Abstract
Purposes
An optimal pedicle screw density for spinal deformity correction in adolescent idiopathic scoliosis (AIS) remains poorly defined. We compared radiographic correction, operative time, estimated blood loss, and implant cost among different screw density patterns in operatively treated AIS patients.
Methods
A retrospective observational cohort study of AIS patients who underwent posterior spinal fusion using all-pedicle screw instrumentation was conducted from January 2012 to December 2018. All patients were categorized into three different pedicle screw density groups: the very low density (VLD), the low density (LD), and the high density (HD) group. The comparative effectiveness between each pairwise comparison was performed under the inverse probability of the treatment weighting method to minimize the possible confounders imbalance among treatment groups. The primary endpoints in this study were the degrees of correction and deformity progression at 2 years postoperatively.
Results
A total of 174 AIS patients were included in this study. The adjusted treatment effects demonstrated similar degrees of deformity correction after 2 years in the three treatment groups. However, the VLD and LD group slightly increased the curve progression at 2 years compared to the HD group by 3.9° (p = 0.005) and 3.2° (p = 0.044), respectively. Nevertheless, the limited screw density patterns (VLD and LD) significantly reduced the operative time, estimated blood loss, and implant cost per operated level.
Conclusion
The limited pedicle screw pattern (VLD and LD) in relatively flexible AIS spinal deformity correction results in similar coronal and sagittal radiological outcomes while reducing operative time, estimated blood loss, and implant cost compared to the high-density pedicle screw instrumentation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adolescent idiopathic scoliosis (AIS) is a three-dimensional spinal deformity found in children between 10 and 18 years old [1]. Regardless of the terminology, current literature has identified several possible etiologies of AIS, such as genetic polymorphisms, physiological disruptions, and environmental triggers [2]. The diagnosis of AIS is made when Cobb’s angle is greater than 10° [3]. Operative treatment is generally indicated when Cobb’s angle reaches 50°.
Currently, pedicle screw instrumentation is considered the standard operative treatment for AIS spinal deformity correction [4, 5]. This fixation construct provides a greater correction degree than hook and hybrid constructs. Previous studies demonstrated additional benefits of the pedicle screw system, including greater pullout strength [6], lower long-term deformity progression rates, lower implant failure rates, and lower pseudarthrosis [7]. An optimal number of pedicle screw applications within the structural curve remains controversial. The definition of low- and high-density pedicle screw fixation remains poorly defined [8]. Although maximizing the number of screw instrumentation theoretically benefits the fixation stability [9], several studies reported no significant association between the screw density and the radiographic outcome [8, 10, 11]. However, relevant evidence was reported based on unadjusted results from observational data, which could alter the accurate effect estimates of the different pedicle screw densities [8].
This study aimed to compare the treatment effects of different screw density patterns on AIS patients’ two-year radiographic outcomes. In addition, we also examined the association between screw density and operative time, estimated blood loss, and implant cost. All analyses were adjusted by potential confounding factors to identify the actual effect estimates of the different screw density patterns.
Materials and methods
Study design
We conducted a retrospective study of AIS patients who received an operative deformity correction at a tertiary care, university-affiliated hospital from January 2012 to December 2018. The study was conducted and reported according to the STROBE statement. The Institutional Review Board has approved the study protocol.
Study patients
We included AIS patients who underwent an operative deformity correction using all-pedicle-screws constructs and posterior spinal fusion during the study period. All included patients receive at least 2 years of regular radiographic studies follow-up. Patients diagnosed with concomitant congenital or neuromuscular spinal involvement, previous spine surgery, and other than a posterior surgical approach were excluded.
Data collection
Patient demographic data, including sex and age, were retrieved from electronic medical records. Preoperative standing radiographic studies of the entire spine were reviewed to determine patients’ initial spinal deformity. Accordingly, we recorded patients’ initial major curve Cobb’s angle, thoracic kyphotic angle, lumbar lordotic angle, and type of spinal deformity classified using Lenke classification [12]. In addition, the traction radiographic studies of the entire spine were reviewed to assess the flexibility of the initial deformity.
