Abstract
Purpose
To review existing classification systems for degenerative spondylolisthesis (DS), propose a novel classification designed to better address clinically relevant radiographic and clinical features of disease, and determine the inter- and intraobserver reliability of this new system for classifying DS.
Methods
The proposed classification system includes four components: 1) segmental dynamic instability, 2) location of spinal stenosis, 3) sagittal alignment, and 4) primary clinical presentation. To establish the reliability of this system, 12 observers graded 10 premarked test cases twice each. Kappa values were calculated to assess the inter- and intraobserver reliability for each of the four components separately.
Results
Interobserver reliability for dynamic instability, location of stenosis, sagittal alignment, and clinical presentation was 0.94, 0.80, 0.87, and 1.00, respectively. Intraobserver reliability for dynamic instability, location of stenosis, sagittal alignment, and clinical presentation were 0.91, 0.88, 0.87, and 0.97, respectively.
Conclusion
The UCSF DS classification system provides a novel framework for assessing DS based on radiographic and clinical parameters with established implications for surgical treatment. The almost perfect interobserver and intraobserver reliability observed for all components of this system demonstrates that it is simple and easy to use. In clinical practice, this classification may allow subclassification of similar patients into groups that may benefit from distinct treatment strategies, leading to the development of algorithms to help guide selection of an optimal surgical approach. Future work will focus on the clinical validation of this system, with the goal of providing for more evidence-based, standardized approaches to treatment and improved outcomes for patients with DS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Degenerative spondylolisthesis (DS) is a progressive, often debilitating spinal disorder that is among the most common indications for lumbar spine surgery in older adults [1]. In contrast to dysplastic or isthmic subtypes, DS is an acquired vertebral subluxation with an intact posterior arch, most characteristically involving anterior displacement L4 on L5 [2]. The development of degenerative olisthesis begins with desiccation of the intervertebral disc that leads to altered spinal load-bearing dynamics and an increased load on the facet joints, resulting in circumferential segmental pathology including segmental hypermobility and facet arthropathy. Over time, the degenerative cascade leads to the development of symptomatic lumbar spinal stenosis (LSS), degenerative spondylolisthesis, and progressive deformity [3, 4]. The structural pathology of degenerative spondylolisthesis is variable and may involve central, lateral recess or foraminal stenosis, and segmental instability with malalignment. The clinical presentation of patients with degenerative spondylolisthesis is also variable and may include combination of back pain, leg pain or radiculopathy, sensorimotor deficits, and symptoms of neurogenic claudication [5, 6].
For symptomatic patients, the benefits of operative intervention have been well established by several large-scale randomized controlled trials [7,8,9]. However, the optimal surgical strategy for the individual patient continues to be a subject of debate [10]. The role of decompression alone or decompression with segmental stabilization remains unclear for many patients and providers [11,12,13]. The absence of an evidence-based approach to the management of degenerative spondylolisthesis leads to the observed variation in treatment [14, 15]. Applying principles of precision medicine to degenerative spondylolisthesis may empower patients and providers to make informed choices. Specifically, consideration of the precise clinical and radiographic characteristics of degenerative spondylolisthesis may guide appropriate care for the individual patient.
As our understanding of the pathophysiology, natural history, and prognosis of DS has evolved, it has become increasingly apparent that the condition encompasses a wide spectrum of pathologies that may require different approaches to surgical treatment. This structural, radiographic, and clinical heterogeneity is poorly accounted for in current practices of diagnosis, treatment, and comparative evaluation, likely underlying the inconsistencies observed in the literature. A more comprehensive system of classifying patients with DS into clinically distinct, functionally relevant subgroups may therefore help to guide the development of evidence-based algorithms for evaluation and treatment. The purpose of this paper is to review the established classification systems for DS and to propose a novel system that will capture the patient-specific features that are impactful in guiding informed surgical choice.
Current systems for classifying DS
Effective classification systems are developed to standardize four primary functions: (1) interprofessional communication, (2) research and data analysis, (3) treatment selection, and (4) prognostication. For a method to be widely accepted and adopted, it must also be easy to use, reliable, and clinically relevant. The following sections introduce current methods for classifying DS and discuss the ways in which they fail to achieve these objectives.
Overview of current classification methods
Meyerding classification
One of the earliest methods for describing spondylolisthesis was proposed by Henry Meyerding in 1932, which delineates five grades based on the degree of vertebral translation [16]:
-
Grade 1: < 25%
-
Grade 2: 25–50%
-
Grade 3: 50–75%
-
Grade 4: 75–100%
-
Grade 5 (spondyloptosis): > 100%
The Meyerding classification is a simple, highly reliable technique that remains one of the most widely recognized methods for characterizing spondylolisthesis. However, beyond providing a standardized description of vertebral translation, there is relatively limited practical utility in using the Meyerding classification to differentiate between patients with DS given that most cases would be categorized as mild (Meyerding grade 1), and slippage rarely exceeds 30% [17]. Furthermore, slip severity and progression correlate poorly with patient symptoms and response to treatment, and therefore cannot be used in isolation to inform clinical practice [17]. Ultimately, classification based solely on olisthesis provides an inadequate description of the complex, clinically relevant features of DS that are fundamental in guiding treatment.
