6 years; 95% CI 56.7–58.4 years) or ORIF + THA (58.9 years; 95% CI 57.8–60.0 years) (Table 2).
Treatment trends by age
We observed an increase in the use of THA for acetabular fracture over the study period in middle-aged and older adults. From 2010 to 2020, the use of ORIF for patients ≥ 65 years decreased 21.5% [R2 = 0.75; β1 = −2.4% per year (95% CI −3.4 to −1.3%)], while THA increased 16.5% [R2 = 0.87; β1 = 1.7% per year (95% CI 1.2–2.2%)] and ORIF + THA increased 5.0% [R2 = 0.38, β1 = 0.6% per year (95% CI 0.0–1.3%)] (Fig. 1a). Among patients aged 45–64 years, the use of ORIF decreased 7.4% [R2 = 0.75; β1 = −0.9% per year (95% CI −1.2 to −0.5%)], while THA increased 4.8% [R2 = 0.62; β1 = 0.6% per year (95% CI 0.2–0.9%)] and ORIF + THA increased 2.6% [R2 = 0.73; β1 = 0.3% per year (95% CI 0.2–0.4%)], (Fig. 1b). Annual rates of change in practice were significantly different between age groups for ORIF (p < 0.001) and THA (p < 0.001), but not for ORIF + THA (p > 0.05).
Treatment trends by sex
Patient sex was associated with changes in practice over time. Acute THA for acetabular fracture significantly increased over time among women ≥ 65 years [R2 = 0.68; β1 = 2.5% per year (95% CI 1.2–3.8%)]. Treatment by ORIF and ORIF + THA did not change over time among women ≥ 65 years. No temporal change of practice was observed among men [R2 = 0.24; β1 = 0.5% per year (95% CI −0.2 to 1.2%); p = 0.002; Fig. 2a, b]. No differences in treatment by sex were observed over time among patients aged 45–64 years (p > 0.05; Fig. 2c, d).
Acetabular treatment trends by open reduction internal fixation (black), total hip arthroplasty (dark grey), and open reduction internal fixation + total hip arthroplasty (light grey) in the NIS database from 2010 to 2020. A males in ages ≥ 65. B Females in ages ≥ 65. C Males in ages 45–64. d Females in ages 45–64
Treatment trends by insurance type
Medicare insurance status was associated with the greatest growth in use of THA in acetabular fracture among patients aged ≥ 65 years [R2 = 0.80; β1 = 2.0% per year (95% CI = 1.2–2.7%) vs R2 = 0.14; β1 = 0.6% per year (95% CI = −0.5 to 1.6%); p = 0.006]. Additionally, the relative use of ORIF declined more rapidly over time in the Medicare insured patients (R2 = 0.67; β1 = −3.0% per year (95% CI = −4.7 to −1.4%)) when compared to non-Medicare insured patients [R2 = 0.15; β1 = −0.6% per year (95% CI = −1.7–0.5%); p = 0.03]. No differences in longitudinal ORIF + THA use rates were observed between insurance groups (p > 0.05; Fig. 3a, b). Insurance type was not significantly associated with treatment in patients aged 45–64 years (p > 0.05; Fig. 3c, d).
Acetabular treatment trends by open reduction internal fixation (black), total hip arthroplasty (dark grey), and open reduction internal fixation + total hip arthroplasty (light grey) in the NIS database from 2010 to 2020. A Medicare insured in ages ≥ 65. B Non-Medicare insured in ages ≥ 65. C Privately insured in ages 45–64. d Non-privately insured in ages 45–64
Treatment trends by hospital type
Hospital type was associated with treatment but not significantly associated with changes in practice over time. The incidence of THA and THA + ORIF increased over time in rural, urban non-teaching, and urban teaching hospitals over time, but the rates of practice change were not significantly different across hospital types among patients aged ≥ 65 years (Supplementary Fig. S2a–S3c) or patients 45–64 years old (Supplementary Fig. S2d–S3f).