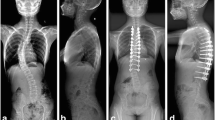
Operative parameters were recorded, including the number of operated vertebrae, applied pedicle screws, and spinal fusion levels. The implant density was defined as the number of fixation screws divided by the number of available anchor sites within the structural curve. Correspondingly, patients were categorized into three groups with different screw densities, high density (HD), low density (LD), and very low density (VLD) (Fig. 1). HD was defined as a screw density of ≥ 1.4, while LD was described as a screw density of 1.1–1.4. Although the definition of HD and LD varied among literature, most used a cutoff value between 1.3 and 1.6. Therefore, we used the value of 1.4 to classify HD and LD in this study. In addition, we defined VLD as a screw density of < 1.1, representing a skipped pedicle screw pattern.
Postoperative spinal parameters, including major curve Cobb’s angle, thoracic kyphosis, lumbar lordosis, shoulder height, lower instrumented vertebra (LIV) tilt, and lower instrumented vertebra-central sacral vertebral line (LIV-CSVL) distance, were recorded using a standing radiographic study of the entire spine 1 month and 2 years postoperatively. Furthermore, associated information such as operative time, estimated blood loss, length of hospital stays, and implant cost was retrieved for evaluation.
Statistical analysis
Fundamental statistical analysis
The data distribution pattern was examined using a histogram and the Shapiro–Wilk test. Normally distributed continuous data were presented as the Mean ± SD. Non-normally distributed data were presented with median and interquartile range (IQR). One-way analysis of variance ANOVA and the Kruskal–Wallis test were utilized to compare data among three different screw density groups regarding their distribution. Bonferroni correction was deployed to examine the difference between the two groups. Categorical data were tested using Fisher’s exact probability test. All statistical analyses were performed using STATA version 16 (StataCorp, Lakeway, TX). Statistical significance was set at a p-value less than 0.05.
Inverse probability of treatments weighting
The non-randomized study design is subjected to several biases. Hence, the univariable analysis cannot determine the treatment effects since the results are probably confounded by several factors [13]. One of the essential biases is the selection bias regarding indications and contraindications of each assigned treatment [14]. Therefore, we applied inverse probability of treatment weighting (IPTW) to balance the probability of receiving different treatments for each patient [15]. IPTW is a propensity score method that considers the probability of receiving treatments regarding confounding factors. Subsequently, the IPTW approach will weigh the treatment effects according to the propensity of receiving each treatment. The standardized difference (STD) of confounding factors was used to determine the difference between treatment groups after weighting. An absolute STD of more than 10% is considered a significant difference among treatment arms [16]. In this study, the IPTW was calculated based on potential confounding factors, including patients’ age, sex, the number of fusion levels, Lenke type, initial major curve, initial kyphotic curve, and flexibility [17] via multinomial logistic regression analysis. Subsequently, VLD, LD, and HD treatment effects were analyzed under calculated IPTW.
Primary endpoints
We determined treatment effects using the mean difference between the postoperative radiographic value (major curve, thoracic kyphosis, and lumbar lordosis) at 2 years and the initial deformity. In addition, the deformity progression was determined using the mean difference of the postoperative radiographic value between 2 years and 1 month. The mean shoulder height, LIV tilt, and LIV-CSVL distance were compared at 1 month and 2 years postoperatively. The adjusted mean difference of treatment effects between each pairwise comparison was reported. As a result, three pairwise comparisons (VLD vs. HD, LD vs. HD, and VLD vs. LD) were calculated under IPTW for each outcome of interest.
Secondary endpoints
Secondary endpoints include the difference in operative time, operative time per level, estimated blood loss, estimated blood loss per level, length of hospital stays, and implant cost per level between treatment arms. All endpoints were calculated in the same approach as the primary endpoints.