French Society for Spine Surgery (FSSS) classification system
In 2014, the French Society for Spine Surgery (FSSS) proposed a novel classification system for degenerative lumbar spondylolisthesis based on segmental, regional, and global sagittal alignment patterns [18, 19]. Adapted from a classification of adult spinal deformity proposed by Schwab et al. [20], this system uses radiographic measurements of sagittal vertical axis (SVA), L1-S1 lumbar lordosis (LL), segmental lordosis (SL), pelvic incidence (PI), and pelvic tilt (PT) to classify DS into one of three main types.
-
Type 1: normal sagittal alignment (PI-LL < 10°).
-
1A: with preserved segmental lordosis (SL >5°)
-
1B: with loss of segmental lordosis (SL <5°)
-
-
Type 2: compensated malalignment (PI-LL > 10°)
-
2A: without pelvic compensation (PT < 25°)
-
2B: with pelvic compensation (PT > 25°)
-
-
Type 3: global sagittal malalignment (SVA > 4 cm).
Although a purely radiographic classification, increasing FSSS type has been correlated with pre- and postoperative patient-reported health-related quality of life (HRQoL) measures [18, 21]. Associated recommendations for treatment are provided, drawing parallels to approaches employed in adult deformity surgery. However, this discussion primarily focuses on the implications of progressively severe malalignment on procedural selection and does not address the influence of other disease-specific structural or clinical features on surgical decision-making.
Clinical and radiographic degenerative spondylolisthesis (CARDS) classification
Also published in 2014, the clinical and radiographic degenerative spondylolisthesis (CARDS) classification categorized DS into four main types based on three radiographic features (disc height, vertebral translation, and segmental alignment) [22]. Although not part of the core defining criteria, a subcategory modifier of leg pain (0: absent, 1: unilateral, 2: bilateral) was also included, representing the first incorporation of a clinical component to classification.
-
Type A: advanced disc collapse without kyphosis.
-
Type B: disc height partially preserved with ≤ 5 mm translation.
-
Type C: disc height partially preserved with > 5 mm translation.
-
Type D: segmental kyphosis.
External clinical validation studies have found the CARDS classification easy to use and reliable, highlighting the importance of segmental lumbar kyphosis in predicting baseline symptom severity and potential for postoperative improvement [21, 23, 24]. However, this system focuses solely on structural derangement at the level of olisthesis and does not consider regional or global alignment patterns, which can be important factors influencing surgical management. Additionally, as originally described, treatment recommendations are not provided.
Degenerative spondylolisthesis instability classification (DSIC)
The degenerative spondylolisthesis instability classification (DSIC) was proposed in 2015 as a qualitative guide for procedural selection based on an assessment of baseline spinal stability [25]. Developed from the significant findings of an extensive systematic review of biomechanical and clinical studies of spinal stability in DS, this system included a combination of radiographic and clinical factors including back pain, restabilization signs (disc height loss, osteophyte formation, and endplate sclerosis), facet joint effusion, disc angle, and magnitude of dynamic translation.
-
Type I (stable): decompression alone.
-
Type II (potentially unstable): decompression with posterior fusion.
-
Type III (unstable): decompression and posterior fusion with interbody placement.
In addition to providing a comprehensive assessment of the salient findings of key evaluating instability in DS, this review functioned to highlight the how the development of evidence-based treatment guidelines has been limited by the relatively low quality of data available.
However, this classification system proposes a surgical decision-making strategy solely centered on an assessment of stability that does not consider other structural and clinical features known to influence surgical management.
Sagittal vertical axis (SVA)
In 2019, Kobayashi et. al published an investigative cross-sectional study of sagittal alignment patterns in DS [26]. Patients were first classified according to SVA using thresholds described by the Scoliosis Research Society (SRS)–Schwab Classification for adult spinal deformity [20].
-
Type 1: SVA < 40 mm.
-
Type 2: 40 mm ≤ SVA < 95 mm.
-
Type 3: SVA ≥ 95 mm.
Additional measurements of TK, LL, PT, PI, and sacral slope (SS) were recorded for all patients as well as volunteers without lumbar pathology and patterns of alignment were compared between groups. Significant differences in spinopelvic alignment were observed with progressively more severe global deformity, providing insight into the functional progression of malalignment in DS. Nevertheless, this study did not address clinical disease status or associated treatment implications, and therefore does little to directly inform management.
Kulkarni scoring system
The Kulkarni scoring system was proposed in 2020 with the goal of providing a simple tool for evaluating the need for a spinal fusion in patients with DS [27, 28]. A weighted scoring system was created based on multiple clinical, radiographic, and technical metrics. A fusion is recommended if the cumulative score exceeds 5.5 [28].
-
(+ 2) Mechanical back pain.
-
(+ 1) Age < 70 years.
-
(+ 1) High-demand activity.
-
(+ 1.5) Segmental kyphosis.
-
(+ 1) Dynamic translation > 2 mm.
-
(+ 1) Disc height > 50% of adjacent level.
