Abstract
Purpose
To investigate whether (1) there is a difference between patients with normal or sagittal spinal and spinopelvic malalignment in terms of their paraspinal muscle composition and (2) if sagittal malalignment can be predicted using muscle parameters.
Methods
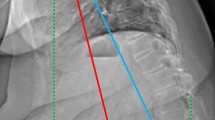
A retrospective review of patients undergoing posterior lumbar fusion surgery was conducted. A MRI-based muscle measurement technique was used to assess the cross-sectional area, the functional cross-sectional area, the intramuscular fat and fat infiltration (FI) for the psoas and the posterior paraspinal muscles (PPM). Intervertebral disc degeneration was graded for levels L1 to S1. Sagittal vertical axis (SVA; ≥ 50 mm defined as spinal malalignment), pelvic incidence (PI) and lumbar lordosis (LL) were measured, and PI-LL mismatch (PI-LL; ≥ 10° defined as spinopelvic malalignment) was calculated. A receiver operating characteristic (ROC) analysis was conducted to determine the specificity and sensitivity of the FIPPM for predicting sagittal malalignment.
Results
One hundred and fifty patients were analysed. The PI-LL and SVA malalignment groups were found to have a significantly higher FIPPM (PI-LL:47.0 vs. 42.1%; p = 0.019; SVA: 47.7 vs. 41.8%; p = 0.040). ROC analysis predicted sagittal spinal malalignment using FIPPM (cut-off value 42.69%) with a sensitivity of 73.4% and a specificity of 54.1% with an area under the curve of 0.662.
Conclusion
Significant differences in the muscle composition between normal and malalignment groups with respect to FIPPM in both sagittal spinal and spinopelvic alignment were found. This work underlines the imminent impact of the paraspinal musculature on the sagittal alignment.





Similar content being viewed by others
Data availability
The datasets generated and analysed during the current study are available from the corresponding author on reasonable request.
References
Teichtahl AJ, Urquhart DM, Wang Y et al (2015) Fat infiltration of paraspinal muscles is associated with low back pain, disability, and structural abnormalities in community-based adults. Spine J 15(7):1593–1601
Goubert D, De Pauw R, Meeus M et al (2017) Lumbar muscle structure and function in chronic versus recurrent low back pain: a cross-sectional study. Spine J 17(9):1285–1296
Faur C, Patrascu JM, Haragus H, Anglitoiu B (2019) Correlation between multifidus fatty atrophy and lumbar disc degeneration in low back pain. BMC Musculoskelet Disord 20(1):414
Ranger TA, Cicuttini FM, Jensen TS, Heritier S, Urquhart DM (2019) Paraspinal muscle cross-sectional area predicts low back disability but not pain intensity. Spine J 19(5):862–868
Katsu M, Ohba T, Ebata S, Oba H, Koyama K, Haro H (2020) Potential role of paraspinal musculature in the maintenance of spinopelvic alignment in patients with adult spinal deformities. Clin Spine Surg 33(2):E76–E80
Le Huec JC, Charosky S, Barrey C, Rigal J, Aunoble S (2011) Sagittal imbalance cascade for simple degenerative spine and consequences: algorithm of decision for appropriate treatment. Eur Spine J 20(Suppl 5):699–703
Marcus RL, Addison O, Kidde JP, Dibble LE, Lastayo PC (2010) Skeletal muscle fat infiltration: impact of age, inactivity, and exercise. J Nutr Health Aging 14(5):362–366
Volpi E, Nazemi R, Fujita S (2004) Muscle tissue changes with aging. Curr Opin Clin Nutr Metab Care 7(4):405–410
Hamrick MW, McGee-Lawrence ME, Frechette DM (2016) Fatty infiltration of skeletal muscle: mechanisms and comparisons with bone marrow adiposity. Front Endocrinol (Lausanne) 7:69
