Abstract
Purpose
The primary objective was to validate the construct validity of the Japanese Core Outcome Measures Index (COMI) in preoperative patients aged 60 years or older undergoing lumbar spine surgery for lumbar spinal stenosis (LSS) and lumbar disk herniation (LDH). Additionally, as a secondary aim, we explored the impact of these diseases on quality of life (QOL).
Methods
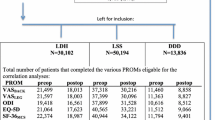
The analysis included 199 preoperative patients aged 60 and above who were scheduled for lumbar spine surgery. To assess QOL, Japanese versions of the COMI, Oswestry Disability Index (ODI), EuroQol-5 Dimension-3 Level (EQ-5D-3L), and SF-12v2 were employed. The study assessed the validity of the COMI and compared demographic and clinical characteristics between the LSS (147 cases) and LDH (52 cases) groups. It used multivariate covariance analysis (MANCOVA) to examine the impact of diseases (LSS and LDH) on each patient-reported outcome measure while considering covariates.
Results
Compared to the LSS group, the LDH group showed more difficulty with the COMI summary score (LSS/LDH [mean]: 6.9/8.1, p < 0.001), ODI score (46.8/57.4, p < 0.001), and EQ-5D utility (0.53/0.43, p < 0.001). The LDH group also reported more difficulties in the COMI-function, COMI-symptom-specific well-being, COMI-disability, ODI-personal care, ODI-social life, and SF-12v2-bodily pain subscales. MANCOVA demonstrated that these results were not influenced by covariates such as gender and medical history.
Conclusions
This study highlights the distinct impact of LSS and LDH on preoperative QOL in older patients undergoing lumbar spinal surgery. Tailored interventions are essential to address the specific challenges posed by these conditions and improve patient-centered outcomes and postoperative recovery.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Lumbar spinal stenosis (LSS) and lumbar disk herniation (LDH) often necessitate surgical intervention, impacting patients’ daily lives due to diverse symptoms and progression patterns [1, 2]. While both conditions affect the lumbar spine, LSS involves canal narrowing, leading to nerve compression and related symptoms, whereas LDH involves disk protrusion or rupture, causing pain and functional impairment. Lumbar spine surgery has been shown to improve the overall quality of life (QOL) for these conditions [3], yet no studies have examined preoperative QOL-related patient-reported outcome measures (PROMs) subscales. Investigating specific PROM subscales for each condition can inform tailored postoperative rehabilitation, addressing individual needs more effectively.
Various PROMs have been developed to assess the impact of LSS and LDH on patients’ QOL. The utilization of a variety of PROMs provides several advantages [4]. These assessments enable a comprehensive evaluation of the multifaceted impacts of LSS and LDH on patients’ well-being, encompassing physical symptoms and broader psychosocial consequences. As such, this study employed the Japanese Core Outcome Measures Index (COMI) [5, 6], the Japanese Oswestry Disability Index (ODI) [7], EuroQol-5 Dimension-3 level (EQ-5D-3L) [8], and SF-12v2 [9]. The COMI has shown reliability among patients undergoing thoracic and lumbar spinal surgeries [5, 6]. COMI comprehensively covers different facets of other PROMs through a single questionnaire. However, the construct validity of the Japanese COMI tailored explicitly to patients undergoing lumbar spinal surgery remains to be established. The validation conducted in this study is expected to streamline the assessment process and alleviate the burden on patients by reducing the number of questionnaires.
Furthermore, focusing on individuals aged 60 years and older holds particular significance. This age group is susceptible to degenerative spinal conditions and constitutes a substantial portion of patients seeking surgical intervention [10, 11]. Notably, lumbar surgery in elderly individuals has been associated with less pronounced improvements in health-related quality of life (HRQOL) when compared to their younger counterparts [12, 13]. Gaining insights into the distinct challenges faced by these older individuals can inform preoperative care and postoperative rehabilitation strategies [14].
Therefore, this study targets patients with LSS and LDH aged 60 and above undergoing lumbar spine surgery. The primary objective is to validate the construct validity of the COMI and examine its correlations with other traditional PROMs. The secondary objective is to investigate differences in the impact of LSS or LDH on QOL.