Results
A total of 174 AIS patients were included in this study. Of those, 144 were female, and 30 were male. Patients were categorized into three treatment groups according to screw density. As a result, 52 patients were categorized in the VLD group, 46 in the LD group, and 76 in the HD group. Patients’ baseline characteristics after categorization are demonstrated in Table 1. Patients in HD were significantly older in the HD group compared to the VLD group. In addition, the number of fusion levels and applied pedicular screws quantity were different among the three treatment groups. The postoperative protocol was not different among the three treatment groups. All patients were allowed to attend outdoor activities as tolerated without external orthosis.
Univariable analyses were performed to demonstrate the unadjusted treatment effects of each screw density group (Table 2). There were no statistically significant differences in primary endpoints among the three treatment groups. Only a slight difference was detected in the one-month postoperative major curve Cobb’s angle. The operative time and estimated blood loss per vertebral level were significantly decreased in the VLD and LD group compared to the HD group. Furthermore, the implant cost was significantly lower in the VLD group than in the LD and HD groups.
After applying the IPTW to the analysis, the treatment effects of all treatment groups were adjusted by the possible confounding factors (patients’ age, sex, the number of fusion levels, Lenke type, initial major curve, initial kyphotic curve, and flexibility). Figure 2 illustrates weighted and unweighted absolute STD of confounding factors between each pairwise comparison. The main results were demonstrated using the mean difference of the treatment effects between each pairwise comparison among the three treatment groups (Table 3). There was no statistical difference in postoperative Cobb’s angle reduction at 2 years among the three treatment groups. However, the HD pedicle screw fixation significantly reduced the postoperative Cobb’s angle at 2 years for 3.9° (95% CI 1.2°–6.6°, p-value = 0.005) and 3.2° (95% CI 0.1°–6.3°, p-value = 0.044) compared with the VLD and LD, respectively. Patients with a high screw density demonstrated significant LIV tilt difference compared to low screw density at one month ( − 1.7°, 95% CI − 3.0° to − 0.3°, p = 0.017) and two years ( − 1.4°, 95% CI − 2.7° to − 0.1°, p = 0.039).
Compared to the HD group, the VLD group significantly decreased the operative time per vertebral level by 7.6 min (95% CI − 12.1 to 3.1, p-value < 0.001), decreased both estimated blood loss ( − 251.3 ml, 95% CI − 437.5 to − 65.1, p-value = 0.008) and estimated blood loss per vertebral level ( − 33.5 ml, 95% CI − 49.5 to − 17.4, p-value < 0.001), and lowered the implant cost per vertebral level by 1200 USD (95% CI − 1300 to − 1000, p-value < 0.001). Likewise, the LD group significantly reduced the operative time ( − 57.2 min, 95% CI − 107.8 to − 6.6, p-value = 0.027), the operative time per vertebral level ( − 5.9 min, 95% CI − 10.7 to − 1.2, p-value = 0.014), the estimated blood loss per vertebral level ( − 20.4 ml, 95% CI − 37.5 to − 3.3, p-value = 0.020), and implant cost per level ( − 700 USD, 95% CI − 800 to − 500, p-value < 0.001), compared with the HD group. For the LD verses VLD group analysis, only a 500 USD increment of implant cost per vertebral level was detected (95% CI 300–700, p-value < 0.001).
Discussion
The study results provided adjusted treatment effects of the different pedicle screw densities in AIS spinal deformity correction. While maintaining the ability to correct the coronal and sagittal spinal deformity, VLD and LD successfully reduced the operative time, estimated blood loss, and implant cost per vertebral level compared to HD pedicle screw fixation. Although Cobb’s angle two years progression was significantly higher in VLD and LD groups, the amount of the progression was clinically insignificant [3, 18]. No difference in shoulder height and LIV-CSVL distance were observed among the three groups. Only slight LIV tilt differences were observed among VLD and HD groups.
