Abstract
Purpose
To evaluate which cervical level is the most appropriate level to measure occipitocervical inclination (OCI).
Methods
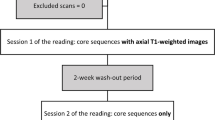
Sixty-two patients with multi-positional MRI: 24 males and 38 females, who had cervical lordosis and had a disk degeneration grade of 3 or less were included. We measured patient’s OCI at C3, C4, and C5, occipitocervical angle (OCA), occipitocervical distance (OCD), C2–7 angle, and cervical sagittal vertical axis (cSVA) in neutral, flexion, and extension position. The correlation between OCI and OCA, OCD, C2–7 angle, and cSVA on each cervical level in all three positions was tested using Pearson’s correlation coefficient test. The difference between OCIs at each cervical level was tested by Wilcoxon signed-rank test. p value of less than 0.05 was set as a statistically significant level.
Results
C5 OCI showed statistically significant correlation with OCA, OCD, C2–7 angle, and cSVA in all three positions (p < 0.05, r = 0.214–0.525). C3 OCI in flexion (p = 0.393, r = 0.081) and C4 OCI in neutral and flexion (neutral p = 0.275, r 0.104; flexion p = 0.987, r = 0.002) did not show significant correlation with C2–7 angle. There was a statistically significant difference between C3, C4, and C5 OCIs in neutral and extension position (p < 0.05). At the same time, OCI showed statistically strong correlation between adjacent cervical levels (p < 0.001, r = 0.627–0.822).
Conclusion
C5 cervical level is the most appropriate level for OCI measurement. OCI should be measured at the same cervical level at all time. C4 OCI can reliably substitute C5 OCI in case C5 which is invisible on radiographic image.
Graphical abstract
These slides can be retrieved under Electronic Supplementary Material.




Similar content being viewed by others
References
Yoon SD, Lee CH, Lee J, Choi JY, Min WK (2017) Occipitocervical inclination: new radiographic parameter of neutral occipitocervical position. Eur Spine J. https://doi.org/10.1007/s00586-017-5161-0
Miyata M, Neo M, Fujibayashi S, Ito H, Takemoto M, Nakamura T (2009) O-C2 angle as a predictor of dyspnea and/or dysphagia after occipitocervical fusion. Spine (Phila Pa 1976) 34(2):184–188. https://doi.org/10.1097/BRS.0b013e31818ff64e
Morita M, Nobuta M, Naruse H, Nakamura H (2011) Prolonged airway obstruction after posterior occipitocervical fusion: a case report and literature review. Adv Orthop 2011:791923. https://doi.org/10.4061/2011/791923
Phillips FM, Phillips CS, Wetzel FT, Gelinas C (1999) Occipitocervical neutral position. Possible surgical implications. Spine (Phila Pa 1976) 24(8):775–778
Izeki M, Neo M, Takemoto M, Fujibayashi S, Ito H, Nagai K, Matsuda S (2014) The O-C2 angle established at occipito-cervical fusion dictates the patient’s destiny in terms of postoperative dyspnea and/or dysphagia. Eur Spine J 23(2):328–336. https://doi.org/10.1007/s00586-013-2963-6
Riel RU, Lee MC, Kirkpatrick JS (2010) Measurement of a posterior occipitocervical fusion angle. J Spinal Disord Tech 23(1):27–29. https://doi.org/10.1097/BSD.0b013e318198164b
Tan J, Liao G, Liu S (2014) Evaluation of occipitocervical neutral position using lateral radiographs. J Orthop Surg Res 9:87. https://doi.org/10.1186/s13018-014-0087-2
Tian W, Yu J (2013) The role of C2–C7 and O-C2 angle in the development of dysphagia after cervical spine surgery. Dysphagia 28(2):131–138. https://doi.org/10.1007/s00455-012-9421-1
Cheung JP, Luk KD (2016) Complications of anterior and posterior cervical spine surgery. Asian Spine J 10(2):385–400. https://doi.org/10.4184/asj.2016.10.2.385