Visser M, Kritchevsky SB, Goodpaster BH et al (2002) Leg muscle mass and composition in relation to lower extremity performance in men and women aged 70 to 79: the health, aging and body composition study. J Am Geriatr Soc 50(5):897–904
Goodpaster BH, Park SW, Harris TB et al (2006) The loss of skeletal muscle strength, mass, and quality in older adults: the health, aging and body composition study. J Gerontol A Biol Sci Med Sci 61(10):1059–1064
Goodpaster BH, Carlson CL, Visser M et al (2001) Attenuation of skeletal muscle and strength in the elderly: the health ABC study. J Appl Physiol 90(6):2157–65
Bokshan SL, Han AL, DePasse JM et al (2016) Effect of sarcopenia on postoperative morbidity and mortality after thoracolumbar spine surgery. Orthopedics 39(6):e1159–e1164
Chang MY, Park Y, Ha JW et al (2019) Paraspinal lean muscle mass measurement using spine MRI as a predictor of adjacent segment disease after lumbar fusion: a propensity score-matched case-control analysis. AJR Am J Roentgenol 212:1–8
Choi MK, Kim SB, Park CK, Malla HP, Kim SM (2017) Cross-sectional area of the lumbar spine trunk muscle and posterior lumbar interbody fusion rate: a retrospective study. Clin Spine Surg 30(6):E798–E803
Choi MK, Kim SB, Park BJ, Park CK, Kim SM (2016) Do trunk muscles affect the lumbar interbody fusion rate?: Correlation of trunk muscle cross sectional area and fusion rates after posterior lumbar interbody fusion using stand-alone cage. J Korean Neurosurg Soc 59(3):276–281
Kim JY, Ryu DS, Paik HK et al (2016) Paraspinal muscle, facet joint, and disc problems: risk factors for adjacent segment degeneration after lumbar fusion. Spine J 16(7):867–875
Prost S, Blondel B, Bauduin E, et al. (2022) Do age-related variations of sagittal alignment rely on spinopelvic organization? An observational study of 1540 subjects. Global Spine J, 21925682221074660
Hu Z, Man G, Yeung KH et al (2021) Age- and gender-related normative value of whole-body sagittal alignment based on 584 asymptomatic Chinese adult population from age 20 to 89. Stud Health Technol Inform 280:66–71
Iyer S, Lenke LG, Nemani VM et al (2016) Variations in sagittal alignment parameters based on age: a prospective study of asymptomatic volunteers using full-body radiographs. Spine (Phila Pa 1976) 41(23):1826–36
Schwab FJ, Blondel B, Bess S et al (2013) Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: a prospective multicenter analysis. Spine (Phila Pa 1976) 38(13):E803-12
Smith MW, Annis P, Lawrence BD, Daubs MD, Brodke DS (2015) Acute proximal junctional failure in patients with preoperative sagittal imbalance. Spine J 15(10):2142–2148
Marie-Hardy L, Pascal-Moussellard H, Barnaba A, Bonaccorsi R, Scemama C (2020) Screw loosening in posterior spine fusion: prevalence and risk factors. Global Spine J 10(5):598–602
Faron A, Luetkens JA, Schmeel FC, Kuetting DLR, Thomas D, Sprinkart AM (2019) Quantification of fat and skeletal muscle tissue at abdominal computed tomography: associations between single-slice measurements and total compartment volumes. Abdom Radiol (NY) 44(5):1907–1916
Crawford RJ, Filli L, Elliott JM et al (2016) Age- and level-dependence of fatty infiltration in lumbar paravertebral muscles of healthy volunteers. AJNR Am J Neuroradiol 37(4):742–748
Moser M, Amini DA, Jones C, et al. (2022) The predictive value of psoas and paraspinal muscle parameters measured on MRI for severe cage subsidence after standalone lateral lumbar interbody fusion. Spine J
Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N (2001) Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976) 26(17):1873–1878
Urrutia J, Besa P, Campos M et al (2016) The Pfirrmann classification of lumbar intervertebral disc degeneration: an independent inter- and intra-observer agreement assessment. Eur Spine J 25(9):2728–2733
