Abstract
Purpose
Post-operative complications following fixation of pelvic fractures can lead to mortality and increased morbidity. Available literature regarding complications is heterogeneous and knowledge on risk factors is limited. This study aims to identify the most common post-operative complications and their possible risk factors following pelvic fracture surgery.
Methods
A retrospective cohort study was performed in two level-1 trauma centers in the Netherlands between January 2015 and January 2021. Included patients were all adult patients (≥ 18 years) with an operatively treated pelvic fracture (pelvic ring and/or acetabular fractures). Post-operative complications included surgical site infections (SSI), material-related complications, neurological complications, malunion/non-union and performed reoperations. A forward stepwise multivariable logistic regression analysis was used to identify any risk factors associated with these complications.
Results
Complications occurred in 55 (24%) of the 233 included patients. SSI’s were most common, occurring in 34 (15%) patients. Duration of surgery (odds ratio 1.01 per minute, 95% confidence interval 1.00–1.01) and obesity (odds ratio 1.10 per BMI point, 95% confidence interval 1.29–7.52) were independent risk factors for development of SSI. Less common post-operative complications were material-related complications (8%) and neurological damage (5%).
Conclusion
Limiting operation time by using less invasive and less time-consuming surgical approaches may reduce the risk of SSI. More awareness and post-operative screening for early signs of SSI is mandatory, especially in obese patients. Future research should include large prospective patient cohorts to determine risk factors for other post-operative complications associated with pelvic fracture surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pelvic fractures, including both pelvic ring and acetabular fractures, are often caused by high-energy trauma such as traffic accidents. They occur in up to 25% of severely injured patients [6, 22]. Pelvic fractures can have a profound impact on the patient’s long-term quality of life; many of them do not fully regain their initial level of physical functioning, and experience mental health problems [5] Often surgical fixation of the pelvic ring and/or acetabulum is required to restore stability and improve patient outcomes [23]. Although many surgical techniques and approaches for fixation of pelvic ring and acetabular fractures are described in the literature, open reduction and internal fixation (ORIF) is still the gold standard, since it provides the best possibilities for adequate fracture reduction and fixation, as well as the best long-term results [9, 10].
Pelvic fracture surgery is associated with complication rates up to 35% [12, 16]. These complications include post-operative infections, neurological complications, re-operations, and mortality [3, 4]. Knowledge of post-operative complication rates and risk factors associated with pelvic fracture fixation is needed for developing prevention strategies and improving patient outcomes [11]. Although understanding the risk factors for surgical complications is important, the available literature regarding complications after pelvic fracture surgery is heterogeneous and mostly addresses only specific subgroups of patients, fracture types or surgical techniques [11, 20].
The current study includes a cohort of patients with pelvic ring, acetabular or combined fractures, that were operated on via commonly used surgical approaches. The aim of this study was to investigate the incidence of common surgical complications and identify their potential risk factors.
Methods and materials
A retrospective cohort study was performed in two level-1 trauma centers in the Netherlands: the Leiden University Medical Center (LUMC) in Leiden and the Haaglanden Medical Center (HMC) in The Hague. The study protocol was approved by the regional Medical Ethics Review Board (protocol nr. G20.118).
Patients
All adult patients (≥ 18 years old) with a surgically treated pelvic ring and/or acetabular fracture in the period from January 2015 up to January 2021 were selected from the regional trauma registry and included for analysis. Patients with previous pelvic ring or acetabular fractures and patients with pathological fractures were excluded.
All patients received standard of care according to the current hospital’s operative and post-operative treatment guidelines regarding traumatic pelvic fractures. According to these guidelines, all patients received standard antibiotic prophylaxis of 1 or 2 g of cefazolin. All operations were conducted by a senior trauma surgeon trained and experienced in pelvic fracture surgery, assisted either by another trauma surgeon or a surgical resident in training.
Data collection
All data were collected from electronic patient records of participating centers. Data concerned the number and type of complications including surgical site infections (SSI). SSI were defined if they were indicated as such in the patient records or if there were local signs of infection at the incision site (e.g., redness, wound fluid leakage) either combined with systemic signs of infection (e.g., fever, leukocytosis). Material-related complications were defined as break-out of material and mechanical irritation followed by material removal. Nerve damage was defined as persistent nerve damage after 6 months since surgery. Other study parameters included mal- and non-union, reoperation, baseline characteristics including demographic data, obesity defined as body mass index ≥ 30, ASA Physical Status Classification, smoking, osteoporosis, use of anticoagulants, fracture and other injury characteristics including high or low energy trauma, applied treatment, surgical intervention (Kocher- Langenbeck approach, (Modified) Stoppa approach, ilioinguinal approach, percutaneous fixation and external fixation), operation time (time between incision and wound closure), materials used, use of pre- and post-operative antibiotics, and hospital outcomes including duration of hospital stay, ICU admission and in-hospital mortality. Data were stored in a secured and coded database in the Castor Electronic Data Capture (EDC) System.