-
(+ 1) Bilateral facet effusion on MRI.
-
(+ 1) Sagittal facet orientation.
-
(+ 1.5) Feasibility of performing a decompression without compromising stability.
Although highly reproducible and easy to use, the major limitations of this system stem from its rigid structure, which does not consider how different combinations of specific features, even with similar cumulative scores, may be optimally managed in different ways. For example, although the authors do underscore the importance of mechanical back pain in prompting spinal fusion, assigning 2 points to this category, many would consider the presence of mechanical back pain a proxy for instability that should be managed with spinal fusion regardless of additional risk factors.
Summary of current classification systems
The earliest, and most widely recognized classification systems were introduced as simple methods for characterizing all types of spondylolisthesis based on etiology (Wiltse) [2] or magnitude of vertebral slippage (Meyerding) [16]. With closer focus on DS, classifications have increased in complexity in attempts to reflect the observed heterogeneity of clinical and radiographic presentations in this condition (Table 1).
The UCSF DS classification system
Overview of the UCSF DS classification system
Review of the landscape of current techniques for characterizing DS highlights the need for a comprehensive classification system that better accounts for the fundamental disease-specific features that guide surgical management. Here at the University of California, San Francisco, we have attempted to address the limitations of earlier methods by developing a classification for DS based on four interrelated, yet distinct principles that may guide surgical intervention:
-
1.
Preserve biomechanical stability
-
2.
Relieve neurologic compression
-
3.
Maintain structural alignment
-
4.
Alleviate patient symptoms
Recognition of the important influence that each has on the approach to diagnosis, treatment, and prognostication in DS prompted selection of four main criteria for this proposed classification.
-
1.
Segmental dynamic instability
-
2.
Location of spinal stenosis
-
3.
Sagittal alignment
-
4.
Primary clinical presentation
These four criteria represent a novel combination of characteristics that have not previously been included within a single classification (Table 2).
The proposed UCSF DS classification is displayed in Table 3. This classification system considers the important, independent influence that each category has for guiding surgical management of DS, a notable advantage over a cumulative point-based system. Within each category, the specific parameters evaluated were selected based on established correlations with patient-reported HRQOL metrics as well as their importance for influencing surgical approach.
UCSF DS classification system components: rationale
Spinal instability
Ensuring biomechanical stability is a fundamental goal of surgery in patients with DS. In patients deemed high risk for postoperative instability, either from the underlying disease process or a result of the planned surgical procedure, a concomitant fusion should be performed to prevent complications related to symptom recurrence, deformity progression, and revision surgery. Instrumented fusions are generally preferred, given higher observed rates of successful fusion with these constructs. Placement of an interbody device may also be used to augment fusion and reinforce the anterior weight-bearing column, which may lead to better outcomes in patients with excessive segmental mobility [29]. However, fusions are more financially costly, invasive procedures that carry additional risks for adjacent segment degeneration[23] and instrumentation-related complications [30]. Nevertheless, concern for postoperative instability has prompted fusion in nearly 95% of surgically treated cases of DS [31].
The development of vertebral slippage in DS is thought to occur because of segmental instability, which is often the source of patient symptoms in earlier stages of disease. In these cases, the addition of a fusion is suggested to provide superior symptomatic relief and prevention of associated complications [32]. However, the natural history of DS ultimately progresses to a stage of restabilization [4]. In the appropriately selected patient, decompression alone has been shown to provide adequate, durable symptomatic relief and avoids risks related to instrumentation [28]. As such, neither the presence nor magnitude of static vertebral slippage, such as provided by the Meyerding classification, necessarily indicates ongoing instability in need of surgical stabilization. As a result, stability assessments typically focus on the presence of dynamic instability in determining the need for a fusion.
Traditionally, the presence of > 3 mm of translation on dynamic radiographs has been used [25]. However, a number of clinical outcomes studies have suggested that a threshold of > 5 mm may be used as well [33]. Inui et al.[34] compared clinical and radiographic outcomes in patients who underwent decompression alone or fusion with interbody placement and found that a clinically significant benefit to interbody fusion was present in patients with > 5 mm of preoperative dynamic olisthesis but not those with 3-5 mm or < 3 mm of dynamic olisthesis. Following systematic review, the proposed DSIC system found both thresholds to be important in patients with DS [25].
Location of lumbar stenosis
Lumbar spinal stenosis (LSS), characterized by a pathologic narrowing of the central canal, lateral recess, or neural foramen, is a relatively common cause of symptoms in patients with DS [35]. Soft tissue or bony encroachment caused by facet joint arthrosis, reactive ligamentous hypertrophy, and/or intervertebral disc herniation can be effectively managed with direct surgical resection of compressive elements, classically through a posterior approach. In most straightforward cases of central or lateral recess stenosis, this can generally be achieved with a traditional laminectomy, laminotomy, or foraminotomy procedure.