Kyrola KK, Salme J, Tuija J, Tero I, Eero K, Arja H (2018) Intra- and interrater reliability of sagittal spinopelvic parameters on full-spine radiographs in adults with symptomatic spinal disorders. Neurospine 15(2):175–181
Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F (2005) The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976) 30(18):2024–2029
Zhu W, Wang W, Kong C, Wang Y, Pan F, Lu S (2020) Lumbar muscle fat content has more correlations with living quality than sagittal vertical axis in elderly patients with degenerative lumbar disorders. Clin Interv Aging 15:1717–1726
Le Huec JC, Thompson W, Mohsinaly Y, Barrey C, Faundez A (2019) Sagittal balance of the spine. Eur Spine J 28(9):1889–1905
Dubousset J (1994) Three-dimensional analysis of the scoliotic deformity. The pediatric spine: principles and practice
Hori Y, Hoshino M, Inage K et al (2019) ISSLS prize in clinical science 2019: clinical importance of trunk muscle mass for low back pain, spinal balance, and quality of life-a multicenter cross-sectional study. Eur Spine J 28(5):914–921
Enoka RM, Duchateau J (2019) Chapter 7—Muscle function: strength, speed, and fatigability. In: Zoladz JA (ed) Muscle and exercise physiology. Cambridge, Academic Press, pp 129–157
Ward SR, Kim CW, Eng CM et al (2009) Architectural analysis and intraoperative measurements demonstrate the unique design of the multifidus muscle for lumbar spine stability. J Bone Joint Surg Am 91(1):176–185
Zwambag DP, Ricketts TA, Brown SH (2014) Sarcomere length organization as a design for cooperative function amongst all lumbar spine muscles. J Biomech 47(12):3087–3093
Zollner AM, Abilez OJ, Bol M, Kuhl E (2012) Stretching skeletal muscle: chronic muscle lengthening through sarcomerogenesis. PLoS ONE 7(10):e45661
Allen DG, Whitehead NP, Yeung EW (2005) Mechanisms of stretch-induced muscle damage in normal and dystrophic muscle: role of ionic changes. J Physiol 567(Pt 3):723–735
Flores DV, Mejia Gomez C, Estrada-Castrillon M, Smitaman E, Pathria MN (2018) MR imaging of muscle trauma: anatomy, biomechanics, pathophysiology, and imaging appearance. Radiographics 38(1):124–148
Cianferotti L, Brandi ML (2014) Muscle-bone interactions: basic and clinical aspects. Endocrine 45(2):165–177
Yin L, Xu Z, Wang L et al (2020) Associations of muscle size and density with proximal femur bone in a community dwelling older population. Front Endocrinol (Lausanne) 11:503
Khalid SI, Nunna RS, Maasarani S et al (2020) Association of osteopenia and osteoporosis with higher rates of pseudarthrosis and revision surgery in adult patients undergoing single-level lumbar fusion. Neurosurg Focus 49(2):E6
Yuan L, Zhang X, Zeng Y, Chen Z, Li W (2021) Incidence, risk, and outcome of pedicle screw loosening in degenerative lumbar scoliosis patients undergoing long-segment fusion. Global Spine J, 21925682211017477
Jun HS, Kim JH, Ahn JH et al (2016) The effect of lumbar spinal muscle on spinal sagittal alignment: evaluating muscle quantity and quality. Neurosurgery 79(6):847–855
Levine D, Whittle MW (1996) The effects of pelvic movement on lumbar lordosis in the standing position. J Orthop Sports Phys Ther 24(3):130–135
Pesenti S, Lafage R, Stein D et al (2018) The amount of proximal lumbar lordosis is related to pelvic incidence. Clin Orthop Relat Res 476(8):1603–1611
Han G, Zou D, Liu Z et al (2022) Fat infiltration of paraspinal muscles as an independent risk for bone nonunion after posterior lumbar interbody fusion. BMC Musculoskelet Disord 23(1):232
Kim JB, Park SW, Lee YS, Nam TK, Park YS, Kim YB (2015) The effects of spinopelvic parameters and paraspinal muscle degeneration on S1 screw loosening. J Korean Neurosurg Soc 58(4):357–362