Pelvic ring fractures were classified according to the Young-Burgess classification and acetabular fractures according to the Letournel classification [1, 18].
Statistical analysis
Data are presented for the total group and per fracture type. Categorical data are presented as number and percentage, and continuous variables were presented as mean with standard deviation (SD) or as median with interquartile range (IQR) if not normally distributed according to the Shapiro–Wilk test. Differences in the mean operation time between surgical approaches were tested using ANOVA. Forward stepwise multivariable logistic regression analysis (p-to-enter = 0.05) was used to identify risk factors for the most prevalent post-operative complication (SSI). All analyses were performed using IBM’s statistical package for social sciences (SPSS) version 27.
Results
Baseline characteristics and hospital outcomes
The study population consisted of 233 patients. Baseline characteristics are presented in Table 1. The median age was 59 years (IQR 38–72), and 62% of patients were male. Seventy-seven percent of the patients had sustained high-energy trauma. Twenty-nine percent of the patients were admitted to the ICU. Six patients died during hospital admission (3% of patients). Five patients died due to other injuries than the pelvic fracture. One patient died one week after the initial operation due to a bowel perforation and one patient died because of an in-hospital cardiac arrest (Table 1).
Pelvic ring fractures
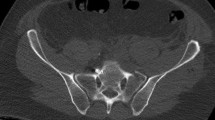
Pelvic ring fractures were diagnosed in 127 (55%) patients. Most common were Lateral Compression (LC) type 1 fractures (n = 37; 29%), LC type 2 fractures (n = 22; 17%) and isolated sacrum fractures (n = 19; 15%). (Table 2) A percutaneous surgical approach was used in 39 patients (31%) and the (Modified) Stoppa approach in 35 patients (28%). Twenty-eight patients were treated using external fixation, of whom 22 received internal fixation and 6 external fixation as definite treatment.
Acetabular fractures
In total, 101 (43%) patients suffered from an acetabular fracture. Both column type was seen in 29 patients (29%) and anterior posterior hemi-transverse fracture in 27 patients (27%). (Table 2) The (Modified) Stoppa approach was used in 51% of patients (n = 51) and the Kocher-Langenbeck was used in 23% of patients (n = 23). Five patients received a total hip prosthesis as a primary treatment without previous fixation (5%). Secondary hip protheses were placed in 8 (8%) patients.
Combined fractures
Five patients (2% of the cohort) with median age of 35 years (31–50) sustained combined pelvic ring and acetabular fractures. All of these patients sustained a high energy trauma. The modified Stoppa approach was used in 2 patients (40%), two patients were treated with a (modified) Stoppa combined with an ilioinguinal approach, medial lumbosacral incision or a prolonged abdominal incision. (Table 2).
Duration of surgery
The mean duration of surgery differed significantly between the surgical approaches (p < 0.01). The shortest operation time was recorded for patients undergoing surgical fixation via the percutaneous approach (mean 57 min; 28 SD). The longest duration of surgery was recorded for the group in which a combination of the modified Stoppa and Kocher-Langenbeck approach was used (mean 277 min, SD 50) (Table 3).
Post-operative complications
Seventy post-operative complications occurred in 50 (21%) patients (Table 4). SSI was observed in 34 patients of which 29 subsequently needed some sort of re-operation (mainly operative debridement because of SSI). Osteomyelitis in addition to a deep infection was diagnosed twice. (Table 4) Overall, Staphylococcus Aureus was found in six percent of patients with an infection, and another 6% had an isolated staphylococcus epidermidis in their wound culture. In 5% an Enterococcus faecium and in 5% Streptococcus anginosus was found in the wound cultures. Ten percent of the patients witch an infection was treated with Flucloxacillin, and 7% was treated with Vancomycin. Material-related complications occurred in 14 patients. Irritation due to fixation material subsequently led to osteosynthesis removal in 8 cases and plate breakage in 6 cases. Impaired fracture healing, including non-union and malunion, was diagnosed in 8 patients and eventually led to revision surgery in 6 cases. Persistent neurological complications occurred in 10 patients (Table 4).