Methods
Study design and participants
This cross-sectional study compared the QOL of preoperative patients aged 60 years and above with LSS or LDH. The study adhered to the STROBE statement and received approval from the Institutional Review Board of Saitama Medical Center, Saitama Medical University (No. 1969-III). The study was conducted between April 2018 and May 2023. In this study, we classified individuals aged 60 and above as elderly, drawing from prior research on QOL assessments [15]. Patients aged 60 years and older, seeking consultation at our center and scheduled for lumbar spine surgery based on the assessment of surgical eligibility for LSS or LDH, were enrolled in the study. In this study, cases of LSS did not involve a prolapsed nucleus pulposus contributing to lower limb neurological symptoms, and surgical procedures on the intervertebral disk were not conducted in these instances. Specifically, decompression was achieved by removing vertebral arch, partial facet, and/or ligamentum flavum. Conversely, cases of LDH were diagnosed based on the identification of compression on the cauda equina and/or nerve roots caused by a prolapsed nucleus pulposus through preoperative imaging, such as MRI. Furthermore, intraoperative observations confirmed the presence of herniated disks, leading to the performance of herniotomy and discectomy. Among the 251 patients scheduled for surgery, 79.2% (199 individuals, including 147 diagnosed with LSS and 52 with LDH) completed all necessary PROMs and were consequently included in the final analysis.
Demographic and clinical characteristics
The participants’ baseline demographic and clinical characteristics were collected, including age, sex, body mass index (BMI: kg/m2), ASA classification, smoking status, history of diabetes, hypertension, hyperlipidemia, and arrhythmia (Table 1). The variables, including these comorbidities, were extracted from the medical records of each patient as documented by the attending physician.
PROMs evaluation
To assess the preoperative QOL of patients, the following PROMs were utilized: Japanese COMI, Japanese ODI, EQ-5D-3L, and SF-12v2. The patients filled out these questionnaires at the point when the decision for lumbar spine surgery was determined. The severity of lumbar symptoms was assessed using the COMI questionnaire, which covers five domains: pain, function, symptom-specific well-being (SSWB), general QOL, and disability [6].
The COMI encompasses seven elements: back pain, leg/buttock pain, function, symptom-specific well-being, general quality of life, social disability, and work disability. All assessments pertain to the preceding week, except for the two disability items, which consider the past four weeks. Back and leg/buttock pain are evaluated on distinct 10-point graphic rating scales, while the remaining items are rated on a 5-point scale. A higher score indicates a more unfavorable status. Calculations are performed for individual domains and a summary score [16]. The higher score between back or leg/buttock pain is initially chosen as the pain domain score for the latter. Subsequently, the scores for other items are converted from their 5-point scales to a 0 to 10-point range using 2.5-point increments (0, 2.5, 5.0, 7.5, 10.0). Social and work disability scores are averaged to create a unified disability domain score. The summary score results from averaging the five domain scores (now each scored 0–10)—pain, function, symptom-specific well-being (SSWB), general quality of life, and disability—providing a comprehensive score ranging from 0 to 10 (representing the best to worst health status) [17, 18]. In this study, we utilized the Japanese version of the COMI, which has been previously validated for cross-cultural adaptation [6]. The ODI questionnaire evaluated the impact of lumbar pain on daily life [19]. The ODI comprises ten items related to daily activities, sleep, and social functioning. Each item is scored on a scale of 0 to 5, with higher total scores indicating more significant disability. The ODI score is calculated by dividing the sum of the scores by 50 and expressing it as a percentage, ranging from 0 to 100. EQ-5D-3L is a questionnaire that comprehensively assesses HRQOL based on five dimensions: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Each dimension is scored on a scale of 1 to 3, with higher scores indicating more problems [20, 21]. The utility score is derived from these five dimensions and ranges from 0 (or negative) to 1, where 1 represents perfect health and lower scores indicate poorer health. The SF-12v2 questionnaire provides a comprehensive measurement of patients’ physical and mental health status, comprising eight health domains: physical functioning, role physical, bodily pain, general health, vitality, social functioning, emotional role limitations, and mental health [22]. Summary scores can be calculated from these domains, including physical component summary (PCS), mental component summary (MCS), role component summary (RCS), and norm-based scores. Considering biases due to fatigue and stress, the order of responding to these PROMs was randomized. To capture patients’ responses to these PROMs more accurately, they completed them in a separate room away from the physician’s presence. In cases of any questions or concerns, dedicated administrative staff assisted.