Pedicle screw instrumentation has become popular in the AIS deformity correction [9]. This fixation method provides three-dimensional biomechanical superiority compared with a hook or hybrid constructs [19]. Theoretically, the stability of the instrumentation construct should be positively correlated to the number of the applied screw, resulting in a better spinal deformity correction [10]. However, several studies reported no correlation between the screw density and the correction ability of the instrumentation [8, 20]. Although no statistical radiographic difference between LD and HD was detected, most studies were observational studies [8, 10, 11]. Accordingly, unadjusted results (without considering potential effect modifiers) reported in previous studies might not reflect the true effect estimates of the different screw density techniques [13].
The optimal number of screw densities remains undefined. Previous studies described a number ranging from 1.2 to 1.6 screws per vertebral level for dichotomizing between low- and high-density screw patterns [8]. Nonetheless, we have observed several cases with screw density as low as 0.8–1.1 that successfully produced an effective radiographic outcome. Therefore, we categorized this particular screw pattern as the very low-density group to provide a more elaborate analysis. After adjusting for potential confounders, our studies also demonstrated similar Cobb’s angle correction ability in accordance with previous studies [8, 10, 11]. Although a slightly increased postoperative deformity progression was shown in the VLD and LD group compared to the HD group, the magnitude of Cobb’s angle increment did not reach the level of clinical significance. An intra- and interobserver variability of Cobb’s angle measurement method was reported at approximately 3°–5° [3]. Furthermore, an increase in Cobb’s angle magnitude of below 5° was not associated with the curve progression [18]. The study found that screw density did not affect postoperative shoulder height and LIV-CSVL distance. Although a statistically significant difference was observed in postoperative LIV tilt between VLD and HD groups, the difference’s magnitude is small and might not affect patients’ clinical outcomes.
Limiting the number of screw instrumentation significantly reduced operative time and estimated blood loss, either in total or per operated vertebral level. A shorter operative time is associated with lower perioperative complications and improved resource utilization [21]. An estimated blood loss is related to the blood transfusion rate, increasing the risk of surgical site infection [22]. As a result, we can imply that the limited screw density would benefit patients’ perioperative safety without deteriorating the radiographic outcome of AIS spinal deformity correction. Implant cost negatively correlated with the screw density. The VLD and LD group significantly reduced the implant cost per operated vertebral level compared to the HD group. In addition, the VLD group demonstrated similar primary endpoints to the LD group with a significant implant cost reduction.
Our study had several strengths. The sample size in this study is relatively large. The results could be applied to most AIS patients since we included all Lenke types in this study. Moreover, we have categorized the screw density into three groups, which provided a more detailed study result. However, due to some limitations, the study results should be interpreted with caution. First, the retrospective observational nature of the study is associated with several biases. Although the IPTW adjustment was deployed, some confounder imbalances persist among treatment groups. Second, some potential confounders, such as Risser grading, bone mineral density, and height velocity [23], were unavailable for adjustment. Third, although implant cost significantly correlates with the screw density, a cost-utility analysis should be performed to identify the economic benefits among different screw density groups [24]. Fourth, this study did not evaluate the patient-reported outcome assessment (e.g., SRS-22 questionnaire) could provide helpful clinical correlations of the intervention. Fifth, postoperative three-dimensional imaging (computer tomography) was not available. Therefore, the study results could not provide postoperative spinal rotational alignment. Finally, the heterogeneity of surgical techniques (i.e., degrees of soft-tissue release, different assisted methods for pedicle screw insertion, and spinal osteotomy) might affect the radiographic outcome [25].
Conclusion
The very low and the low-density pedicle screw instrumentation demonstrated similar coronal and sagittal radiographic outcomes compared to the high-density pedicle screw fixation in relatively flexible spinal deformity. Since no 3D analysis nor patient-reported outcomes were performed and thus the effects of apical derotation possible with pedicle screw constructs were unable to be assessed on these three treatment groups. Nevertheless, these limited pedicle screw fixation constructs improve perioperative safety by reducing operative time and estimated blood loss.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request. The data are not publicly available due to their containing information that could compromise the privacy of research participants.