Davis JW, Kaups KL, Cunningham MA, Parks SN, Nowak TP, Bilello JF, Williams JL (2001) Routine evaluation of the cervical spine in head-injured patients with dynamic fluoroscopy: a reappraisal. J Trauma 50(6):1044–1047
Sierink JC, van Lieshout WA, Beenen LF, Schep NW, Vandertop WP, Goslings JC (2013) Systematic review of flexion/extension radiography of the cervical spine in trauma patients. Eur J Radiol 82(6):974–981. https://doi.org/10.1016/j.ejrad.2013.02.009
Suzuki A, Daubs MD, Inoue H, Hayashi T, Aghdasi B, Montgomery SR, Ruangchainikom M, Hu X, Lee CJ, Wang CJ, Wang BJ, Nakamura H (2013) Prevalence and motion characteristics of degenerative cervical spondylolisthesis in the symptomatic adult. Spine (Phila Pa 1976) 38(17):E1115–E1120. https://doi.org/10.1097/BRS.0b013e31829b1487
Ruangchainikom M, Daubs MD, Suzuki A, Hayashi T, Weintraub G, Lee CJ, Inoue H, Tian H, Aghdasi B, Scott TP, Phan KH, Chotivichit A, Wang JC (2014) Effect of cervical kyphotic deformity type on the motion characteristics and dynamic spinal cord compression. Spine (Phila Pa 1976) 39(12):932–938. https://doi.org/10.1097/BRS.0000000000000330
Phan KH, Daubs MD, Kupperman AI, Scott TP, Wang JC (2015) Kinematic analysis of diseased and adjacent segments in degenerative lumbar spondylolisthesis. Spine J 15(2):230–237. https://doi.org/10.1016/j.spinee.2014.08.453
Paholpak P, Tamai K, Shoell K, Sessumpun K, Buser Z, Wang JC (2017) Can multi-positional magnetic resonance imaging be used to evaluate angular parameters in cervical spine? A comparison of multi-positional MRI to dynamic plain radiograph. Eur Spine J. https://doi.org/10.1007/s00586-017-5306-1
Weng C, Wang J, Tuchman A, Fu C, Hsieh PC, Buser Z, Wang JC (2016) Influence of T1 slope on the cervical sagittal balance in degenerative cervical spine: an analysis using kinematic MRI. Spine (Phila Pa 1976) 41(3):185–190. https://doi.org/10.1097/BRS.0000000000001353
Ames CP, Blondel B, Scheer JK, Schwab FJ, Le Huec JC, Massicotte EM, Patel AA, Traynelis VC, Kim HJ, Shaffrey CI, Smith JS, Lafage V (2013) Cervical radiographical alignment: comprehensive assessment techniques and potential importance in cervical myelopathy. Spine (Phila Pa 1976) 38(22 Suppl 1):S149–S160. https://doi.org/10.1097/BRS.0b013e3182a7f449
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33(1):159–174
Evans JD (1996) Straightforward statistics for the behavioral sciences. Brooks/Cole Pub. Co., Pacific Grove
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No conflicts of interest for the current study.
Disclosure
Disclosures outside of submitted work: ZB- consultancy: Xenco Medical, AO Spine (past); Research Support: SeaSpine (paid directly to institution); JCW - Royalties – Biomet, Seaspine, Amedica, DePuy Synthes; Investments/Options – Bone Biologics, Pearldiver, Electrocore, Surgitech; Board of Directors - North American Spine Society, AO Foundation (20,000 honorariums for board position, plus travel for board meetings), Cervical Spine Research Society; Editorial Boards - Spine, The Spine Journal, Clinical Spine Surgery, Global Spine Journal; Fellowship Funding (paid directly to institution): AO Foundation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Paholpak, P., Formanek, B., Vega, A. et al. The most appropriate cervical vertebra for the measurement of occipitocervical inclination parameter: a validation study of C3, C4, and C5 levels using multi-positional magnetic resonance imaging. Eur Spine J 28, 2325–2332 (2019). https://doi.org/10.1007/s00586-019-06028-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-019-06028-8