Abstract
Background
Acetabular fractures and surgical interventions used to treat them can result in nerve injuries. To date, only small case studies have tried to explore the frequency of nerve injuries and their association with patient and treatment characteristics. High-quality data on the risk of traumatic and iatrogenic nerve lesions and their epidemiology in relation to different fracture types and surgical approaches are lacking.
Questions/purposes
The purpose of this study was to determine (1) the proportion of patients who develop nerve injuries after acetabular fracture; (2) which fracture type(s) are associated with increased nerve injury risk; and (3) which surgical approach was associated with the highest proportion of patients developing nerve injuries using data from the German Pelvic Trauma Registry. Two secondary aims were (4) to assess hospital volume–nerve-injury relationship; and (5) internal data validity.
Methods
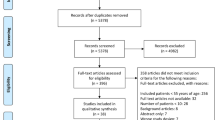
Between March 2001 and June 2012, 2236 patients with acetabular fractures were entered into a prospectively maintained registry from 29 hospitals; of those, 2073 (92.7%) had complete records on the endpoints of interest in this retrospective study and were analyzed. The neurological status in these patients was captured at their admission and at the discharge. A total of 1395 of 2073 (67%) patients underwent surgery, and the proportions of intervention-related and other hospital-acquired nerve injuries were obtained. Overall proportions of patients developing nerve injuries, risk based on fracture type, and risk of surgical approach type were analyzed.
Results
The proportion of patients being diagnosed with nerve injuries at hospital admission was 4% (76 of 2073) and at discharge 7% (134 or 2073). Patients with fractures of the “posterior wall” (relative risk [RR], 2.0; 95% confidence interval [CI], 1.4–2.8; p = 0.001), “posterior column and posterior wall” (RR, 2.9; CI, 1.6–5.0; p = 0.002), and “transverse + posterior wall” fracture (RR, 2.1; CI, 1.3–3.5; p = 0.010) were more likely to have nerve injuries at hospital discharge. The proportion of patients with intervention-related nerve injuries and that of patients with other hospital-acquired nerve injuries was 2% (24 of 1395 and 46 of 2073, respectively). They both were associated with the Kocher-Langenbeck approach (RR, 3.0; CI, 1.4–6.2; p = 0.006; and RR, 2.4; CI, 1.4–4.3; p = 0.004, respectively).
Conclusions
Acetabular fractures with the involvement of posterior wall were most commonly accompanied with nerve injuries. The data suggest also that Kocher-Langenbeck approach to the pelvic ring is associated with a higher risk of perioperative nerve injuries. Trauma surgeons should be aware of common nerve injuries, particularly in posterior wall fractures. The results of the study should help provide patients with more exact information on the risk of perioperative nerve injuries in acetabular fractures.
Level of Evidence
Level III, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.

Similar content being viewed by others
References
AO/OTA. Pelvis. J Orthop Trauma. 2007;21(Suppl 10):S59–S67.
Archdeacon MT, Kazemi N, Guy P, Sagi HC. The modified Stoppa approach for acetabular fracture. J Am Acad Orthop Surg. 2011;19:170–175.
Bradshaw C, McCrory P, Bell S, Brukner P. Obturator nerve entrapment. A cause of groin pain in athletes. Am J Sports Med. 1997;25:402–408.
Cole JD, Bolhofner BR. Acetabular fracture fixation via a modified Stoppa limited intrapelvic approach. Description of operative technique and preliminary treatment results. Clin Orthop Relat Res. 1994;305:112–123.
de Ridder VA, de Lange S, Kingma L, Hogervorst M. Results of 75 consecutive patients with an acetabular fracture. Clin Orthop Relat Res. 1994;305:53–57.
Dunbar RP Jr, Gardner MJ, Cunningham B, Routt ML Jr. Sciatic nerve entrapment in associated both-column acetabular fractures: a report of 2 cases and review of the literature. J Orthop Trauma. 2009;23:80–83.
Fassler PR, Swiontkowski MF, Kilroy AW, Routt ML Jr. Injury of the sciatic nerve associated with acetabular fracture. J Bone Joint Surg Am. 1993;75:1157–1166.
Gruson KI, Moed BR. Injury of the femoral nerve associated with acetabular fracture. J Bone Joint Surg Am. 2003;85:428–431.
Haidukewych GJ, Scaduto J, Herscovici D Jr, Sanders RW, DiPasquale T. Iatrogenic nerve injury in acetabular fracture surgery: a comparison of monitored and unmonitored procedures. J Orthop Trauma. 2002;16:297–301.
Hospodar PP, Ashman ES, Traub JA. Anatomic study of the lateral femoral cutaneous nerve with respect to the ilioinguinal surgical dissection. J Orthop Trauma. 1999;13:17–19.
