Abstract
Purpose
Current decision-making in multilevel cervical fusion weighs the potential to protect adjacent levels and reduce reoperation risk by crossing the cervicothoracic junction (C7/T1) against increased operative time and risk of complication. Careful planning is required, and the planned distal and adjacent levels should be assessed for degenerative disc disease (DDD). This study assessed whether DDD at the cervicothoracic junction was associated with DDD, disc height, translational motion, or angular variation in the adjacent superior (C6/C7) or inferior (T1/T2) levels.
Methods
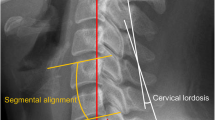
This study retrospectively analyzed 93 cases with kinematic MRI. Cases were randomly selected from a database with inclusion criteria being no prior spine surgery and images having sufficient quality for analysis. DDD was assessed using Pfirrmann classification. Vertebral body bone marrow lesions were assessed using Modic changes. Disc height was measured at the mid-disc in neutral and extension. Translational motion and angular variation were calculated by assessing translational or angular motion segment integrity respectively in flexion and extension. Statistical associations were assessed with scatterplots and Kendall’s tau.
Results
DDD at C7/T1 was positively associated with DDD at C6/C7 (tau = 0.53, p < 0.01) and T1/T2 (tau = 0.58, p < 0.01), with greater disc height in neutral position at T1/T2 (tau = 0.22, p < 0.01), and with greater disc height in extended position at C7/T1 (tau = 0.17, p = 0.04) and at T1/T2 (tau = 0.21, p < 0.01). DDD at C7/T1 was negatively associated with angular variation at C6/C7 (tau = − 0.23, p < 0.01). No association was appreciated between DDD at C7/T1 and translational motion.
Conclusion
The association of DDD at the cervicothoracic junction with DDD at the adjacent levels emphasizes the necessity for careful selection of the distal level in multilevel fusion in the distal cervical spine.




Similar content being viewed by others
References
Salzmann SN, Derman PB, Lampe LP, Kueper J, Pan TJ, Yang J, Shue J, Girardi FP, Lyman S, Hughes AP (2018) Cervical spinal fusion: 16-year trends in epidemiology, indications, and in-hospital outcomes by surgical approach. World Neurosurg 113:e280–e295. https://doi.org/10.1016/j.wneu.2018.02.004
Ibaseta A, Rahman R, Andrade NS, Uzosike AC, Byrapogu VK, Ramji AF, Skolasky RL, Reidler JS, Kebaish KM, Riley LH, Sciubba DM, Cohen DB, Neuman BJ (2019) Crossing the cervicothoracic junction in cervical arthrodesis results in lower rates of adjacent segment disease without affecting operative risks or patient-reported outcomes. Clin Spine Surg 32:377–381. https://doi.org/10.1097/BSD.0000000000000897
Cheng I, Sundberg EB, Iezza A, Lindsey DP, Riew KD (2015) Biomechanical determination of distal level for fusions across the cervicothoracic junction. Global Spine J 5:282–286. https://doi.org/10.1055/s-0035-1546418
Osterhoff G, Ryang Y-M, von Oelhafen J, Meyer B, Ringel F (2017) Posterior multilevel instrumentation of the lower cervical spine: is bridging the cervicothoracic junction necessary? World Neurosurg 103:419–423. https://doi.org/10.1016/j.wneu.2017.04.029
Chang MC, Kim G-U, Choo YJ, Lee GW (2022) To cross or not to cross the cervicothoracic junction in multilevel posterior cervical fusion: a systematic review and meta-analysis. Spine J 22:723–731. https://doi.org/10.1016/j.spinee.2022.01.001
Toci GR, Karamian BA, Lambrechts MJ, Mao J, Mandel J, Darrach T, Canseco JA, Kaye ID, Woods BI, Rihn J, Kurd MF, Hilibrand AS, Kepler CK, Vaccaro AR, Schroeder GD (2022) Instrumentation across the cervicothoracic junction does not improve patient-reported outcomes in multilevel posterior cervical decompression and fusion. Clinical Spine Surgery. https://doi.org/10.1097/BSD.0000000000001335
Rajjoub R, Michalopoulos GD, El Sammak S, Goyal A, Alexander AY, Wahood W, Freedman BA, Sebastian A, Bydon M (2022) Crossing the cervicothoracic junction in multilevel cervical arthrodesis: a systematic review and meta-analysis. World neurosurgery 162:e336–e346. https://doi.org/10.1016/j.wneu.2022.03.013
Coban D, Faloon M, Changoor S, Saela S, Sahai N, Record N, Sinha K, Hwang K, Emami A (2022) Should we bridge the cervicothoracic junction in long cervical fusions? A meta-analysis and systematic review of the literature. J Neurosurg Spine. https://doi.org/10.3171/2021.12.SPINE211090
Fayed I, Toscano DT, Triano MJ, Makariou E, Lee C, Spitz SM, Anaizi AN, Nair MN, Sandhu FA, Voyadzis JM (2020) Crossing the cervicothoracic junction during posterior cervical decompression and fusion: is it necessary? Neurosurgery 86:E544–E550. https://doi.org/10.1093/neuros/nyaa078
Chan AK, Badiee RK, Rivera J, Chang C-C, Robinson LC, Mehra RN, Tan LA, Clark AJ, Dhall SS, Chou D, Mummaneni PV (2020) Crossing the cervicothoracic junction during posterior cervical fusion for myelopathy is associated with superior radiographic parameters but similar clinical outcomes. Neurosurgery 87:1016–1024. https://doi.org/10.1093/neuros/nyaa241