Sample size
We calculated the sample size using the G*Power software for power analysis (http://www.gpower.hhu.de/). Since there have been no previous studies of this nature, we estimated the effect size (d) for the independent t test to compare the results of each PROM between the LSS and LDH groups as 0.5 (Medium, α = 0.05, 1-β = 0.8). Furthermore, considering the ratio of elderly LSS to LDH patients in our hospital (3:1), the number of subjects needed for the t test was determined to be at least 170 (LSS: 127 cases, LDH: 43 cases). Therefore, the number of cases in this study can be considered sufficient.
Statistical analysis
IBM SPSS Statistics for Windows, Version 29.0, was used for all statistical analyses, with a significance level of p = 0.05.
Construct validity of the Japanese COMI
Relying on prior research [5], we evaluated the construct validity of the preoperative COMI score and other PROMs using Spearman’s correlation coefficient.
Impact of lumbar spinal conditions on PROMs and PROMs subscales
The Mann–Whitney U test and χ2 test were employed for continuous and categorical variables, respectively, to compare baseline PROMs and demographic information between the LSS and LDH groups. Additionally, a multivariate covariance analysis (MANCOVA) was performed to examine whether diseases (LSS and LDH) influenced the composite scores of each PROM and subscales. The dependent variables were the combined scores of each PROM or subscales of PROMs; the fixed factor was diseases, and covariates included gender, ASA classification, smoking status, history of diabetes, hypertension, hyperlipidemia, and arrhythmia. By conducting this analysis, we can demonstrate whether covariates influence the comparison results between the two groups or reflect of the impact of the diseases (LSS or LDH). Post hoc power analysis was conducted using G*Power 3.1.9.7.
Results
Construct validity of the Japanese COMI
Correlations between the COMI core index score, COMI subscales, and various PROMs are shown in Table 2. A positive correlation was observed between the COMI core index score and ODI (ρ = 0.73, p < 0.001), while negative correlations were noted with EQ-5D-3L (ρ = −0.71, p < 0.001) and SF-12v2 (PCS: ρ = −0.29, p < 0.001; MCS: ρ = −0.280, p < 0.001; RCS: ρ = −0.43, p < 0.001).
Impact of lumbar spinal conditions on PROMs and PROMs subscales
The results of the comparison of PROMs between the two groups are presented in Table 3. In comparing PROMs, the LDH group exhibited higher values in the COMI summary score, as well as in the function and disability subscales of COMI. The LDH group also showed higher values in the ODI score, along with the personal care, sexual life, and social life subscales of ODI. The EQ-5D-3L utility score was lower in the LDH group, with no significant differences observed in the subscales. While no significant differences were found in the component scores of SF-12v2, the LDH group had lower values in the bodily pain subscale.
The results of the MANCOVA are presented in Table 4. There was a significant overall impact of diseases (LSS and LDH) on PROMs and their subscales. Even after adjusting for covariates such as gender and comorbidities, diseases had a significant effect on COMI Core Index, ODI score, EQ-5D utility score, COMI-function, COMI-SSWB, COMI-disability, ODI-personal care, ODI-social life, and SF-12v2-bodily pain.
Discussion
The objective of this study was to validate the construct validity of the Japanese COMI in patients aged 60 and above undergoing lumbar spine surgery and to investigate the differential impact of LSS and LDH on QOL. The results of this study demonstrated the construct validity of the Japanese COMI, revealing the distinct impacts of LSS and LDH on each PROMs assessed. The LDH group exhibited higher values compared to the LSS group in the COMI summary score, COMI function and disability subscales, ODI score, and ODI subscales for personal care, sexual life, and social life. These findings suggest a more pronounced decrease in QOL among the LDH group. The findings of our MANCOVA highlighted the significant impact of both LSS and LDH on various PROMs, even after adjusting for covariates such as gender, ASA classification, smoking status, and medical history.