Issack PS, Helfet DL. Sciatic nerve injury associated with acetabular fractures. HSS J. 2009;5:12–18.
Keel MJ, Bastian JD, Buchler L, Siebenrock KA. [Anterior approaches to the acetabulum] [in German]. Der Unfallchirurg. 2013;116:213–220.
Keel MJ, Ecker TM, Cullmann JL, Bergmann M, Bonel HM, Buchler L, Siebenrock KA, Bastian JD. The Pararectus approach for anterior intrapelvic management of acetabular fractures: an anatomical study and clinical evaluation. J Bone Joint Surg Br. 2012;94:405–411.
Kloen P, Siebenrock KA, Ganz R. Modification of the ilioinguinal approach. J Orthop Trauma. 2002;16:586–593.
Letournel E. Acetabulum fractures: classification and management. Clin Orthop Relat Res. 1980;151:81–106.
Matta JM. Operative treatment of acetabular fractures through the ilioinguinal approach: a 10-year perspective. J Orthop Trauma. 2006;20:S20–29.
Middlebrooks ES, Sims SH, Kellam JF, Bosse MJ. Incidence of sciatic nerve injury in operatively treated acetabular fractures without somatosensory evoked potential monitoring. J Orthop Trauma. 1997;11:327–329.
Ochs BG, Marintschev I, Hoyer H, Rolauffs B, Culemann U, Pohlemann T, Stuby FM. Changes in the treatment of acetabular fractures over 15 years: analysis of 1266 cases treated by the German Pelvic Multicentre Study Group (DAO/DGU). Injury. 2010;41:839–851.
Pohlemann T, Tosounidis G, Bircher M, Giannoudis P, Culemann U. The German Multicentre Pelvis Registry: a template for an European Expert Network? Injury. 2007;38:416–423.
Sagi HC, Afsari A, Dziadosz D. The anterior intra-pelvic (modified Rives-Stoppa) approach for fixation of acetabular fractures. J Orthop Trauma. 2010;24:263–270.
Vrahas M, Gordon RG, Mears DC, Krieger D, Sclabassi RJ. Intraoperative somatosensory evoked potential monitoring of pelvic and acetabular fractures. J Orthop Trauma. 1992;6:50–58.
Yang KH, Han DY, Park HW, Park SJ. Intraarticular entrapment of the obturator nerve in acetabular fracture. J Orthop Trauma. 2001;15:361–363.
Acknowledgments
We thank all members of the Pelvic Trauma Working Group of the German Trauma Association. Without their efforts, the German Pelvic Trauma Registry and this study would not have been possible. Institutions contributing to the German Pelvic Trauma Registry include: AZ Groeninge Hospital, Kortrijk, Belgium; BG Trauma Hospital, Halle, Germany; BG Trauma Hospital, Tübingen, Germany; BG Trauma Hospital, Ludwigshafen, Germany; BG Trauma Hospital, Murnau, Germany; German Army Hospital, Ulm, Germany; Charité Virchow Campus, Berlin, Germany; Friederikenstift Hospital, Hannover, Germany; University Hospital, Regensburg, Germany; General Hospital, Ludwigsburg, Germany; Hospital of the Technical University, Munich, Germany; General Hospital, Augsburg, Germany; General Hospital, Dortmund, Germany; General Hospital, Biberach, Germany; Medical University, Hannover, Germany; University Hospital Aachen, Aachen, Germany; SKM Hospital, Koblenz, Germany; Municipal Hospital, Braunschweig, Germany; Municipal Hospital, Karlsruhe, Germany; University Hospital, Magdeburg, Germany; University Hospital, Kiel, Germany; University Hospital, Mainz, Germany; University Hospital, Halle, Germany; University Hospital, Freiburg, Germany; University Hospital, Jena, Germany; University Hospital, Münster, Germany; University Hospital, Homburg, Germany; University Hospital, Leipzig, Germany; University Hospital, Hamburg, Germany; University Hospital, Ulm, Germany; and Westpfalz Hospital, Kaiserslautern, Germany.
Author information
Authors and Affiliations
Corresponding author
Additional information
W. Lehmann and M. Hoffmann contributed equally and therefore share first authorship.
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at University Medical Center Hamburg-Eppendorf, Hamburg, Germany.
About this article
Cite this article
Lehmann, W., Hoffmann, M., Fensky, F. et al. What Is the Frequency of Nerve Injuries Associated With Acetabular Fractures?. Clin Orthop Relat Res 472, 3395–3403 (2014). https://doi.org/10.1007/s11999-014-3838-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-014-3838-9