In contrast, a wider, more lateral exposure may be necessary to address foraminal stenosis, in many cases requiring partial or complete removal of the facet joint(s). Given the particularly destabilizing effects of a facetectomy [36], a concomitant fusion is often performed to prevent iatrogenic instability [37]. Highlighted by the Spinal Laminectomy vs. Instrumented Pedicle Screw (SLIP) Trial, the destabilizing effects of a wide decompression may be particularly important in patients with LSS and DS. Among patients with Meyerding Grade 1 DS without overt clinical or radiographic signs of instability preoperatively, those treated with decompression alone (wide laminectomy and partial facetectomy) had significantly higher rates of revision surgery compared to those who underwent posterolateral instrumented fusion (34% vs 14%, p = 0.05); the indications in all cases were same-segment instability versus junctional complications, respectively, raising concerns for iatrogenic destabilization [11].
Foraminal stenosis can result from anteroposterior (transverse), craniocaudal (“up-down”), or circumferential pathologic changes in vertebral anatomy [38]. Hasegawa established that a foraminal height less than or equal to 15 mm and a posterior disc height of less than or equal to 4 mm were significant identifiers of lumbar foraminal stenosis [39]. Anteroposterior foraminal stenosis can be caused by facet arthropathy dorsally, foraminal disc protrusion ventrally, or anterior subluxation of the superior facet [39, 40]. The combination of hypertrophy of the ligamentum flavum and development of osteophytes in response to changes in biomechanical force distribution can further worsen transverse foraminal stenosis. Foraminal stenosis without “up-down” stenosis, or transverse only stenosis, may be corrected through decompression alone.
With more advanced degenerative disease, significant disc collapse, olisthesis or other malalignment may result in a vertical, rather than horizontal, narrowing of the neurovascular channels of the spine. Craniocaudal foraminal stenosis can occur due to degenerative loss in disc height that leads to pedicle-on-pedicle contact between vertebrae. Protrusion of posterolateral osteophytes on the vertebral endplates may also impinge the nerve in an “up-down” manner as its traverses the foraminal canal [40]. This stenosis often cannot be adequately addressed with direct resection of the posterior elements alone [41, 42]. In these cases, vertebral distraction with placement of an interbody device can be performed to restore disc height and prevent ligamentous buckling, thereby indirectly decompressing neural structures [43, 44]. While correcting foraminal stenosis may sometimes be amenable to decompression alone, restoring foraminal height through fusion is an effective way to restore foraminal space [45].
Despite its relative prevalence in DS, importance in determining symptomatic presentation, and role in dictating surgical approach, the location of LSS has not been formally incorporated into any existing classification system.
Sagittal alignment
As illustrated in the study by Kobayashi et al. [26], progressive loss of local, regional, and global sagittal balance is observed in patients with DS. Focal malalignment is often an early finding, manifesting with disc angle changes at the level of olisthesis. Clinically, the development of focal lumbar kyphosis has been shown to be particularly disabling, though strongly responsive to surgical correction [22, 23, 46]. If left untreated, progression of focal malalignment can lead to loss of regional lordosis, and ultimately more significant global deformity [18, 19, 26].
However, segmental kyphosis or global malalignment may also be a postural response to pain or symptomatic stenosis [47]. Recognizing structural versus compensatory changes in alignment is important in determining treatment.
Given the strong linear correlation between both SVA [48] and PT [49] and functional outcomes in patients with lumbar pathology, these parameters are often used to guide surgical correction and assess procedural success. In DS, a postoperative SVA > 5 cm has been linked with poor outcomes after fusion surgery [50, 51]. Similarly, a high PT has been shown to particularly impair functional ambulation [49], and insufficient postoperative restoration of balanced pelvic version has been identified as an independent predictor of persistent low back pain in patients with DS [52]. Thus, a comprehensive evaluation of alignment in DS must consider pre- and postoperative measures of global (SVA, PT), regional (LL, PI), and focal (disc angulation) sagittal balance [53].
Clinical presentation
Clinical presentation, in particular the presence and relative severity of low back versus leg pain, has been shown to be particularly relevant for treatment and prognostication in DS [54]. These symptoms are thought to be caused by two distinct disease processes requiring different management strategies. Failure to recognize and appropriately address the primary source of a patient’s pain may result in undertreatment and inadequate symptomatic relief or overtreatment and an increased risk of unnecessary complications. Lower extremity pain and radiculopathy, classic symptoms of focal neurologic compression, are typically best addressed with direct decompression of stenotic regions; in the absence of symptomatic deformity or signs of instability, these patients may be less likely to receive an additional benefit from fusion. Therefore, the least invasive and most cost-effective procedure (i.e., decompression alone) would be more appropriate [55, 56]. In contrast, a primary clinical presentation with mechanical low back pain is often considered a sign of underlying instability and stabilization of the painful or pathologic motion segment is thought to be particularly important for providing adequate symptomatic relief. In support of this, several studies have observed suboptimal outcomes after decompression in the absence of fusion in patients with low back pain [55, 57].
Several classifications systems include either leg (CARDS) or back pain (DSIC, Kulkarni), however none account for the relative severity of both, which has been shown to be particularly predictive of functional improvement postoperatively. Outcomes of the Spine Patient Outcomes Research Trial (SPORT) showed that patients presenting with primarily lower extremity symptoms tend to have less severe baseline pain and experience greater improvement after surgery compared to those with primarily low back pain; intermediate outcomes are observed in those with symptoms of equal severity [54].
