Abstract
Purpose
To evaluate the motion-preserving properties of vertebral body tethering with varying cord/screw constructs and cord thicknesses in cadaveric thoracolumbar spines.
Methods
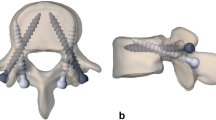
In vitro flexibility tests were performed on six fresh-frozen human cadaveric spines (T1-L5) (2 M, 4F) with a median age of 63 (59-to-80). An ± 8 Nm load was applied to determine range of motion (ROM) in flexion–extension (FE), lateral bending (LB), and axial rotation (AR) in the thoracic and lumbar spine. Specimens were tested with screws (T5-L4) and without cords. Single (4.0 mm and 5.0 mm) and double (4.0 mm) cord constructs were sequentially tensioned to 100 N and tested: (1) Single 4.0 mm and (2) 5.0 mm cords (T5-T12); (3) Double 4.0 mm cords (T5-12); (4) Single 4.0 mm and (5) 5.0 mm cord (T12-L4); (6) Double 4.0 mm cords (T12-L4).
Results
In the thoracic spine (T5-T12), 4.0–5.0 mm single-cord constructs showed slight reductions in FE and 27–33% reductions in LB compared to intact, while double-cord constructs showed reductions of 24% and 40%, respectively. In the lumbar spine (T12-L4), double-cord constructs had greater reductions in FE (24%), LB (74%), and AR (25%) compared to intact, while single-cord constructs exhibited reductions of 2–4%, 68–69%, and 19–20%, respectively.
Conclusions
The present biomechanical study found similar motion for 4.0–5.0 mm single-cord constructs and the least motion for double-cord constructs in the thoracic and lumbar spine suggesting that larger diameter 5.0 mm cords may be a more promising motion-preserving option, due to their increased durability compared to smaller cords. Future clinical studies are necessary to determine the impact of these findings on patient outcomes.







Similar content being viewed by others
References
Agabegi SS, Kazemi N, Sturm PF, Mehlman CT (2015) Natural history of adolescent idiopathic scoliosis in skeletally mature patients: a critical review. J Am Acad Orthop Surg 23:714–723. https://doi.org/10.5435/jaaos-d-14-00037
Weinstein SL, Dolan LA, Wright JG, Dobbs MB (2013) Effects of bracing in adolescents with idiopathic scoliosis. N Engl J Med 369:1512–1521. https://doi.org/10.1056/NEJMoa1307337
Trobisch P, Suess O, Schwab F (2010) Idiopathic scoliosis. Dtsch Arztebl Int. https://doi.org/10.3238/arztebl.2010.0875
Danielsson AJ, Romberg K, Nachemson AL (2006) Spinal range of motion, muscle endurance, and back pain and function at least 20 years after fusion or brace treatment for adolescent idiopathic scoliosis: a case-control study. Spine (Phila Pa 1976). https://doi.org/10.1097/01.brs.0000197652.52890.71
Kepler CK, Meredith DS, Green DW, Widmann RF (2012) Long-term outcomes after posterior spine fusion for adolescent idiopathic scoliosis. Curr Opin Pediatr 24:68–75. https://doi.org/10.1097/MOP.0b013e32834ec982
Green DW, Lawhorne TW 3rd, Widmann RF, Kepler CK, Ahern C, Mintz DN, Rawlins BA, Burke SW, Boachie-Adjei O (2011) Long-term magnetic resonance imaging follow-up demonstrates minimal transitional level lumbar disc degeneration after posterior spine fusion for adolescent idiopathic scoliosis. Spine (Phila Pa 1976). https://doi.org/10.1097/BRS.0b013e3181ff1ea9
Samdani AF, Ames RJ, Kimball JS, Pahys JM, Grewal H, Pelletier GJ, Betz RR (2014) Anterior vertebral body tethering for idiopathic scoliosis: two-year results. Spine (Phila Pa 1976). https://doi.org/10.1097/brs.0000000000000472
Samdani AF, Ames RJ, Kimball JS, Pahys JM, Grewal H, Pelletier GJ, Betz RR (2015) Anterior vertebral body tethering for immature adolescent idiopathic scoliosis: one-year results on the first 32 patients. Eur Spine J 24:1533–1539. https://doi.org/10.1007/s00586-014-3706-z
Kasliwal MK, Shaffrey CI, Lenke LG, Dettori JR, Ely CG, Smith JS (2012) Frequency, risk factors, and treatment of distal adjacent segment pathology after long thoracolumbar fusion: a systematic review. Spine (Phila Pa 1976). https://doi.org/10.1097/BRS.0b013e31826d62c9
Betz RR, Ranade A, Samdani AF, Chafetz R, D’Andrea LP, Gaughan JP, Asghar J, Grewal H, Mulcahey MJ (2010) Vertebral body stapling: a fusionless treatment option for a growing child with moderate idiopathic scoliosis. Spine (Phila Pa 1976). https://doi.org/10.1097/BRS.0b013e3181c6dff5