These results are consistent with the differing clinical presentations of LSS and LDH in the elderly [2]. Patients with LDH often experience more pronounced pain and functional limitations due to the compression of nerve roots caused by herniated disks. This could explain the higher values observed in the ODI and COMI subscales related to functional limitations and disability. Additionally, the lower values in the EQ-5D-3L utility score in the LDH group may reflect the greater impact of pain and discomfort on their HRQOL. Furthermore, the absence of significant differences in the SF-12v2 component scores between the two groups suggests that the impact of these conditions on overall physical and mental health may not vary significantly. However, the LDH group exhibited lower values on the physical pain subscale, possibly due to more localized pain linked to the herniated disk. Prior studies have noted that lower extremity pain is a contributing factor to reduced QOL in patients with LDH [23]. Moreover, the intensity of preoperative pain has been identified as a predictor of diminished postoperative QOL [24]. Notably, patients with LDH often experience lingering back pain post-surgery [25], and their fear-avoidance beliefs concerning pain have been associated with unfavorable prognoses [26]. This emphasizes the heightened importance of postoperative care [27]. In addition, both groups showed significantly lower PCS and physical functioning scores on the SF-12v2 compared to the national norm (mean: PCS, 44.3; Physical Functioning, 46.1) in the 70–79 age group. Given the scenarios where patients with LSS experience central stenosis accompanied by neurogenic claudication, lateral stenosis leading to nerve root impairment, and combined syndromes that necessitate surgical interventions, the compromised quality of life for these individuals is unsurprising. Therefore, post-surgery, rehabilitation objectives should encompass enhancing overall physical and mental well-being while addressing each distinct symptom [28,29,30].
Importantly, the use of PROMs offers valuable insights into patients’ subjective experiences and functional limitations. By evaluating these PROMs preoperatively, healthcare providers can identify the specific domains of QOL that are most affected by LSS and LDH. This knowledge can guide preoperative counseling, surgical decision-making, and postoperative rehabilitation strategies tailored to each patient’s needs.
While providing valuable insights into the divergent impact of LSS and LDH on the QOL of older patients undergoing lumbar spinal surgery, our study has certain limitations. Conducted within a single institution, the mono-center approach may limit generalizability. A multicenter study encompassing diverse settings would offer a more comprehensive perspective. Additionally, the cross-sectional design restricts our ability to establish causality or explore temporal relationships. Further investigation into the predictive value of preoperative QOL assessments for postoperative outcomes is warranted, ideally through prospective studies collecting data from the same patient cohort. It is essential to consider factors like physical function, social role, health literacy, and surgical expectations, which influence postoperative QOL. The focus on patients aged 60 years and above introduces potential selection bias, cautioning against extrapolating findings to younger populations. Additionally, it is not uncommon for variations in physical function and living conditions to occur with advancing age, potentially leading to diverse impacts on QOL. While our research investigated differences related to specific medical conditions, future studies examining variations based on age could further enhance rehabilitation medicine practices. Addressing these limitations will enhance the robustness and applicability of our findings in clinical practice.