Inter/intraobserver reliability
Methods
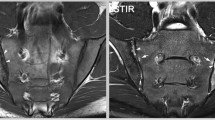
Approval from the institutional Investigational Review Board was received prior to study initiation. Diagnostic imaging and clinical presentations of 10 patients surgically treated for L4/5 DS were used for validation of the UCSF Degenerative Spondylolisthesis Classification. Validation of the classification was done by 12 individuals, including 4 fellowship trained spine faculty, 3 fellows in training, 2 residents, and 3 medical students. There was no significant difference in the accuracy of validation by level of training. Representative images were provided, along with relevant radiographic measurements. For each of the four classification system categories, the reviewers were asked to assign a score of 1, 2, or 3 based on the presented pathology. For example, a patient with 4 mm of dynamic translation, central stenosis without foraminal stenosis, segmental kyphosis with preserved global alignment, VAS for back pain 6/10, and VAS for leg pain 2/10 would be assigned ratings of 2, 1, 2, and 3, respectively. Each reviewer reclassified the ten cases 2 weeks later to assess intraobserver reliability. During this second round, the order of the cases was randomized to minimize recall bias.
Kappa statistics were calculated to determine interobserver and intraobserver reliabilities for each of the four categories within the UCSF DS classification. Calculations were performed using R, Version 4.2.3 (R Foundation, Vienna, Austria). Interobserver reliability for each category was determined by comparing all reviewers’ first round ratings to limit bias from being familiar with the protocol. Intraobserver reliability was calculated by first determining the kappa value for each rater between the first and second rounds and then averaging kappa statistics across all raters [22]. Kappa values were interpreted according to the guidelines established by Landis and Koch (kappa 0–0.20, slight agreement; 0.21–0.40, fair agreement; 0.41–0.60, moderate agreement; 0.61–0.80, substantial agreement; and 0.81–1.00, near perfect agreement) [58].
Results
The 10 cases were comprised of 6 males and 4 females, with average age 64.0 ± 8.5 years. 12 individuals completed evaluations for all 10 cases. The interobserver Fleiss kappa values for the dynamic instability, location of stenosis, sagittal alignment, and clinical presentation were 0.94, 0.80, 0.87, and 1.00, respectively. The intraobserver kappa values for the dynamic instability, location of stenosis, sagittal alignment, and clinical presentation were 0.91, 0.88, 0.87, and 0.97, respectively. The interobserver and intraobserver reliability results are summarized below in Table 4. All kappa values were greater than 0.80, indicting almost perfect interobserver and intraobserver reliability [58].
Discussion
The UCSF DS classification was designed to reflect the fundamental components of surgical decision-making in DS. These subcategories categorize patients into clinically distinct subgroups for which the optimal surgical strategy may differ.
Patients with biomechanically stable DS who are presenting with symptoms of focal neurologic compression in the absence of symptomatic deformity have been successfully treated with decompression alone with low rates of complications or revision surgery [33]. These patients are unlikely to experience clinically significant benefits from a more extensive fusion procedure, and therefore should not be subjected to the additional risk of a larger surgery.
In contrast, spinal fusion will likely confer a clinically significant benefit to patient subgroups with features of instability. Fusion may be indicated to stabilize painful motion segments in patients with mechanical back pain or to prevent deformity progression in cases with gross dynamic instability or in patients for whom a wide, likely destabilizing, decompression may be necessary to adequately address foraminal stenosis.
In the setting of significant dynamic instability, up–down foraminal stenosis, and / or regional or global malalignment, a more extensive procedure may be necessary to address structural deformity [38]. Interbody fusion is an effective strategy for treating discogenic low back pain that can be used to augment biomechanical stability, enhance fusion rates, introduce segmental lordosis, and correct sagittal balance. The indirect decompression afforded by placement of an interbody device is particularly useful in the treatment of patients with alignment deformity or severe disc collapse and resultant up/down foraminal stenosis [59,60,61].
All four categories composing the UCSF DS classification were shown to have almost perfect interobserver and intraobserver reliability when applied to a variety of case examples representative of the spectrum of DS disease pathologies. Moving forward, it will be important to explore the utility of this classification for guiding treatment in patients with DS. Future work will consequently involve validating the clinical significance of proposed classification components and their individual subgroups to determine their relative significance for influencing surgical treatment of DS.
Conclusion
Degenerative spondylolisthesis is among the most common causes of low back pain and disability in older adults. For symptomatic disease, while spinal fusion seems to result in better clinical outcomes in some patients, others experience durable relief from decompression alone. Clinical studies and meta-analyses have reported conflicting outcomes regarding the comparative efficacy of different approaches, which has precluded establishment of standardized evidence-based guidelines for treatment. This is largely a result of the heterogeneous spectrum of clinical and radiographic presentations encompassed in this condition, which are poorly accounted for in current methods of classification. Considering these historical limitations, the UCSF Degenerative Spondylolisthesis Classification System was created to provide a framework for subclassifying patients with DS based on a combination of features with established crucial roles for surgical decision-making. Future work will continue to validate the clinical relevance of this system, with the goal of providing for a more evidence-based, standardized approach to treatment that can optimize outcomes for patients with DS.