Trends in length of stay by treatment
Length of stay was significantly shorter among patients who received THA [6.4 days (95% CI 5.8–7.0 days)] versus patients who received ORIF [9.7 days (95% CI 9.4–9.9 days); p < 0.001) or ORIF + THA (8.2 days (95% CI 7.3–9.0 days); p = 0.004]. Length of stay did not significantly vary over time by procedure among patients ≥ 65 years old with acetabular fracture (Fig. 4a). In patients aged 45–64 years, the overall hospital length of stay decreased over time for ORIF [R2 = 0.65; β1 = −0.17 days per year (95% CI −0.27 to −0.01 days)] but remained unchanged for both THA [R2 = 0.05; β1 = −0.11 days per year (95% CI = −0.5, to 0.27 days)] and ORIF + THA [R2 = 0.24; β1 = −0.22 days per year (95% CI −0.5 to 0.1 days)] (Fig. 4b).
Trends in estimated charges by treatment
National estimated hospital charges were significantly lower in patients who received THA [$112,591.40 (95% CI $104,912.40–$120,270.40)] compared to patients who received ORIF [$143,542.80 (95% CI $138,922.50–$148,163.10)] (p < 0.001) and ORIF + THA [$159,730.10 (95% CI $144,901.70–$174,558.60)] (p < 0.001). In patients ≥ 65 years old, the cost of both ORIF [R2 = 0.47; β1 = $2285.59 per year (95% CI $456.96–$4114.22)] and ORIF + THA [R2 = 0.37; β1 = $5308.89 per year (95% CI $75.24–$10,542.53)] increased significantly per year, while the cost of THA [R2 = 0.01; β1 = $550.01 per year (95% CI −$3844.19–$4944.22)] did not change (Fig. 5a). In patients 45–64 years old, no differences in cost of ORIF [R2 = 0.19; β1 = $1762.39 per year (95% CI −$1062.08–$4586.87)], THA [R2 = 0.13; β1 = $2,272.71 per year (95% CI −$2234.15–$6779.56)], or ORIF + THA [R2 = 0.00; β1 = $245.90 per year (95% CI −$7443.65–$7935.46)] were observed over time (Fig. 5b).
Discussion
We observed substantial practice changes in the surgical management of middle-aged and older US adults with acetabular fracture between 2010 and 2020 in the Nationwide Inpatient Sample. Among older adults aged ≥ 65 years, the incidence of THA and ORIF + THA increased 16.5% and 5.0%, respectively, while the use of ORIF decreased by 21.5%. Practice changes were less substantial among middle-aged adults aged 45–64 years: the incidence of THA and ORIF + THA increased 4.8% and 2.6%, respectively, while the use of ORIF decreased 7.4%. The practice of acute THA for acetabular fracture grew 1.6% annually among older adults and 0.6% annually among middle-aged adults. To our knowledge, these novel observations reflect progressive adoption of arthroplasty for acetabular fractures in middle-aged and older adults.
Acetabular fractures in older adults incur substantial morbidity, disability, and healthcare costs [2, 3]. The adoption of acute THA as either a primary treatment or combined with adjunctive ORIF may reflect a response by surgeons to contemporary evidence for benefits to arthroplasty over ORIF alone in older patients. In a recent systematic review on the outcomes following acetabular fracture in 3928 patients aged 55–99 years, McCormick et al. found ORIF was associated with 2.2 greater odds of non-fatal complications versus THA and a pooled 15% rate of conversion to THA after ORIF at a mean of 29.4 months [12]. Although early reports of ORIF + THA have reported concerning rates of heterotopic ossification, dislocation, and other mechanical failures, single center series suggest improved survival with low rates of reoperation [7, 24]. Manson et al. prospectively randomized 47 patients over age 60 to either ORIF or ORIF + THA and reported a 28% absolute risk reduction in overall reoperations and 12% greater Harris Hip score with no dislocations in either group within 2 years [22]. Borg et al. found improved three-year hip survival in patients undergoing ORIF + THA when compared to ORIF alone [13]. Lin et al. noted equivalent functional outcomes to patients undergoing primary THA for osteoarthritis with a 15% complication rate [17]. However, Kelly et al. identified a 27% surgical complication rate, 13% medical complication rate, and 18% all cause revision risk in a recent review of insurance claims data [25]. These studies provide compelling, if tempered, support for the use of arthroplasty to treat acetabular fractures with a reasonable probability of a favorable outcome in older patients [24].