Acknowledgements
Dr. Sama reports royalties from Ortho Development, Corp.; private investments for Vestia Ventures MiRUS Investment, LLC, IVY II, LLC, ISPH 3, LLC, and VBros Venture Partners X Centinel Spine; consulting fee from Clariance, Inc., Kuros Biosciences AG, and Medical Device Business Service, Inc.; speaking and teaching arrangements of DePuy Synthes Products, Inc.; membership of scientific advisory board of Clariance, Inc., and Kuros Biosciences AG; and trips/travel of Medical Device Business research support from Spinal Kinetics, Inc., outside the submitted work. Dr. Cammisa reports royalties from NuVasive, Inc. Accelus; private investments for 4WEB Medical/4WEB, Inc., Bonovo Orthopedics, Inc., Healthpoint Capital Partners, LP, ISPH II, LLC, ISPH 3 Holdings, LLC, Ivy Healthcare Capital Partners, LLC, Medical Device Partners II, LLC, Medical Device Partners III, LLC, Orthobond Corporation, Spine Biopharma, LLC, Synexis, LLC, Tissue Differentiation Intelligence, LLC, VBVP VI, LLC, VBVP X, LLC (Centinel) and Woven Orthopedics Technologies; consulting fees from 4WEB Medical/4WEB, Inc., DePuy Synthes Spine, NuVasive, Inc., Spine Biopharma, LLC, and Synexis, LLC, Accelus; membership of scientific advisory board/other office of Healthpoint Capital Partners, LPIVY, Medical Device Partners III, LLC, Orthobond Corporation, Spine Biopharma, LLC, Synexis, LLC, and Woven Orthopedic Technologies; and research support from 4WEB Medical/4WEB, Inc., Mallinckrodt Pharmaceuticals, Camber Spine, and Centinel Spine, outside the submitted work. Dr. Girardi reports royalties from Lanx, Inc., and Ortho Development Corp.; private investments for Centinel Spine, and BCMID; stock ownership of Healthpoint Capital Partners, LP; and consulting fees from NuVasive, Inc., and DePuy Synthes Spine, outside the submitted work. Dr. Hughes reports research support from NuVasive, Inc. and Kuros Biosciences AG; and fellowship support from NuVasive, Inc. and Kuros Biosciences AG, outside the submitted work.
Funding
Research reported in this publication was supported by the National Center for Advancing Translational Science of the National Institute of Health Under Award Number UL1TR002384.
Author information
Authors and Affiliations
Contributions
Conception and design was done by M.M. Acquisition of data was done by M.M. and H.H. Analysis and interpretation of data were carried out by M.M. and H.H. Drafting the article was done by M.M. Critically revising the article was done by all authors. Preparation of graphical content was done by M.M. and H.H. Reviewed submitted version of manuscript was done by all authors. H.H. approved the final version of the manuscript on behalf of all authors. Statistical analysis was done by M.M. and J.Z. Administrative/technical/material support was done by E.T.T. and J.S. Study supervision was done by A.H.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest regarding this work.
Ethical approval
The investigation was approved by the institutional review board.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The work was performed at the Hospital for Special Surgery, New York City, NY, USA. The institutional review board of the Hospital for Special Surgery approved this study.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Muellner, M., Haffer, H., Chiapparelli, E. et al. Differences in lumbar paraspinal muscle morphology in patients with sagittal malalignment undergoing posterior lumbar fusion surgery. Eur Spine J 31, 3109–3118 (2022). https://doi.org/10.1007/s00586-022-07351-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-022-07351-3