Change history
02 November 2023
A Correction to this paper has been published: https://doi.org/10.1007/s00586-023-07994-w
References
Deyo RA, Gray DT, Kreuter W et al (2005) United States trends in lumbar fusion surgery for degenerative conditions. Spine 30:1441–1445. https://doi.org/10.1097/01.brs.0000166503.37969.8a
Wiltse L (1981) Classification, terminology and measurements in spondylolisthesis. Iowa Orthop J 1:52–57
Lee JYB, Patel AA (2013) Lumbar spinal stenosis and degenerative spondylolisthesis. Semin Spine Surg 25:256–262. https://doi.org/10.1053/j.semss.2013.05.006
Kirkaldy-Willis WHMA, Farfan HFMS (1982) Instability of the lumbar spine. Clin Orthop 165:110–123
Sengupta DK, Herkowitz HN (2005) Degenerative spondylolisthesis: review of current trends and controversies. Spine 30:S71-81. https://doi.org/10.1097/01.brs.0000155579.88537.8e
García-Ramos CL, Valenzuela-González J, Baeza-Álvarez VB et al (2020) Degenerative spondylolisthesis I: general principles. Acta Ortop Mex 34:324–328
Weinstein JN, Lurie JD, Tosteson TD et al (2007) Surgical versus nonsurgical treatment for lumbar degenerative spondylolisthesis. N Engl J Med 356:2257–2270. https://doi.org/10.1056/NEJMoa070302
Weinstein JN, Lurie JD, Tosteson TD et al (2009) Surgical compared with nonoperative treatment for lumbar degenerative spondylolisthesis. four-year results in the Spine Patient Outcomes Research Trial (SPORT) randomized and observational cohorts. J Bone Joint Surg Am 91:1295–1304. https://doi.org/10.2106/JBJS.H.00913
Abdu WA, Sacks OA, Tosteson ANA et al (2018) Long-term results of surgery compared with nonoperative treatment for lumbar degenerative spondylolisthesis in the spine patient outcomes research trial (SPORT). Spine 43:1619–1630. https://doi.org/10.1097/BRS.0000000000002682
Matz PG, Meagher RJ, Lamer TJ, Tonz W (2014) Diagnosis and treatment of degenerative lumbar spondylolisthesis, 2nd ed. North American Spine Society
Ghogawala Z, Dziura J, Butler WE et al (2016) Laminectomy plus fusion versus laminectomy alone for lumbar spondylolisthesis. N Engl J Med 374:1424–1434. https://doi.org/10.1056/NEJMoa1508788
Chan AK, Bisson EF, Bydon M et al (2019) A comparison of minimally invasive transforaminal lumbar interbody fusion and decompression alone for degenerative lumbar spondylolisthesis. Neurosurg Focus 46:E13. https://doi.org/10.3171/2019.2.FOCUS18722
Austevoll IM, Gjestad R, Solberg T, et al (2020) Comparative effectiveness of microdecompression alone vs decompression plus instrumented fusion in lumbar degenerative spondylolisthesis. JAMA Netw Open 3:e2015015. https://doi.org/10.1001/jamanetworkopen.2020.15015
Wu J, Zhang J, Xu T, et al (2021) The necessity or not of the addition of fusion to decompression for lumbar degenerative spondylolisthesis patients: a PRISMA compliant meta-analysis. Medicine (Baltimore) 100:e24775. https://doi.org/10.1097/MD.0000000000024775
Lubelski D, Alentado VJ, Williams SK et al (2018) Variability in surgical treatment of spondylolisthesis among spine surgeons. World Neurosurg 111:e564–e572. https://doi.org/10.1016/j.wneu.2017.12.108
Meyerding HW (1932) Spondylolisthesis. Surg Gynecol Obstet 54:371–377
Matsunaga S, Ijiri K, Hayashi K (2000) Nonsurgically managed patients with degenerative spondylolisthesis: a 10- to 18-year follow-up study. J Neurosurg Spine 93:194–198. https://doi.org/10.3171/spi.2000.93.2.0194
Gille O, Bouloussa H, Mazas S et al (2017) A new classification system for degenerative spondylolisthesis of the lumbar spine. Eur Spine J 26:3096–3105. https://doi.org/10.1007/s00586-017-5275-4
Gille O, Challier V, Parent H et al (2014) Degenerative lumbar spondylolisthesis: cohort of 670 patients, and proposal of a new classification. Orthop Traumatol Surg Res 100:S311–S315. https://doi.org/10.1016/j.otsr.2014.07.006
Schwab F, Ungar B, Blondel B et al (2012) Scoliosis Research Society-Schwab adult spinal deformity classification: a validation study. Spine 37:1077–1082. https://doi.org/10.1097/BRS.0b013e31823e15e2
Kong C, Sun X, Ding J et al (2019) Comparison of the French and CARDS classifications for lumbar degenerative spondylolisthesis: reliability and validity. BMC Musculoskelet Disord 20:382. https://doi.org/10.1186/s12891-019-2753-3
Kepler CK, Hilibrand AS, Sayadipour A et al (2015) Clinical and radiographic degenerative spondylolisthesis (CARDS) classification. Spine J 15:1804–1811. https://doi.org/10.1016/j.spinee.2014.03.045