ORIF remains widely regarded as the standard of care for younger patients with displaced or minimally-displaced but unstable acetabular fractures. We did not observe a clinically relevant change—a minimal 0.9% decline—in the incidence of ORIF for acetabular fracture in middle-aged patients aged 45–64 years. Younger and middle-aged adults experience excellent hip survival and functional outcomes when the congruity and stability of the hip joint are restored [5, 6]. However, specific fracture patterns and patient factors may increase the risk of subsequent posttraumatic arthritis requiring conversion to THA [8, 26, 27]. It is possible that specific fracture and patient characteristics, evolution in implant materials and bearing surfaces, and surgeon confidence in implant survivorship may have driven the small increases in the use of THA (4.8%) and ORIF + THA (2.6%) in middle-aged adults.
We observed differences in the treatment of acetabular fractures by patient sex among older adults: women over age 65 were more likely to receive a THA for acetabular fracture than men, with the incidence of THA for acetabular fracture increasing 2.5% annual in women and 0.5% per year in men. Disparities in treatment by sex may be related to sex-based differences in underlying risk factors for poor outcome with ORIF – chiefly, perhaps, osteoporosis. Most acetabular fractures in the elderly are associated with osteopenic or osteoporotic bone and consequently demonstrate more complex fracture patterns with impaction, comminution, and higher rates of failure when treated with ORIF [5, 26]. Women are more likely to develop osteoporosis than men with advancing age, but the burden of metabolic bone disease among older men and the implications for the outcomes of acetabular ORIF should not be disregarded [28, 29]. The sex-based differences in treatment we observed may also reflect survivorship bias as more women survive to old age and sustain acetabular fractures than men. We did not observe longitudinal trends in treatment by race.
Medicare primary insurance was also associated with a more rapid adoption of THA and concurrent decline in use of ORIF compared to patients without non-Medicare primary insurance. Medicare reimbursement for hip fracture declined 30% between 2000 and 2020 [30]. Medicare reimbursement of acetabular fracture ORIF under DRG 536 is also equivalent to pelvic fracture closed reduction internal fixation, despite major differences in perioperative resources, risk, blood loss, surgical time, and technical difficulty of open acetabular fracture surgery versus minimally invasive percutaneous pelvic ring screw fixation [31]. Unlike femoral neck and head fractures, THA for acetabular fracture is not eligible for bundled payment programs which may protect reimbursement for this use of THA [32]. Our data also demonstrate longitudinally stable costs of care for patients undergoing THA, while ORIF and ORIF + THA related costs rose significantly over the same period. These differential costs are important considerations and are not fully explained by inflation [33]. The combined economic incentives favoring THA may partially account for the practice change observed in patients with acetabular fracture and Medicare primary insurance.
This study has several limitations. The retrospective review of a hospital discharge database is subject to documentation and classification bias. The risk of misclassification may be potentiated by the change from ICD-9 to ICD-10 coding schemes in 2015. We attempted to address this through the careful exclusion of concomitant injuries which may have confounded our analysis. Furthermore, while the NIS database is a validated method to determine national estimates on procedural trends, it is limited to a 20% sample of the actual annual volume of inpatient care. Our observations reflect weighted national estimates rather than observations [34]. This study did not account for injury mechanism, injury severity, or comorbid conditions, which may also influence treatment. These trends may not be generalizable to practice outside of the United States.