Guppy KH, Royse KE, Fennessy JH, Norheim EP, Harris JE, Brara HS (2021) No difference in reoperation rates for nonunions (operative nonunions) in posterior cervical fusions stopping at C7 versus T1/2: a cohort of 875 patients. J Neurosurg Spine 36:1–985. https://doi.org/10.3171/2021.10.SPINE211085
Lee D-H, Cho JH, Jung JI, Baik J-M, Jun DS, Hwang CJ, Lee CS (2019) Does stopping at C7 in long posterior cervical fusion accelerate the symptomatic breakdown of cervicothoracic junction? PLoS ONE 14:e0217792–e0217792. https://doi.org/10.1371/journal.pone.0217792
Rajjoub R, Michalopoulos GD, El Sammak S, Goyal A, Alexander AY, Wahood W, Freedman BA, Sebastian A, Bydon M (2022) Crossing the cervicothoracic junction in multilevel cervical arthrodesis: a systematic review and meta-analysis. World Neurosurg. https://doi.org/10.1016/j.wneu.2022.03.013
Louie PK, Presciutti SM, Iantorno SE, Bohl DD, Shah K, Shifflett GD, An HS (2017) There is no increased risk of adjacent segment disease at the cervicothoracic junction following an anterior cervical discectomy and fusion to C7. Spine J 17:1264–1271. https://doi.org/10.1016/j.spinee.2017.04.027
Truumees E, Singh D, Geck MJ, Stokes JK (2018) Should long-segment cervical fusions be routinely carried into the thoracic spine? A multicenter analysis. Spine J 18:782–787. https://doi.org/10.1016/j.spinee.2017.09.010
Toci GR, Karamian BA, Lambrechts MJ, Mao J, Mandel J, Darrach T, Canseco JA, Kaye ID, Woods BI, Rihn J, Kurd MF, Hilibrand AS, Kepler CK, Vaccaro AR, Schroeder GD (2022) Instrumentation across the cervicothoracic junction does not improve patient-reported outcomes in multilevel posterior cervical decompression and fusion. Clin Spine Surg. https://doi.org/10.1097/bsd.0000000000001335
Guppy KH, Royse KE, Fennessy JH, Norheim EP, Harris JE, Brara HS (2021) No difference in reoperation rates for nonunions (operative nonunions) in posterior cervical fusions stopping at C7 versus T1/2: a cohort of 875 patients. J Neurosurg Spine. https://doi.org/10.3171/2021.10.Spine211085
Son S, Lee SG, Kim WK, Ahn Y, Jung JM (2021) Disc height discrepancy between supine and standing positions as a screening metric for discogenic back pain in patients with disc degeneration. Spine J 21:71–79. https://doi.org/10.1016/j.spinee.2020.07.006
Cannata F, Vadalà G, Ambrosio L, Fallucca S, Napoli N, Papalia R, Pozzilli P, Denaro V (2020) Intervertebral disc degeneration: a focus on obesity and type 2 diabetes. Diabetes Metab Res Rev 36:e3224. https://doi.org/10.1002/dmrr.3224
Kirnaz S, Capadona C, Wong T, Goldberg JL, Medary B, Sommer F, McGrath LB Jr, Härtl R (2022) Fundamentals of Intervertebral Disc Degeneration. World Neurosurg 157:264–273. https://doi.org/10.1016/j.wneu.2021.09.066
Tu TH, Wang CY, Chen YC, Wu JC (2023) Multilevel cervical disc arthroplasty: a review of optimal surgical management and future directions. J Neurosurg Spine 38:372–381. https://doi.org/10.3171/2022.11.Spine22880
Safaee MM, Lin J, Smith DL, Fury M, Scheer JK, Burke JF, Bravate C, Lambert D, Ames CP (2023) Association of telomere length with risk of complications in adult spinal deformity surgery: a pilot study of 43 patients. J Neurosurg Spine 38:331–339. https://doi.org/10.3171/2022.10.Spine22605
Battié MC, Videman T, Kaprio J, Gibbons LE, Gill K, Manninen H, Saarela J, Peltonen L (2009) The Twin Spine Study: contributions to a changing view of disc degeneration. Spine J 9:47–59. https://doi.org/10.1016/j.spinee.2008.11.011
Battié MC, Videman T, Levälahti E, Gill K, Kaprio J (2008) Genetic and environmental effects on disc degeneration by phenotype and spinal level: a multivariate twin study. Spine (Phila Pa 1976) 33:2801–2808. doi: https://doi.org/10.1097/BRS.0b013e31818043b7
Hancock MJ, Battie MC, Videman T, Gibbons L (2010) The role of back injury or trauma in lumbar disc degeneration: an exposure-discordant twin study. Spine (Phila Pa 1976) 35:1925–1929. https://doi.org/10.1097/BRS.0b013e3181d60598
Näkki A, Battié MC, Kaprio J (2014) Genetics of disc-related disorders: current findings and lessons from other complex diseases. Eur Spine J 23(Suppl 3):S354-363. https://doi.org/10.1007/s00586-013-2878-2
Acknowledgements
The authors make no declarations.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The authors declare no conflict of interests. The authors did not receive support from any organization for the submitted work. The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kim, M.S., Gilbert, Z.D., Bajouri, Z. et al. What does degeneration at the cervicothoracic junction tell us? A kinematic MRI study of 93 individuals. Eur Spine J 32, 2425–2430 (2023). https://doi.org/10.1007/s00586-023-07743-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07743-z