Risk factors for surgical site infections (SSI)
Univariable analysis showed that patients with SSI were significantly younger (mean 56 years vs. 50 years; p = 0.09; Table 5), more often suffered from obesity (35% vs 12%; p = 0.001), had a significantly longer duration of surgery (179 min vs 138 min; p = 0.003) and hospital stay (28 days vs 17 days; p = 0.08). The use of external fixator before definitive surgery, the amount of ICU admission, smoking and high or low-energy trauma did not differ significantly between the patients with or without SSIs. (Table 5) In the multivariable logistic regression analysis using forward selection, presence of obesity (OR: 3.12; 95% CI: 1.29–7.52; p = 0.01) and duration of surgery (OR per minute increase: 1.01; 95% CI: 1.00–1.01; p = 0.04) were identified as independent risk factors for the development of SSI (Table 5).
Discussion
This cohort study found an overall complication rate following operative treatment of pelvic ring and acetabular fractures of 21% and in-hospital mortality of 3%. The most common post-operative complication was SSI (accounting for 49% of all reported complications) followed by material-related (20%) and neurological complications (14%). Multivariable analysis identified duration of surgery and obesity as independent risk factors for SSI’s.
Surgical site infections (SSI)
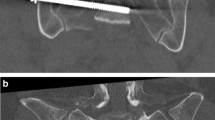
In the current study, patients’ age, obesity, duration of surgery and hospital stay were significantly associated with SSI in the univariable analysis (Table 5). In the multivariable analysis, obesity (OR 3.12; p = 0.01) and duration of surgery (OR: 1.006; p = 0.04) remained independent, statistically significant predictors for the development of SSI after pelvic fracture surgery. (Table 3) In pelvic fracture surgery, ORIF is still the gold standard since it provides excellent fracture exposure. The downside of open surgery, however, is the prolonged operation time and large surgical wound areas which increase the risk of SSI as shown by our study and other literature [8]. Based on these findings avoiding prolonged operation times seems of key importance to reduce the risk of SSI. In the current study, the shortest operation time (57 min; 28 SD) was recorded in patients treated via the percutaneous approach. This approach is not only associated with shorter operation times but because of their minimally invasive nature also involve smaller surgical wound areas. However, for complex multi-fragment displaced pelvic ring or acetabular fractures, a percutaneous approach is not possible because of technical reasons including unsatisfactory fracture exposure leading to inadequate fracture reposition or fixation. Still further development of novel minimally invasive and efficient operation techniques is key for reducing operation time and wound exposure which would reduce the risk of post-operative infections [2].
Another significant risk factor identified in the current study was obesity. Several underlying causes such as lower tissue levels of prophylactic antibiotic and also prolonged operation times are hypothesized to lead to the increased risk of SSI in obese patients [7, 13, 21]. Extra pre- and post-operative attention, adequate pre-operative counseling about the increased risk of SSI should be considered in these patients. Furthermore, extra attention and awareness of early signs of SSI is recommended to prevent or, if present, to detect SSI in a early stage. Early detection followed by adequate treatment leads to less severe outcomes and could prevent the necessity of operative debridement [25, 26]. However, in the current study, almost all patients with SSI needed revision surgery which can lead to a significantly longer hospital stay, adverse outcomes or higher healthcare costs.
Neurological complications
Persistent neurological complications (13% of all complications) were relatively uncommon which is in accordance with existing literature [15]. Neurological complications can either be caused by the accident itself or be induced by the intervention. In acetabular fractures involvement of the posterior wall and the Kocher-Langenbeck approach are more commonly associated with nerve damage since especially the sciatic nerve is at risk [17]. This is also the case for posterior fixation of pelvic ring fractures [15]. However, when anterior pelvic ring fractures are fixated using for example the (modified) Stoppa approach, the neurovascular bundles of the bladder are particularly at risk [15]. Also, iatrogenic injury of the obturator and sciatic nerve has been described when using this approach [15].
Material-related complications
Although less common, material-related complications after acetabular and pelvic ring surgery are reported and associated with severe adverse outcomes including chronic residual pain, material removal, deformity, and progressive physical impairment [19, 24]. Material-related complications including plate breakage and mechanical irritation accounted for 13% of all complications observed in the current study. Literature reporting on material-related complications after acetabular or pelvic ring treatment reports complication rates between 0 and 22% but is heterogeneous with respect to definition and included patients [3, 15].
Impaired fracture healing
Although malunion and non-union of surgically treated acetabular and pelvic ring fractures are rare, treating these conditions can be very challenging [14]. Since mal and non-union are not common, literature regarding this matter is scarce and exact incidence rates are not clearly defined. This is partly due to the differences in the definition of mal and non-union between studies [14]. In the current study, impaired fracture healing diagnosed on radiographs occurred in 3% of the patients. Several underlying causes such as low-grade infections, osteoporosis or other conditions involving bone demineralization are associated with the development of non- and malunions. However, most cases of mal-union or non-union after pelvic fracture surgery are caused by delayed or inadequate fixation [27]. Frequent follow-up using physical examination and radiographic evaluation is necessary to detect this complication and to treat it accordingly.
