Abstract
Purpose
The outcomes of anterior cruciate ligament reconstruction (ACLR) in patients with generalized joint laxity (GJL) are not clearly understood. In this study, we compared the outcomes of ACLR with quadruple hamstring autograft between GJL and non-GJL patients.
Methods
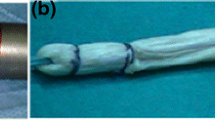
In a retrospective case–control study, 36 patients with GJL, according to the Beighton and Horan Joint Mobility Index, who underwent ACLR surgery, were included. Forty-four group-matched non-GJL patients were included in the control group. The mean follow-up of the patients was 20.65 ± 6.93 months. The outcomes of ACLR were evaluated by the Lachman test, pivot shift test, anterior tibial translation and KT-1000 side-to-side difference, and International Knee Documentation Committee (IKDC) scale.
Results
The results of the Lachman and pivot shift test were not significantly different between the GJL and non-GJL patients (P = 0.67 and P = 0.27, respectively). The mean anterior tibial translation was 7.06 ± 1.41 mm in the GJL group and 6.11 ± 1.53 mm in the non-GJL group (P = 0.006). The mean KT-1000 side-to-side difference was 2.25 ± 1.31 mm in the case and 2.5 ± 1.44 mm in the control group (P = 0.42). The mean IKDC score of the patients was not significantly different between the GJL and non-GJL groups (66.1 ± 20.6 vs. 69.9 ± 16.1, P = 0.35). ACLR failure occurred in 2 (5.5%) patients of the GJL group and no patients of the control group (P = 0.21).
Conclusion
The present findings suggest ACLR with quadruple hamstring autograft as an adequate treatment for GJL patients, at least in short-term follow-up.
Similar content being viewed by others
References
Kim S-J, Kumar P, Kim S-H (2010) Anterior cruciate ligament reconstruction in patients with generalized joint laxity. Clin Orthop Surg 2(3):130–139. https://doi.org/10.4055/cios.2010.2.3.130
Nicholas JA (1970) Injuries to knee ligaments. Relationship to looseness and tightness in football players. Jama 212(13):2236–9. https://doi.org/10.1001/jama.212.13.2236
Acasuso Díaz M, Collantes Estévez E, Sánchez Guijo P (1993) Joint hyperlaxity and musculoligamentous lesions: study of a population of homogeneous age, sex and physical exertion. Br J Rheumatol 32(2):120–122. https://doi.org/10.1093/rheumatology/32.2.120
Ramesh R, Von Arx O, Azzopardi T, Schranz PJ (2005) The risk of anterior cruciate ligament rupture with generalised joint laxity. J Bone Joint Surg Br 87(6):800–803. https://doi.org/10.1302/0301-620x.87b6.15833
Myer GD, Ford KR, Paterno MV, Nick TG, Hewett TE (2008) The effects of generalized joint laxity on risk of anterior cruciate ligament injury in young female athletes. Am J Sports Med 36(6):1073–1080. https://doi.org/10.1177/0363546507313572
Kramer LC, Denegar CR, Buckley WE, Hertel J (2007) Factors associated with anterior cruciate ligament injury: history in female athletes. J Sports Med Phys Fit 47(4):446–454
Jackson DW, Simon TM (2002) Donor cell survival and repopulation after intraarticular transplantation of tendon and ligament allografts. Microsc Res Tech 58(1):25–33. https://doi.org/10.1002/jemt.10118
Kim SJ, Lee SK, Choi CH, Kim SH, Kim SH, Jung M (2014) Graft selection in anterior cruciate ligament reconstruction for smoking patients. Am J Sports Med 42(1):166–172. https://doi.org/10.1177/0363546513505191
Hardin JA, Voight ML, Blackburn TA, Canner GC, Soffer SR (1997) The effects of “decelerated” rehabilitation following anterior cruciate ligament reconstruction on a hyperelastic female adolescent: a case study. J Orthop Sports Phys Ther 26(1):29–34. https://doi.org/10.2519/jospt.1997.26.1.29
Kim SJ, Kim TE, Lee DH, Oh KS (2008) Anterior cruciate ligament reconstruction in patients who have excessive joint laxity. J Bone Joint Surg Am 90(4):735–741. https://doi.org/10.2106/jbjs.f.01173
Sundemo D, Hamrin Senorski E, Karlsson L, Horvath A, Juul-Kristensen B, Karlsson J et al (2019) Generalised joint hypermobility increases ACL injury risk and is associated with inferior outcome after ACL reconstruction: a systematic review. B MJ Open Sport Exerc Med 5(1):e000620. https://doi.org/10.1136/bmjsem-2019-000620