In conclusion, THA is increasingly being used as a primary or adjunctive treatment acetabular fracture in middle aged and older US adults, while the incidence of ORIF has declined. Female sex and Medicare insurance were significantly associated with more rapid adoption of THA as a treatment for acetabular fracture in patients ≥ 65 years old. The downstream implications of these evolving treatment trends unknown and warrant further investigation, particularly with regard to physical function, hip survival, health status, independence, and costs of care.
Data availability
Data analyzed in the present study are available online through the National Inpatient Sample Program at https://hcup-us.ahrq.gov/nisoverview.jsp.
References
Ferguson TA, Patel R, Bhandari M, Matta JM (2010) Fractures of the acetabulum in patients aged 60 years and older: an epidemiological and radiological study. J Bone Joint Surg Br 92-B:250–257. https://doi.org/10.1302/0301-620X.92B2.22488
Daurka JS, Pastides PS, Lewis A, Rickman M, Bircher MD. Acetabular fractures in patients aged > 55 years: a systematic review of the literature. Bone Joint J 96-B:157–63. https://doi.org/10.1302/0301-620X.96B2.32979
Khoshbin A, Atrey A, Chaudhry H, Nowak L, Melo LT, Stavrakis A, et al. Mortality rate of geriatric acetabular fractures is high compared with hip fractures. A matched cohort study. J Orthopaedic Trauma 2020;34:424–428. https://doi.org/10.1097/BOT.0000000000001758
Anglen JO, Burd TA, Hendricks KJ, Harrison P (2003) The, “Gull Sign”: a harbinger of failure for internal fixation of geriatric acetabular fractures. J Orthop Trauma 17:625–634. https://doi.org/10.1097/00005131-200310000-00005
Mears DC (1999) Surgical treatment of acetabular fractures in elderly patients with osteoporotic bone. J Am Acad Orthop Surg 7:128–141. https://doi.org/10.5435/00124635-199903000-00006
Letournel E (1980) Acetabulum fractures: classification and management. Clin Orthop Relat Res, 81–106
Herscovici D, Lindvall E, Bolhofner B, Scaduto JM (2010) The combined hip procedure: open reduction internal fixation combined with total hip arthroplasty for the management of acetabular fractures in the elderly. J Orthop Trauma 24:291–296. https://doi.org/10.1097/BOT.0b013e3181b1d22a
Tannast M, Najibi S, Matta JM (2012) Two to twenty-year survivorship of the hip in 810 patients with operatively treated acetabular fractures. J Bone Joint Surg-Am 94:1559–67. https://doi.org/10.2106/JBJS.K.00444
Matta J (1996) Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Joint Surg Am 78:1632–1645. https://doi.org/10.1055/s-0030-1267077
Weaver MJ, Smith RM, Lhowe DW, Vrahas MS (2018) Does total hip arthroplasty reduce the risk of secondary surgery following the treatment of displaced acetabular fractures in the elderly compared to open reduction internal fixation? A Pilot Study. J Orthop Trauma 32(Suppl 1):S40–S45. https://doi.org/10.1097/BOT.0000000000001088
Boelch SP, Jordan MC, Meffert RH, Jansen H (2017) Comparison of open reduction and internal fixation and primary total hip replacement for osteoporotic acetabular fractures: a retrospective clinical study. Int Orthop 41:1831–1837. https://doi.org/10.1007/s00264-016-3260-x
McCormick BP, Serino J, Orman S, Webb AR, Wang DX, Mohamadi A et al (2022) Treatment modalities and outcomes following acetabular fractures in the elderly: a systematic review. Eur J Orthop Surg Traumatol 32:649–659. https://doi.org/10.1007/s00590-021-03002-3
Borg T, Hernefalk B, Hailer NP (2019) Acute total hip arthroplasty combined with internal fixation for displaced acetabular fractures in the elderly: a short-term comparison with internal fixation alone after a minimum of two years. Bone Joint J 101-B:478–483. https://doi.org/10.1302/0301-620X.101B4.BJJ-2018-1027.R2