Study limitations
The main limitations of the study are related to the retrospective design of the study and its small sample size. Therefore, the statistical power was limited, and only two independent risk factors for the most common complication (SSI) could be identified in the multivariable analysis. Due to the retrospective study design and without data on follow-up after hospital discharge, it was not possible to assess the effects of complications on long-term functional outcomes.
Conclusion
The most common post-operative complications after surgery of pelvic ring or acetabular fractures are SSI’s, which account for almost half of the reported complications. Independent risk factors for SSI’s were increased duration of surgery and obesity. These findings stress the need to avoid prolonged operation times and encourage the use of minimally invasive surgical approaches. Furthermore, extra post-operative awareness of early signs of SSI is recommended to prevent adverse outcomes and re-operations, especially in obese patients since these patients are highly susceptible for developing SSI’s. More prospective research is needed with larger patient cohorts including all subgroups of patients, fracture types and surgical techniques to further determine risk factors for post-operative complications associated with pelvic fracture surgery.
Change history
08 October 2022
Table 1: in the most right column the title says: ‘fracturesn = 5’ . It should be ‘fractures n = 5’ and the ‘n’ should be in italic and in Table 2: after the variable ‘Fixation material’ the ‘;’ is missing and it has been updated and in Table 5: after the variable ‘external fixator before definitive surgery’ the ‘n’ should be in italic. The same for the ‘n’ following surgical approach.
References
Alton TB, Gee AO (2014) Classifications in brief: young and burgess classification of pelvic ring injuries. Clin Orthop Relat Res 472(8):2338–2342. https://doi.org/10.1007/s11999-014-3693-8
Andersen BM (2018) Prevention of postoperative wound infections. Prevent Cont Infect Hospitals. https://doi.org/10.1007/978-3-319-99921-0_33
Bakhshayesh P, Weidenhielm L, Enocson A (2018) Factors affecting mortality and reoperations in high-energy pelvic fractures. Eur J Orthop Surg Traumatol. 28(7):1273–1282. https://doi.org/10.1007/s00590-018-2203-1
Bellabarba C, Schildhauer TA, Vaccaro AR, Chapman JR (2006) Complications associated with surgical stabilization of high-grade sacral fracture dislocations with spino-pelvic instability. Spine (Phila Pa 1976) 31(Suppl):S80–S88. https://doi.org/10.1097/01.brs.0000217949.31762.be
Brouwers L, de Jongh MAC, de Munter L, Edwards M, Lansink KWW (2020) Prognostic factors and quality of life after pelvic fractures. The brabant injury outcome surveillance (BIOS) study. PLoS One 15(6):e0233690. https://doi.org/10.1371/journal.pone.0233690
Buller LT, Best MJ, Quinnan SM (2016) A nationwide analysis of pelvic ring fractures: incidence and trends in treatment, length of stay, and mortality. Geriatr Orthop Surg Rehabil 7(1):9–17. https://doi.org/10.1177/2151458515616250
Carson JT, Shah SG, Ortega G, Thamyongkit S, Hasenboehler EA, Shafiq B (2018) Complications of pelvic and acetabular fractures in 1331 morbidly obese patients (BMI ≥ 40): a retrospective observational study from the National Trauma Data Bank. Patient Saf Surg. https://doi.org/10.1186/s13037-018-0172-2
Chen L, Zhang G, Song D, Guo X, Yuan W (2012) A comparison of percutaneous reduction and screw fixation versus open reduction and plate fixation of traumatic symphysis pubis diastasis. Arch Orthop Trauma Surg 132(2):265–270. https://doi.org/10.1007/s00402-011-1414-2
Halawi MJ (2016) Pelvic ring injuries: surgical management and long-term outcomes. J Clin Orthop Trauma 7(1):1–6. https://doi.org/10.1016/j.jcot.2015.08.001
Hartensuer R, Lodde MF, Keller J, Eveslage M, Stolberg-Stolberg J, Riesenbeck O et al (2020) Safety, effect and feasibility of percutaneous SI-Screw with and without augmentation-A 15-Year retrospective analysis on over 640 Screws. J Clin Med 9(8):2660. https://doi.org/10.3390/jcm9082660