Beighton P, Solomon L, Soskolne CL (1973) Articular mobility in an African population. Ann Rheum Dis 32(5):413–418. https://doi.org/10.1136/ard.32.5.413
Strauss MJ, Varatojo R, Boutefnouchet T, Condello V, Samuelsson K, Gelber PE et al (2019) The use of allograft tissue in posterior cruciate, collateral and multi-ligament knee reconstruction. Knee Surg Sports Traumatol Arthrosc 27(6):1791–1809. https://doi.org/10.1007/s00167-019-05426-1
Outerbridge RE, Dunlop JA (1975) The problem of chondromalacia patellae. Clin Orthop Relat res 110:177–196
Kim S-J, Choi CH, Lee S-K, Lee W, An H, Jung M (2018) Minimum two-year follow-up of anterior cruciate ligament reconstruction in patients with generalized joint laxity. J Bone Joint Surg Am 100(4):278–287
Kilinc BE, Kara A, Celik H, Oc Y, Camur S (2016) Evaluation of the accuracy of Lachman and anterior drawer tests with KT1000 in the follow-up of anterior cruciate ligament surgery. J Exerc Rehabil 12(4):363–367. https://doi.org/10.12965//jer.1632622.311
Samitier G, Marcano AI, Alentorn-Geli E, Cugat R, Farmer KW, Moser MW (2015) Failure of anterior cruciate ligament reconstruction. Arch Bone Joint Surg 3(4):220–240
Ebrahimzadeh MH, Makhmalbaf H, Golhasani-Keshtan F, Rabani S, Birjandinejad A (2015) The international knee documentation committee (IKDC) subjective short form: a validity and reliability study. Knee Surg Sports Traumatol Arthrosc 23(11):3163–3167. https://doi.org/10.1007/s00167-014-3107-1
Irrgang JJ, Anderson AF, Boland AL, Harner CD, Kurosaka M, Neyret P et al (2001) Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med 29(5):600–613. https://doi.org/10.1177/03635465010290051301
Kim SJ, Moon HK, Kim SG, Chun YM, Oh KS (2010) Does severity or specific joint laxity influence clinical outcomes of anterior cruciate ligament reconstruction? Clin Orthop Relat Res 468(4):1136–1141. https://doi.org/10.1007/s11999-009-0961-0
Kim SJ, Choi CH, Kim SH, Lee SK, Lee W, Kim T et al (2018) Bone-patellar tendon-bone autograft could be recommended as a superior graft to hamstring autograft for ACL reconstruction in patients with generalized joint laxity: 2- and 5-year follow-up study. Knee Surg Sport Traumatol Arthrosc 26(9):2568–2579. https://doi.org/10.1007/s00167-018-4881-y
Larson CM, Bedi A, Dietrich ME, Swaringen JC, Wulf CA, Rowley DM et al (2017) Generalized hypermobility, knee hyperextension, and outcomes after anterior cruciate ligament reconstruction: prospective, case-control study with mean 6 years follow-up. Arthroscopy 33(10):1852–1858. https://doi.org/10.1016/j.arthro.2017.04.012
Liu Z, Jiang J, Yi Q, Teng Y, Liu X, He J et al (2022) An increased posterior tibial slope is associated with a higher risk of graft failure following ACL reconstruction: a systematic review. Knee Surg Sports Traumatol Arthrosc 30(7):2377–2387. https://doi.org/10.1007/s00167-022-06888-6
Rosso F, Bonasia DE, Cottino U, Cambursano S, Dettoni F, Rossi R (2018) Factors affecting subjective and objective outcomes and return to play in anterior cruciate ligament reconstruction: a retrospective cohort study. Joints 6(1):23–32. https://doi.org/10.1055/s-0038-1636931
Gupta R, Singhal A, Malhotra A, Soni A, Masih GD, Raghav M (2020) Predictors for anterior cruciate ligament (ACL) re-injury after successful primary ACL reconstruction (ACLR). Malays Orthop J 14(3):50–56. https://doi.org/10.5704/moj.2011.009
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Nima Hosseinzadeh, Mehdi Mohammadpour, Mehdi Moghtadaei, Hossein Farahini, Ahmad Khazanchin, Shirin Nasiri, and Amir Khazanchin declare that they have no conflict of interest.
Ethical approval
This study was approved by the review board of our institute under the code IR.IUMS.REC 1395.9311242006. Patients provided written consent before participation in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hosseinzadeh, N., Mohammadpour, M., Moghtadaei, M. et al. Evaluation of the short-term outcomes of anatomic ACL reconstruction with hamstring autograft in patients with generalized joint laxity: A retrospective case–control study. Eur J Orthop Surg Traumatol 33, 2049–2055 (2023). https://doi.org/10.1007/s00590-022-03390-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-022-03390-0