Conclusions
In conclusion, the construct validity of the Japanese COMI was confirmed for patients aged 60 and above undergoing lumbar spine surgery, demonstrating its effectiveness in assessing this patient population. Additionally, utilizing PROMs allowed for a comprehensive evaluation of the multifaceted impacts of these conditions on patients’ lives, revealing a greater decline in QOL among patients with LDH. These findings underscore the need for tailored interventions to address the specific challenges posed by LSS and LDH, ensuring improved patient-centered outcomes and enhanced postoperative recovery.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Chou R, Baisden J, Carragee EJ, et al (2009) Surgery for low back pain: a review of the evidence for an American Pain Society Clinical Practice Guideline. Spine (Phila Pa 1976) 34:1094–1109. https://doi.org/10.1097/BRS.0b013e3181a105fc
Rainville J, Lopez E (2013) Comparison of radicular symptoms caused by lumbar disc herniation and lumbar spinal stenosis in the elderly. Spine (Phila Pa 1976) 38:1282–1287. https://doi.org/10.1097/BRS.0b013e31828f463e
HWD Hey N Luo SY Chin 2018 The predictive value of preoperative health-related quality-of-life scores on postoperative patient-reported outcome scores in lumbar spine surgery Global Spine J 8 156 163 https://doi.org/10.1177/2192568217701713
D Lubelski MD Alvin S Nesterenko 2016 Correlation of quality of life and functional outcome measures for cervical spondylotic myelopathy J Neurosurg Spine 24 483 489 https://doi.org/10.3171/2015.6.SPINE159
K Nagata Y Oshima H Nakamoto 2020 Validity of the Japanese Core Outcome Measures Index (COMI)-Back for thoracic and lumbar spine surgery: a prospective cohort study Eur Spine J 29 1435 1444 https://doi.org/10.1007/s00586-019-06249-x
K Matsudaira H Oka Y Oshima 2018 Development of the Japanese Core Outcome Measures Index (COMI): cross-cultural adaptation and psychometric validation BMC Musculoskelet Disord 19 71 https://doi.org/10.1186/s12891-018-1986-x
H Hashimoto M Komagata O Nakai 2006 Discriminative validity and responsiveness of the Oswestry Disability Index among Japanese outpatients with lumbar conditions Eur Spine J 15 1645 1650 https://doi.org/10.1007/s00586-005-0022-7
A Tsuchiya S Ikeda N Ikegami 2002 Estimating an EQ-5D population value set: the case of Japan Health Econ 11 341 353 https://doi.org/10.1002/hec.673
H Takasaki 2022 Cross-cultural adaptation of the Satisfaction and Recovery Index among Japanese people with musculoskeletal disorders J Phys Ther Sci 34 374 378 https://doi.org/10.1589/jpts.34.374
W Brinjikji PH Luetmer B Comstock 2015 Systematic literature review of imaging features of spinal degeneration in asymptomatic populations AJNR Am J Neuroradiol 36 811 816 https://doi.org/10.3174/ajnr.A4173
RP Jackson AC McManus J Moore 2012 Lumbar spinal stenosis: treatment options for an aging population Mo Med 109 466 469
F Strömqvist B Strömqvist B Jönsson MK Karlsson 2016 The outcome of lumbar disc herniation surgery is worse in old adults than in young adults Acta Orthop 87 516 521 https://doi.org/10.1080/17453674.2016.1205173
M Halicka M Wilby R Duarte C Brown 2023 Predicting patient-reported outcomes following lumbar spine surgery: development and external validation of multivariable prediction models BMC Musculoskelet Disord 24 333 https://doi.org/10.1186/s12891-023-06446-2
JG Marwell MT Heflin SR McDonald 2018 Preoperative screening Clin Geriatr Med 34 95 105 https://doi.org/10.1016/j.cger.2017.08.004
RR Marzo P Khanal S Shrestha 2023 Determinants of active aging and quality of life among older adults: systematic review Front Public Health 11 1193789 https://doi.org/10.3389/fpubh.2023.1193789
L Pochon FS Kleinstück F Porchet AF Mannion 2016 Influence of gender on patient-oriented outcomes in spine surgery Eur Spine J 25 235 246 https://doi.org/10.1007/s00586-015-4062-3
AF Mannion A Elfering R Staerkle 2005 Outcome assessment in low back pain: how low can you go? Eur Spine J 14 1014 1026 https://doi.org/10.1007/s00586-005-0911-9