Henstenburg JM, Larwa JA, Williams CS, Shah MP, Harding SP (2021) Risk factors for complications following pelvic ring and acetabular fractures: a retrospective analysis at an urban level 1 trauma center. J Orthopaed Trauma Rehabilit 28:22104917211006890. https://doi.org/10.1177/22104917211006890
Jindal K, Aggarwal S, Kumar P, Kumar V (2019) Complications in patients of acetabular fractures and the factors affecting the quality of reduction in surgically treated cases. J Clin Orthop Trauma 10(5):884–889. https://doi.org/10.1016/j.jcot.2019.02.012
José Alonso S-V, Smedts C (2020) Obesity a risk factor for infection after surgery. Intechopen, London. https://doi.org/10.5772/intechopen.91216
Kanakaris NK, Angoules AG, Nikolaou VS, Kontakis G, Giannoudis PV (2009) Treatment and outcomes of pelvic malunions and nonunions: a systematic review. Clin Orthop Relat Res 467(8):2112–2124. https://doi.org/10.1007/s11999-009-0712-2
Küper MA, Trulson A, Minarski C, Stuby F, Stöckle U, Konrads C (2021) Risks and strategies to avoid approach-related complications during operative treatment of pelvic ring or acetabular fractures. Z Orthop Unfall 159(2):144–152. https://doi.org/10.1055/a-1023-4756
Lal SR (2018) Outcome of surgical treatment for displaced acetabular fractures: a prospective study. Rev Bras Ortop 53(4):482–488. https://doi.org/10.1016/j.rboe.2017.12.007
Lehmann W, Hoffmann M, Fensky F, Nüchtern J, Großterlinden L, Aghayev E et al (2014) What is the frequency of nerve injuries associated with acetabular fractures? Clin Orthop Relat Res 472(11):3395–403. https://doi.org/10.1007/s11999-014-3838-9
Letournel E (1980) Acetabulum fractures: classification and management. Clin Orthop Relat Res 151:81–106
Marchand LS, Working ZM, Rane AA, Elliott IS, Howenstein A, Haller JM et al (2019) Unstable pelvic ring injuries: how soon can patients safely bear weight? J Orthop Trauma 33(2):71–77. https://doi.org/10.1097/bot.0000000000001356
Mardanpour K, Rahbar M, Mardanpour S, Rezaei M (2020) Risk factors for surgical site infections after open reduction and internal fixation of acetabulum fracture in the west of Iran. Int J Surg Open 27:119–122. https://doi.org/10.1016/j.ijso.2020.11.006
Meijs AP, Koek MBG, Vos MC, Geerlings SE, Vogely HC, de Greeff SC (2019) The effect of body mass index on the risk of surgical site infection. Infect Control Hosp Epidemiol 40(9):991–996. https://doi.org/10.1017/ice.2019.165
Pereira GJC, Damasceno ER, Dinhane DI, Bueno FM, Leite JBR, Ancheschi BdC (2017) Epidemiology of pelvic ring fractures and injuries. Rev Bras Ortop 52(3):260–269. https://doi.org/10.1016/j.rboe.2017.05.012
Pohlemann T, Gänsslen A, Schellwald O, Culemann U, Tscherne H (1996) Outcome after pelvic ring injuries. Injury 27(Suppl 2):B31–B38
Rommens PM, Graafen M, Arand C, Mehling I, Hofmann A, Wagner D (2020) Minimal-invasive stabilization of anterior pelvic ring fractures with retrograde transpubic screws. Injury 51(2):340–346. https://doi.org/10.1016/j.injury.2019.12.018
Smedts JAS-VAC (2020) Obesity: a risk factor for infection after surgery. Intechopen, London. https://doi.org/10.5772/intechopen.91216
Thelwall S, Harrington P, Sheridan E, Lamagni T (2015) Impact of obesity on the risk of wound infection following surgery: results from a nationwide prospective multicentre cohort study in England. Clin Microbiol Infect 21(11):1008.e1–8. https://doi.org/10.1016/j.cmi.2015.07.003
Tripathy SK, Goyal T, Sen RK (2015) Nonunions and malunions of the pelvis. Eur J Trauma Emerg Surg 41(4):335–342. https://doi.org/10.1007/s00068-014-0461-0
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare that are relevant to the content of this article.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Not applicable, according to the approval by the regional Medical Ethics Review Board (protocol nr. G20.118).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mostert, C.Q.B., Timmer, R.A., Krijnen, P. et al. Rates and risk factors of complications associated with operative treatment of pelvic fractures. Eur J Orthop Surg Traumatol 33, 1973–1980 (2023). https://doi.org/10.1007/s00590-022-03375-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-022-03375-z