MacCormick LM, Lin CA, Westberg JR, Schmidt AH, Templeman DC (2019) Acute total hip arthroplasty versus open reduction internal fixation for posterior wall acetabular fractures in middle-aged patients. OTA Int 2:e014. https://doi.org/10.1097/OI9.0000000000000014
Nicol GM, Sanders EB, Kim PR, Beaulé PE, Gofton WT, Grammatopoulos G (2021) Outcomes of total hip arthroplasty after acetabular open reduction and internal fixation in the elderly—acute vs delayed total hip arthroplasty. J Arthroplasty 36:605–611. https://doi.org/10.1016/j.arth.2020.08.022
Salama W, Mousa S, Khalefa A, Sleem A, Kenawey M, Ravera L et al (2017) Simultaneous open reduction and internal fixation and total hip arthroplasty for the treatment of osteoporotic acetabular fractures. International Orthopaedics (SICOT) 41:181–189. https://doi.org/10.1007/s00264-016-3175-6
Lin C, Caron J, Schmidt AH, Torchia M, Templeman D (2015) Functional outcomes after total hip arthroplasty for the acute management of acetabular fractures: 1- to 14-year follow-up. J Orthop Trauma 29:151–159. https://doi.org/10.1097/BOT.0000000000000164
HCUP Nationwide Inpatient Sample (NIS) (2011) Healthcare cost and utilization project (HCUP)
HCUP National Inpatient Sample (NIS) (2012) Healthcare cost and utilization project (HCUP)
Houchens RL, Ross DN, Elixhauser A, Jiang J (2021) Nationwide Inpatient sample redesign final report. 2014. HCUP NIS Related Reports ONLINE. April 4 2014. US Agency for Healthcare Research and Quality
Tannast M, Najibi S, Matta JM (2012) Two to twenty-year survivorship of the hip in 810 patients with operatively treated acetabular fractures. J Bone Joint Surg Am 94:1559–1567. https://doi.org/10.2106/JBJS.K.00444
Manson TT, Slobogean GP, Nascone JW, Sciadini MF, LeBrun CT, Boulton CL et al (2022) Open reduction and internal fixation alone versus open reduction and internal fixation plus total hip arthroplasty for displaced acetabular fractures in patients older than 60 years: a prospective clinical trial. Injury 53:523–528. https://doi.org/10.1016/j.injury.2021.09.048
Kreder HJ, Rozen N, Borkhoff CM, Laflamme YG, McKee MD, Schemitsch EH, et al (2006) Determinants of functional outcome after simple and complex acetabular fractures involving the posterior wall. J Bone Joint Surg Br 88-B:776–82. https://doi.org/10.1302/0301-620X.88B6.17342
Mears DC, Velyvis JH (2002) Acute total hip arthroplasty for selected displaced acetabular fractures: two to twelve-year results. J Bone Joint Surg Am 84:1–9. https://doi.org/10.2106/00004623-200201000-00001
Kelly M, Peterson DF, Yoo J, Working ZM, Friess D, Kagan R (2023) Risk of revision and complications after total hip arthroplasty for acute treatment of acetabular fracture. J Arthroplasty. https://doi.org/10.1016/j.arth.2023.05.038
Verbeek DO, van der List JP, Tissue CM, Helfet DL (2018) Predictors for long-term hip survivorship following acetabular fracture surgery: importance of gap compared with step displacement. J Bone Joint Surg 100:922–929. https://doi.org/10.2106/JBJS.17.00692
Firoozabadi R, Hamilton B, Toogood P, Routt M “Chip”, Shearer D (2018) Risk factors for conversion to total hip arthroplasty after acetabular fractures involving the posterior wall. J Orthopaedic Trauma 32:607–611. https://doi.org/10.1097/BOT.0000000000001327
Vescini F, Chiodini I, Falchetti A, Palermo A, Salcuni AS, Bonadonna S et al (2021) Management of osteoporosis in men: a narrative review. IJMS 22:13640. https://doi.org/10.3390/ijms222413640
Nelson R, Willson T, Nelson S, Newbold J, LaFleur J (2015) The clinical epidemiology of male osteoporosis: a review of the recent literature. CLEP 65. https://doi.org/10.2147/CLEP.S40966