Sobol GL, Hilibrand A, Davis A et al (2018) Reliability and clinical utility of the CARDS classification for degenerative spondylolisthesis. Clin Spine Surg Spine Publ 31:E69–E73. https://doi.org/10.1097/BSD.0000000000000571
Hammerberg KW (2005) New concepts on the pathogenesis and classification of spondylolisthesis. Spine 30:S4–S11. https://doi.org/10.1097/01.brs.0000155576.62159.1c
Simmonds AM, Rampersaud YR, Dvorak MF et al (2015) Defining the inherent stability of degenerative spondylolisthesis: a systematic review. J Neurosurg Spine 23:178–189. https://doi.org/10.3171/2014.11.SPINE1426
Kobayashi H, Endo K, Sawaji Y et al (2019) Global sagittal spinal alignment in patients with degenerative low-grade lumbar spondylolisthesis. J Orthop Surg 27:230949901988519. https://doi.org/10.1177/2309499019885190
Kulkarni AG, Sagane SS, Kunder TS (2020) Management of spondylolisthesis using MIS techniques: recent advances. J Clin Orthop Trauma 11:839–847. https://doi.org/10.1016/j.jcot.2020.07.015
Kulkarni AG, Kunder TS, Dutta S (2020) Degenerative spondylolisthesis: when to fuse and when not to? a new scoring system. Clin Spine Surg 33:E391–E400. https://doi.org/10.1097/BSD.0000000000000970
Ha K-Y, Na K-H, Shin J-H, Kim K-W (2008) Comparison of posterolateral fusion with and without additional posterior lumbar interbody fusion for degenerative lumbar spondylolisthesis. J Spinal Disord Tech 21:229–234. https://doi.org/10.1097/BSD.0b013e3180eaa202
Reis RC, de Oliveira MF, Rotta JM, Botelho RV (2015) Risk of complications in spine surgery: a prospective study. Open Orthop J 9:20–25. https://doi.org/10.2174/1874325001509010020
Kepler CK, Vaccaro AR, Hilibrand AS et al (2014) National trends in the use of fusion techniques to treat degenerative spondylolisthesis. Spine 39:1584–1589. https://doi.org/10.1097/BRS.0000000000000486
Satomi K, Hirabayashi K, Toyama Y, Fujimura Y (1992) A clinical study of degenerative spondylolisthesis: radiographic analysis and choice of treatment. Spine 17:1329–1336
Kelleher MO, Timlin M, Persaud O, Rampersaud YR (2010) Success and failure of minimally invasive decompression for focal lumbar spinal stenosis in patients with and without deformity. Spine 35:E981–E987. https://doi.org/10.1097/BRS.0b013e3181c46fb4
Inui T, Murakami M, Nagao N et al (2017) Lumbar degenerative spondylolisthesis: changes in surgical indications and comparison of instrumented fusion with two surgical decompression procedures. Spine 42:E15–E24. https://doi.org/10.1097/BRS.0000000000001688
Ilyas H, Udo-Inyang I, Savage J (2019) Lumbar spinal stenosis and degenerative spondylolisthesis: a review of the SPORT literature. Clin Spine Surg 32:272–278. https://doi.org/10.1097/BSD.0000000000000841
Zeng Z-L, Zhu R, Wu Y-C et al (2017) Effect of graded facetectomy on lumbar biomechanics. J Healthc Eng 2017:7981513. https://doi.org/10.1155/2017/7981513
Sharif S, Shaikh Y, Bajamal AH, et al (2020) Fusion surgery for lumbar spinal stenosis: WFNS spine committee recommendations. World Neurosurg X 7:100077. https://doi.org/10.1016/j.wnsx.2020.100077
Choi YK (2019) Lumbar foraminal neuropathy: an update on non-surgical management. Korean J Pain 32:147–159. https://doi.org/10.3344/kjp.2019.32.3.147
Hasegawa T, An HS, Haughton VM, Nowicki BH (1995) Lumbar foraminal stenosis: critical heights of the intervertebral discs and foramina: a cryomicrotome study in cadavera. J Bone Joint Surg Am 77:32–38
Lee S, Lee JW, Yeom JS et al (2010) A practical MRI grading system for lumbar foraminal stenosis. Am J Roentgenol 194:1095–1098. https://doi.org/10.2214/AJR.09.2772
Oliveira L, Marchi L, Coutinho E, Pimenta L (2010) A radiographic assessment of the ability of the extreme lateral interbody fusion procedure to indirectly decompress the neural elements. Spine 35:S331-337. https://doi.org/10.1097/BRS.0b013e3182022db0
Park D, Mummaneni PV, Mehra R, et al (2020) Predictors of the need for laminectomy after indirect decompression via initial anterior or lateral lumbar interbody fusion. J Neurosurg Spine 1–7. https://doi.org/10.3171/2019.11.SPINE19314
Isaacs RE, Sembrano JN, Tohmeh AG, SOLAS Degenerative Study Group (2016) Two-year comparative outcomes of MIS lateral and MIS transforaminal interbody fusion in the treatment of degenerative spondylolisthesis: Part II: radiographic findings. Spine 41 Suppl 8:S133-144. https://doi.org/10.1097/BRS.0000000000001472