Newton PO, Farnsworth CL, Faro FD, Mahar AT, Odell TR, Mohamad F, Breisch E, Fricka K, Upasani VV, Amiel D (2008) Spinal growth modulation with an anterolateral flexible tether in an immature bovine model: disc health and motion preservation. Spine (Phila Pa 1976). https://doi.org/10.1097/BRS.0b013e31816950a0
Newton PO, Fricka KB, Lee SS, Farnsworth CL, Cox TG, Mahar AT (2002) Asymmetrical flexible tethering of spine growth in an immature bovine model. Spine (Phila Pa 1976). https://doi.org/10.1097/00007632-200204010-00004
Crawford CH 3rd, Lenke LG (2010) Growth modulation by means of anterior tethering resulting in progressive correction of juvenile idiopathic scoliosis: a case report. J Bone Joint Surg Am 92:202–209. https://doi.org/10.2106/jbjs.H.01728
Lavelle WF, Moldavsky M, Cai Y, Ordway NR, Bucklen BS (2016) An initial biomechanical investigation of fusionless anterior tether constructs for controlled scoliosis correction. Spine J 16:408–413. https://doi.org/10.1016/j.spinee.2015.11.004
Newton PO, Faro FD, Farnsworth CL, Shapiro GS, Mohamad F, Parent S, Fricka K (2005) Multilevel spinal growth modulation with an anterolateral flexible tether in an immature bovine model. Spine (Phila Pa 1976). https://doi.org/10.1097/01.brs.0000188267.66847.bf
Braun JT, Ogilvie JW, Akyuz E, Brodke DS, Bachus KN (2006) Creation of an experimental idiopathic-type scoliosis in an immature goat model using a flexible posterior asymmetric tether. Spine (Phila Pa 1976). https://doi.org/10.1097/01.brs.0000219869.01599.6b
Miyanji F, Pawelek J, Nasto LA, Rushton P, Simmonds A, Parent S (2020) Safety and efficacy of anterior vertebral body tethering in the treatment of idiopathic scoliosis. Bone Jt J. https://doi.org/10.1302/0301-620x.102b12.Bjj-2020-0426.R1
Newton PO, Bartley CE, Bastrom TP, Kluck DG, Saito W, Yaszay B (2020) Anterior spinal growth modulation in skeletally immature patients with idiopathic scoliosis: a comparison with posterior spinal fusion at 2 to 5 years postoperatively. J Bone Jt Surg Am 102:769–777. https://doi.org/10.2106/jbjs.19.01176
Newton PO, Kluck DG, Saito W, Yaszay B, Bartley CE, Bastrom TP (2018) Anterior spinal growth tethering for skeletally immature patients with scoliosis: a retrospective look two to four years postoperatively. J Bone Jt Surg Am 100:1691–1697. https://doi.org/10.2106/jbjs.18.00287
Samdani AF, Pahys JM, Ames RJ, Grewal H, Pelletier GJ, Hwang SW, Betz RR (2021) Prospective follow-up report on anterior vertebral body tethering for idiopathic scoliosis: interim results from an FDA IDE study. J Bone Joint Surg Am 103:1611–1619. https://doi.org/10.2106/jbjs.20.01503
Hoernschemeyer DG, Boeyer ME, Robertson ME, Loftis CM, Worley JR, Tweedy NM, Gupta SU, Duren DL, Holzhauser CM, Ramachandran VM (2020) Anterior vertebral body tethering for adolescent scoliosis with growth remaining: a retrospective review of 2 to 5-year postoperative results. J Bone Joint Surg Am 102:1169–1176. https://doi.org/10.2106/jbjs.19.00980
Baroncini A, Trobisch PD, Birkenmaier C, Da Paz S, Migliorini F (2021) Radiographic results after vertebral body tethering. Z Orthop Unfall. https://doi.org/10.1055/a-1387-8334
Nicolini LF, Kobbe P, Seggewiß J, Greven J, Ribeiro M, Beckmann A, Da Paz S, Eschweiler J, Prescher A, Markert B, Stoffel M, Hildebrand F, Trobisch PD (2021) Motion preservation surgery for scoliosis with a vertebral body tethering system: a biomechanical study. Eur Spine J. https://doi.org/10.1007/s00586-021-07035-4
Trobisch P, Baroncini A, Berrer A, Da Paz S (2022) Difference between radiographically suspected and intraoperatively confirmed tether breakages after vertebral body tethering for idiopathic scoliosis. Eur Spine J. https://doi.org/10.1007/s00586-021-07107-5
Tan JS, Kayanja MM, St Clair SF (2010) The difference in spine specimen dual-energy X-ray absorptiometry bone mineral density between in situ and in vitro scans. Spine J 10:784–788. https://doi.org/10.1016/j.spinee.2010.02.016
Wilke HJJB, Wenger K, Claes LE (1998) Spinal segment range of motion as a function of in vitro test conditions: effects of exposure period, accumulated cycles, angular-deformation rate, and moisture condition. Anat Rec 251:15–19