Haglin JM, Lott A, Kugelman DN, Konda SR, Egol KA (2021) Declining medicare reimbursement in orthopaedic trauma surgery: 2000–2020. J Orthop Trauma 35:79–85. https://doi.org/10.1097/BOT.0000000000001947
Samuel AM, Webb ML, Lukasiewicz AM, Basques BA, Bohl DD, Varthi AG et al (2016) Variation in resource utilization for patients with hip and pelvic fractures despite equal medicare reimbursement. Clin Orthop Relat Res 474:1486–1494. https://doi.org/10.1007/s11999-016-4765-8
Malik AT, Khan SN, Ly TV, Phieffer L, Quatman CE (2020) The “Hip Fracture” bundle—experiences, challenges, and opportunities. Geriatr Orthop Surg Rehabil 11:215145932091084. https://doi.org/10.1177/2151459320910846
U.S Inflation Calculator. US Inflation Calculator 2023. https://www.usinflationcalculator.com/. Accessed 28 Feb 2023
Alluri RK, Leland H, Heckmann N (2016) Surgical research using national databases. Ann Transl Med 4:393–393. https://doi.org/10.21037/atm.2016.10.49
Acknowledgements
Neither generative artificial intelligence nor writing assistance were used in the production of this work. This work has not previously been published or presented.
Funding
Open access funding provided by SCELC, Statewide California Electronic Library Consortium.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
JTP reports research support from AO North America, consulting fees from Johnson & Johnson, and board or committee membership with Orthopaedic Trauma Association. RF reports honoraria from AO North America AO, royalties from Innomed, consulting fees from Smith & Nephew, and board or committee membership with Orthopaedic Trauma Association. The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: JTP reports research support from AO Trauma North America, board or committee membership with Orthopaedic Trauma Association, and consulting fees from Johnson & Johnson. No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article. JW, PK, AA declare no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Ethical approval
This study was performed with de-identified public data and was therefore exempt from institutional review board approval. This study was exempt from Institutional Review Board as data is de-identified. Investigation performed at Keck School of Medicine of University of Southern California. This work was accepted for presentation as a poster at the Orthopaedic Trauma Association Annual meeting in Seattle, WA in October 2023.
Informed consent
This study was performed with de-identified public data and therefore did not require informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
590_2023_3653_MOESM2_ESM.docx
STROBE diagram of cohort selection. Given non-specificity of ICD-9-PCS coding for acetabular fractures, patients with concomitant fractures* (clavicular, patellar, pelvic, proximal femoral, sacral, and scapular) were excluded from analysis. (DOCX 25 kb)
590_2023_3653_MOESM3_ESM.docx
Acetabular treatment trends by open reduction internal fixation (black), total hip arthroplasty (dark grey), and open reduction internal fixation + total hip arthroplasty (light grey) in the NIS database from 2010 to 2020 by admitting hospital type. a. rural hospital admissions in ages ≥65 b. urban non-teaching hospital admissions in ages ≥65 c. urban teaching hospital admissions in ages ≥65 d. rural hospital admissions in ages 45–64 e. urban non-teaching hospital admissions in ages 45–64 f. urban teaching hospital admissions in ages 45–64 (DOCX 29 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Patterson, J.T., Wier, J., Kumaran, P. et al. Rising incidence of acute total hip arthroplasty for primary and adjunctive treatment of acetabular fracture in older and middle-aged adults. Eur J Orthop Surg Traumatol (2023). https://doi.org/10.1007/s00590-023-03653-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00590-023-03653-4