Sembrano JN, Tohmeh A, Isaacs R, SOLAS Degenerative Study Group (2016) Two-year comparative outcomes of MIS lateral and MIS transforaminal interbody fusion in the treatment of degenerative spondylolisthesis: part I: clinical findings. Spine 41 Suppl 8:S123-132. https://doi.org/10.1097/BRS.0000000000001471
Orita S, Inage K, Eguchi Y et al (2016) Lumbar foraminal stenosis, the hidden stenosis including at L5/S1. Eur J Orthop Surg Traumatol Orthop Traumatol 26:685–693. https://doi.org/10.1007/s00590-016-1806-7
Phillips FM, Slosar PJ, Youssef JA et al (2013) Lumbar spine fusion for chronic low back pain due to degenerative disc disease: a systematic review. Spine 38:E409–E422. https://doi.org/10.1097/BRS.0b013e3182877f11
Barrey C, Roussouly P, Le Huec J-C et al (2013) Compensatory mechanisms contributing to keep the sagittal balance of the spine. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 22(Suppl 6):S834-841. https://doi.org/10.1007/s00586-013-3030-z
Glassman SD, Bridwell K, Dimar JR et al (2005) The impact of positive sagittal balance in adult spinal deformity. Spine 30:2024–2029. https://doi.org/10.1097/01.brs.0000179086.30449.96
Lafage V, Schwab F, Patel A et al (2009) Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine 34:E599–E606. https://doi.org/10.1097/BRS.0b013e3181aad219
Schwab F, Patel A, Ungar B et al (2010) Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine 35:2224–2231. https://doi.org/10.1097/BRS.0b013e3181ee6bd4
Radovanovic I, Urquhart JC, Ganapathy V et al (2017) Influence of postoperative sagittal balance and spinopelvic parameters on the outcome of patients surgically treated for degenerative lumbar spondylolisthesis. J Neurosurg Spine 26:448–453. https://doi.org/10.3171/2016.9.SPINE1680
He S, Zhang Y, Ji W et al (2020) Analysis of spinopelvic sagittal balance and persistent low back pain (PLBP) for degenerative spondylolisthesis (DS) following posterior lumbar interbody fusion (PLIF). Pain Res Manag 2020:5971937. https://doi.org/10.1155/2020/5971937
Butt S, Saifuddin A (2005) The imaging of lumbar spondylolisthesis. Clin Radiol 60:533–546. https://doi.org/10.1016/j.crad.2004.07.013
Pearson A, Blood E, Lurie J et al (2011) Predominant leg pain is associated with better surgical outcomes in degenerative spondylolisthesis and spinal stenosis: results from the spine patient outcomes research trial (SPORT). Spine 36:219–229. https://doi.org/10.1097/BRS.0b013e3181d77c21
Dijkerman ML, Overdevest GM, Moojen WA, Vleggeert-Lankamp CLA (2018) Decompression with or without concomitant fusion in lumbar stenosis due to degenerative spondylolisthesis: a systematic review. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 27:1629–1643. https://doi.org/10.1007/s00586-017-5436-5
Koenig S, Jauregui JJ, Shasti M et al (2019) Decompression versus fusion for grade I degenerative spondylolisthesis: a meta-analysis. Glob Spine J 9:155–161. https://doi.org/10.1177/2192568218777476
Joaquim AF, Milano JB, Ghizoni E, Patel AA (2016) Is there a role for decompression alone for treating symptomatic degenerative lumbar spondylolisthesis?: a systematic review. Clin Spine Surg 29:191–202. https://doi.org/10.1097/BSD.0000000000000357
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Kim SJ, Lee YS, Kim YB, et al (2014) Clinical and radiological outcomes of a new cage for direct lateral lumbar interbody fusion. Korean J Spine 11:145–151. https://doi.org/10.14245/kjs.2014.11.3.145
Rao PJ, Maharaj MM, Phan K et al (2015) Indirect foraminal decompression after anterior lumbar interbody fusion: a prospective radiographic study using a new pedicle-to-pedicle technique. Spine J Off J North Am Spine Soc 15:817–824. https://doi.org/10.1016/j.spinee.2014.12.019
Walker CT, Xu DS, Cole TS, et al (2021) Predictors of indirect neural decompression in minimally invasive transpsoas lateral lumbar interbody fusion. J Neurosurg Spine 1–11. https://doi.org/10.3171/2020.8.SPINE20676
Funding
No funding was received to assist with the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rangwalla, K., Filley, A., El Naga, A. et al. Degenerative lumbar spondylolisthesis: review of current classifications and proposal of a novel classification system. Eur Spine J 33, 1762–1772 (2024). https://doi.org/10.1007/s00586-023-07818-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07818-x