Code availability
Not applicable.
References
Weinstein SL, Dolan LA, Cheng JC, Danielsson A, Morcuende JA (2008) Adolescent idiopathic scoliosis. Lancet 371:1527–1537. https://doi.org/10.1016/s0140-6736(08)60658-3
Kikanloo SR, Tarpada SP, Cho W (2019) Etiology of adolescent idiopathic scoliosis: a literature review. Asian Spine J 13:519–526. https://doi.org/10.31616/asj.2018.0096
Wang J, Zhang J, Xu R, Chen TG, Zhou KS, Zhang HH (2018) Measurement of scoliosis Cobb angle by end vertebra tilt angle method. J Orthop Surg Res 13:223. https://doi.org/10.1186/s13018-018-0928-5
Xu R, Ebraheim NA, Ou Y, Yeasting RA (1998) Anatomic considerations of pedicle screw placement in the thoracic spine Roy-Camille technique versus open-lamina technique. Spine 23:1065–1068. https://doi.org/10.1097/00007632-199805010-00021
Vaccaro AR, Rizzolo SJ, Balderston RA, Allardyce TJ, Garfin SR, Dolinskas C, An HS (1995) Placement of pedicle screws in the thoracic spine. Part II: an anatomical and radiographic assessment. J Bone Joint Surg Am 77:1200–1206. https://doi.org/10.2106/00004623-199508000-00009
Liljenqvist U, Hackenberg L, Link T, Halm H (2001) Pullout strength of pedicle screws versus pedicle and laminar hooks in the thoracic spine. Acta Orthop Belg 67:157–163
Kuklo TR, Potter BK, Lenke LG, Polly DW Jr, Sides B, Bridwell KH (2007) Surgical revision rates of hooks versus hybrid versus screws versus combined anteroposterior spinal fusion for adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 32:2258–2264. https://doi.org/10.1097/BRS.0b013e31814b1ba6
Luo M, Wang W, Shen M, Luo X, Xia L (2017) Does higher screw density improve radiographic and clinical outcomes in adolescent idiopathic scoliosis? A systematic review and pooled analysis. J Neurosurg: Pediatr PED 19:448–457. https://doi.org/10.3171/2016.11.Peds16334
Wang X, Larson AN, Crandall DG, Parent S, Labelle H, Ledonio CGT, Aubin C-E (2017) Biomechanical effect of pedicle screw distribution in AIS instrumentation using a segmental translation technique: computer modeling and simulation. Scoliosis Spinal Disord 12:13. https://doi.org/10.1186/s13013-017-0120-4
Quan GM, Gibson MJ (2010) Correction of main thoracic adolescent idiopathic scoliosis using pedicle screw instrumentation: does higher implant density improve correction? Spine (Phila Pa 1976) 35:562–567. https://doi.org/10.1097/BRS.0b013e3181b4af34
Bharucha NJ, Lonner BS, Auerbach JD, Kean KE, Trobisch PD (2013) Low-density versus high-density thoracic pedicle screw constructs in adolescent idiopathic scoliosis: do more screws lead to a better outcome? Spine J 13:375–381. https://doi.org/10.1016/j.spinee.2012.05.029
Lenke LG, Betz RR, Harms J, Bridwell KH, Clements DH, Lowe TG, Blanke K (2001) Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am 83:1169–1181
D’Agostino RB Jr, D’Agostino RB Sr (2007) Estimating treatment effects using observational data. JAMA 297:314–316. https://doi.org/10.1001/jama.297.3.314
Salas M, Hofman A, Stricker BH (1999) Confounding by indication: an example of variation in the use of epidemiologic terminology. Am J Epidemiol 149:981–983. https://doi.org/10.1093/oxfordjournals.aje.a009758
Mitchell JD, Gage BF, Fergestrom N, Novak E, Villines TC (2020) Inverse probability of treatment weighting (propensity score) using the military health system data repository and national death index. J Vis Exp. https://doi.org/10.3791/59825
Austin PC (2009) Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med 28:3083–3107. https://doi.org/10.1002/sim.3697
Soucacos PN, Zacharis K, Soultanis K, Gelalis J, Xenakis T, Beris AE (2000) Risk factors for idiopathic scoliosis: review of a 6-year prospective study. Orthopedics 23:833–838