Mannion AF, Porchet F, Kleinstück FS, et al (2009) The quality of spine surgery from the patient’s perspective. Part 1: the Core Outcome Measures Index in clinical practice. Eur Spine J 18(Suppl 3):367–373. https://doi.org/10.1007/s00586-009-0942-8
Fujiwara A, Kobayashi N, Saiki K, et al (2003) Association of the Japanese Orthopaedic Association score with the Oswestry Disability Index, Roland-Morris Disability Questionnaire, and short-form 36. Spine (Phila Pa 1976) 28:1601–1607
EuroQol Group 1990 EuroQol–a new facility for the measurement of health-related quality of life Health Policy 16 199 208 https://doi.org/10.1016/0168-8510(90)90421-9
T Shiroiwa T Fukuda S Ikeda 2016 Japanese population norms for preference-based measures: EQ-5D-3L, EQ-5D-5L, and SF-6D Qual Life Res 25 707 719 https://doi.org/10.1007/s11136-015-1108-2
Singh A, Gnanalingham K, Casey A, Crockard A (2006) Quality of life assessment using the Short Form-12 (SF-12) questionnaire in patients with cervical spondylotic myelopathy: comparison with SF-36. Spine (Phila Pa 1976) 31:639–643. https://doi.org/10.1097/01.brs.0000202744.48633.44
D Ionescu CI Iacob FM Brehar E Avram 2023 The role of catastrophizing and basic psychological needs satisfaction on health-related quality of life and pain in patients with lumbar disc herniation Front Psychol 14 1147254 https://doi.org/10.3389/fpsyg.2023.1147254
K Silverplats B Lind B Zoega 2011 Health-related quality of life in patients with surgically treated lumbar disc herniation Acta Orthop 82 198 203 https://doi.org/10.3109/17453674.2011.566136
T Toyone T Tanaka D Kato R Kaneyama 2004 Low-back pain following surgery for lumbar disc herniation. A prospective study J Bone Joint Surg Am 86 893 896 https://doi.org/10.2106/00004623-200405000-00001
J Rainville RJEM Smeets T Bendix 2011 Fear-avoidance beliefs and pain avoidance in low back pain–translating research into clinical practice Spine J 11 895 903 https://doi.org/10.1016/j.spinee.2011.08.006
D Claus E Coudeyre J Chazal 2017 An evidence-based information booklet helps reduce fear-avoidance beliefs after first-time discectomy for disc prolapse Ann Phys Rehabil Med 60 68 73 https://doi.org/10.1016/j.rehab.2015.10.008
N Hara H Oka T Yamazaki 2010 Predictors of residual symptoms in lower extremities after decompression surgery on lumbar spinal stenosis Eur Spine J 19 1849 1854 https://doi.org/10.1007/s00586-010-1374-1
D Yan Z Zhang Z Zhang 2020 Residual leg numbness after endoscopic discectomy treatment of lumbar disc herniation BMC Musculoskelet Disord 21 273 https://doi.org/10.1186/s12891-020-03302-5
JD Lurie TD Tosteson ANA Tosteson 2014 Surgical versus nonoperative treatment for lumbar disc herniation: eight-year results for the spine patient outcomes research trial Spine 39 3 https://doi.org/10.1097/BRS.0000000000000088
Funding
Open Access funding provided by Saitama Medical University. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript. The manuscript submitted does not contain information about medical device (s)/drug (s).
FDA device/drug status
Not applicable.
Author disclosure
YM: Nothing to disclose. KA: Nothing to disclose. KS: Nothing to disclose. FK: Nothing to disclose. TH: Nothing to disclose. SO: Nothing to disclose.
Ethical Approval
The study received approval from the Institutional Review Board of Saitama Medical Center, Saitama Medical University (No. 1969-III). A disclosure statement was posted on the website, with contact information for refusal to use the data for research, and the data of eligible patients who were notified of the refusal would not be used.
Informed consent
A disclosure statement was posted on the website, with contact information for refusal to use the data for research, and the data of eligible patients who were notified of the refusal would not be used.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mizoguchi, Y., Akasaka, K., Suzuki, K. et al. Construct validation of the Japanese Core Outcome Measures Index and the impact of diseases on patient-reported outcome measures in preoperative patients with lumbar spinal stenosis and disk herniation: a single-center observational study. Eur Spine J (2024). https://doi.org/10.1007/s00586-024-08148-2
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00586-024-08148-2