Goel VK, Panjabi MM, Patwardhan AG, Dooris AP, Serhan H, American Society for T, Materials (2006) Test protocols for evaluation of spinal implants. J Bone Jt Surg Am 88(Suppl 2):103–109. https://doi.org/10.2106/JBJS.E.01363
Wilke HJ, Herkommer A, Werner K, Liebsch C (2017) In vitro analysis of the segmental flexibility of the thoracic spine. PLoS ONE. https://doi.org/10.1371/journal.pone.0177823
Trobisch PD, Kobbe P, Baroncini A (2020) Dynamic scoliosis correction as alternative treatment for patients with adolescent idiopathic scoliosis: a non-fusion surgical technique. Z Orthop Unfall 158:641–646. https://doi.org/10.1055/a-0983-1265
Pehlivanoglu T, Oltulu I, Ofluoglu E, Sarioglu E, Altun G, Korkmaz M, Yildirim K, Aydogan M (2020) Thoracoscopic vertebral body tethering for adolescent idiopathic scoliosis: a minimum of 2 years’ results of 21 patients. J Pediatr Orthop 40:575–580. https://doi.org/10.1097/bpo.0000000000001590
Jackson TJ, Milbrandt TA, Mathew SE, Heilman JA, Larson AN (2022) Intervertebral disk health following vertebral body tethering for adolescent idiopathic scoliosis: a preliminary study. J Pediatr Orthop 42:347–353. https://doi.org/10.1097/BPO.0000000000002172
Yucekul A, Akpunarli B, Durbas A, Zulemyan T, Havlucu I, Ergene G, Senay S, Yalinay Dikmen P, Turgut Balci S, Karaarslan E, Yavuz Y, Yilgor C, Alanay A (2021) Does vertebral body tethering cause disc and facet joint degeneration? A preliminary MRI study with minimum two years follow-up. Spine J 21:1793–1801. https://doi.org/10.1016/j.spinee.2021.05.020
Nicolini LFGJ, Krobbe P, Hildebrand F, Stoffel M, Markert B, Yllera BM, Simões MS, Mello Roesle CR, Fancello EA (2022) The effects of tether pretension within vertebral body tethering on the biomechanics of the spine: a finite element analysis. Latin Am J Solids Struct. https://doi.org/10.1590/1679-78256932
Trobisch PD, Baroncini A (2021) Preliminary outcomes after vertebral body tethering (VBT) for lumbar curves and subanalysis of a 1- versus 2-tether construct. Eur Spine J 30:3570–3576. https://doi.org/10.1007/s00586-021-07009-6
Bernard J, Bishop T, Herzog J, Haleem S, Lupu C, Ajayi B, Lui DF (2022) Dual modality of vertebral body tethering : anterior scoliosis correction versus growth modulation with mean follow-up of five years. Bone Jt Open 3:123–129. https://doi.org/10.1302/2633-1462.32.Bjo-2021-0120.R1
Baroncini A, Migliorini F, Eschweiler J, Hildebrand F, Trobisch P (2022) The timing of tether breakage influences clinical results after VBT. Eur Spine J 31:2362–2367. https://doi.org/10.1007/s00586-022-07321-9
Holewijn RM, de Kleuver M, van der Veen AJ, Emanuel KS, Bisschop A, Stadhouder A, van Royen BJ, Kingma I (2017) A novel spinal implant for fusionless scoliosis correction: a biomechanical analysis of the motion preserving properties of a posterior periapical concave distraction device. Global Spine J 7:400–409. https://doi.org/10.1177/2192568217699377
Funding
Funding for this study was provided by Globus Medical, Inc. (GMI).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
PDT receives consulting fees from GMI and Stryker Spine, and lecture fees from ZimVie and Triaspine. RRB receives royalties from GMI, DePuy Synthes Spine, SpineGuard, Thieme Medical Publishers; Speakers bureau payments from GMI and DePuy Synthes Spine; Consulting fees from GMI, DePuy Synthes Spine, SpineGuard, SpineWelding, Addivation, and Orthopediatric Corp and stock options from SpineGuard, SpineWelding, Orthopediatric Corp, Abyrx, Electrocore, H-CYTE, Life Unit, Molecular Surface Technologies, and Orthobond. RRB is also on the Life Unit and Molecular Surface Technologies boards and is the co-owner of NOFUSCO. CLA, LC, DRC, MRO, and MDA have no disclosures to report. EKE, JMM, DBA, JPM, and BSB are paid employees of GMI. JMM, JPM, and BSM also receive stock options from GMI.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Trobisch, P., Mahoney, J.M., Eichenlaub, E.K. et al. An investigation of range of motion preservation in fusionless anterior double screw and cord constructs for scoliosis correction. Eur Spine J 32, 1173–1186 (2023). https://doi.org/10.1007/s00586-023-07608-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07608-5