Soucacos PN, Zacharis K, Gelalis J, Soultanis K, Kalos N, Beris A, Xenakis T, Johnson EO (1998) Assessment of curve progression in idiopathic scoliosis. Eur Spine J 7:270–277. https://doi.org/10.1007/s005860050074
Ledonio CG, Polly DW Jr, Vitale MG, Wang Q, Richards BS (2011) Pediatric pedicle screws: comparative effectiveness and safety: a systematic literature review from the Scoliosis Research Society and the Pediatric Orthopaedic Society of North America task force. J Bone Joint Surg Am 93:1227–1234. https://doi.org/10.2106/jbjs.J.00678
Shen M, Jiang H, Luo M, Wang W, Li N, Wang L, Xia L (2017) Comparison of low density and high density pedicle screw instrumentation in Lenke 1 adolescent idiopathic scoliosis. BMC Musculoskelet Disord 18:336. https://doi.org/10.1186/s12891-017-1695-x
Wagala NN, Marasigan JAM, Mian HM, Schwend RM (2021) Operative time in adolescent idiopathic scoliosis surgery: a need for a standard definition. J Pediatr Orthop B 30:205–210. https://doi.org/10.1097/bpb.0000000000000754
Tang CYK, Kamath VHD, Cheung PWH, Cheung JPY (2021) Predictive factors for intraoperative blood loss in surgery for adolescent idiopathic scoliosis. BMC Musculoskelet Disord 22:225. https://doi.org/10.1186/s12891-021-04104-z
Lenz M, Oikonomidis S, Harland A, Fürnstahl P, Farshad M, Bredow J, Eysel P, Scheyerer MJ (2021) Scoliosis and Prognosis—a systematic review regarding patient-specific and radiological predictive factors for curve progression. Eur Spine J 30:1813–1822. https://doi.org/10.1007/s00586-021-06817-0
Robinson R (1993) Cost-utility analysis. Br Med J 307:859–862. https://doi.org/10.1136/bmj.307.6908.859
Kato S, Murray J-C, Ganau M, Tan Y, Oshima Y, Tanaka S (2018) Does posterior scoliosis correction improve respiratory function in adolescent idiopathic scoliosis? A systematic review and meta-analysis. Glob Spine J 9:866–873. https://doi.org/10.1177/2192568218811312
Acknowledgements
The authors would like to thank Miss Suchitphon Chanchoo for her assistance in statistical analysis and the Siriraj orthopedic research unit staff.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
Conceptualization was contributed by CC, JP, and TA; methodology was contributed by CC, NA, and PL; software was contributed by NA; validation was contributed by CC and TA; formal analysis was contributed by NA and JP; investigation was contributed by JP, MR, PL, SW and TA; resources were contributed by CC, MR, PL, SW, TA, and EK; data curation was contributed by NA, JP, and EK; writing—original draft preparation was contributed by NA; writing—review and editing was contributed by CC, MR, PL, SW, TA, and EK; visualization was contributed by MR, PL, SW, EK; supervision was contributed by CC; project administration was contributed by TA. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
This study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board.
Consent to participate
As it is a retrospective study and data was reviewed retrospectively from chart review, so patient’s consents are waived with the approval of the Institutional Review Board.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chotigavanichaya, C., Adulkasem, N., Pisutbenya, J. et al. Comparative effectiveness of different pedicle screw density patterns in spinal deformity correction of small and flexible operative adolescent idiopathic scoliosis: inverse probability of treatment weighting analysis. Eur Spine J 32, 2203–2212 (2023). https://doi.org/10.1007/s00586-023-07615-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07615-6