Abstract
Purpose
Fatty infiltration (FI) is a feature of degenerating muscle that predominates in the low lumbar spine, associates with pain, and is confounded by age, spinal degeneration, and curvature. We determined rates for decline of lumbar muscle quality according to ethnicity, muscle, and spinal level in asymptomatic subjects.
Methods
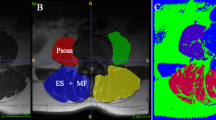
Cross-sectional simulation study assessing aggregated data; 650 Asians aged 20–89 years versus 80 Caucasians aged 20–62 years. Change in lumbar multifidus, erector spinae (ES), and psoas fat content were computed using synthetic data and Monte Carlo simulations. General linear regression models and multivariate adaptive regression splines enabled estimation of yearly decline rates [with 95% confidence intervals (CI)].
Results
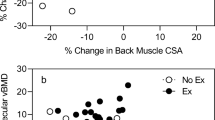
ES at L1–5 (total) shows steeply reduced density (rate; CI) for Asians in older (>53.3 years) adulthood (−0.32; −0.27 to −0.36/year). For Asians, multifidus (−0.18; −0.15 to −0.20/year) and psoas (−0.04; −0.03 to −0.06/year) also decline, while ES in younger ≤53.3 years) adults does not (0.06; 0.01–0.12/year). Caucasian multifidus declines (increasing FI % rate; CI) insignificantly faster (L1–5; 0.23; 0.10–0.36%/year) than ES (0.13; 0.04–0.22%/year). Multifidus decline does not differ between ethnicities. ES in older Asians generally declines fastest across ethnicities and muscles, and particularly in the low lumbar levels. Low lumbar levels show higher rates of decline in Asians, with mixed level-dependencies apparent in Caucasians.
Conclusions
Decline in lumbar muscle composition may differ between ethnicities and muscles. ES and low lumbar levels appear increasingly susceptible in Asians. Longitudinal studies examining rate of change to muscle composition may provide distinction between spinal conditions.




Similar content being viewed by others
Abbreviations
- APCT:
-
Abdomen and pelvis computer tomography
- CI:
-
95% confidence intervals
- ES:
-
Erector spinae
- FI:
-
Fatty infiltration
- LBP:
-
Low back pain
- MRI:
-
Magnetic resonance imaging
References
Elliott JM, Kerry R, Flynn T, Parrish TB (2013) Content not quantity is a better measure of muscle degeneration in whiplash. Man Ther 18:578–582. doi:10.1016/j.math.2013.02.002
Mitchell WK, Williams J, Atherton P, Larvin M, Lund J, Narici M (2012) Sarcopenia, dynapenia, and the impact of advancing age on human skeletal muscle size and strength; a quantitative review. Front Physiol 3:260. doi:10.3389/fphys.2012.00260
Fortin M, Gibbons LE, Videman T, Battie MC (2014) Do variations in paraspinal muscle morphology and composition predict low back pain in men? Scand J Med Sci Sports. doi:10.1111/sms.12301
Fortin M, Yuan Y, Battie MC (2013) Factors associated with paraspinal muscle asymmetry in size and composition in a general population sample of men. Phys Ther 93:1540–1550. doi:10.2522/ptj.20130051
Kalichman L, Hodges P, Li L, Guermazi A, Hunter DJ (2010) Changes in paraspinal muscles and their association with low back pain and spinal degeneration: CT study. Eur Spine J 19:1136–1144. doi:10.1007/s00586-009-1257-5
Meakin JR, Fulford J, Seymour R, Welsman JR, Knapp KM (2013) The relationship between sagittal curvature and extensor muscle volume in the lumbar spine. J Anat 222:608–614. doi:10.1111/joa.12047
Shahidi B, Parra CL, Berry DB, Hubbard JC, Gombatto S, Zlomislic V, Allen RT, Hughes-Austin J, Garfin S, Ward SR (2016) Contribution of lumbar spine pathology and age to paraspinal muscle size and fatty infiltration. Spine. doi:10.1097/brs.0000000000001848
Crawford R, Filli L, Elliott J, Nanz D, Fischer M, Marcon M, Ulbrich E (2016) Age- and level-dependence of fatty infiltration in lumbar paravertebral muscles of healthy volunteers. Am J Neuroradiol 37:742–748. doi:10.3174/ajnr.A4596
Valentin S, Licka T, Elliott J (2015) Age and side-related morphometric MRI evaluation of trunk muscles in people without back pain. Man Ther 20:90–95. doi:10.1016/j.math.2014.07.007
Haig AJ (2002) Paraspinal denervation and the spinal degenerative cascade. Spine J 2:372–380
Lee SH, Park SW, Kim YB, Nam TK, Lee YS (2017) The fatty degeneration of lumbar paraspinal muscles on computed tomography scan according to age and disc level. Spine J 17:81–87. doi:10.1016/j.spinee.2016.08.001
Abbott R, Pedler A, Sterling M, Hides J, Murphey T, Hoggarth M, Elliott J (2015) The geography of fatty infiltrates within the cervical multifidus and semispinalis cervicis in individuals with chronic whiplash-associated disorders. J Orthop Sports Phys Ther 45:8. doi:10.2519/jospt.2015.5719
Crawford R, Volken T, Valentin S, Melloh M, Elliott J (2016) Rate of lumbar paravertebral muscle fat infiltration versus spinal degeneration in asymptomatic populations: an age- aggregated cross-sectional simulation study. BMC Scoliosis Spinal Disord 11:21–29. doi:10.1186/s13013-016-0080-0
Karlsson A, Leinhard OD, Aslund U, West J, Romu T, Smedby O, Zsigmond P, Peolsson A (2016) An investigation of fat infiltration of the multifidus muscle in patients with severe neck symptoms associated with chronic whiplash-associated disorder. J Orthop Sports Phys Ther 46:886–893. doi:10.2519/jospt.2016.6553
O’Leary S, Jull G, Van Wyk L, Pedler A, Elliott J (2015) Morphological changes in the cervical muscles of women with chronic whiplash can be modified with exercise—a pilot study. Muscle Nerve. doi:10.1002/mus.24612
Hebert JJ, Kjaer P, Fritz JM, Walker BF (2014) The relationship of lumbar multifidus muscle morphology to previous, current, and future low back pain: a 9-year population-based prospective cohort study. Spine 39:1417–1425. doi:10.1097/brs.0000000000000424
Hyun SJ, Bae CW, Lee SH, Rhim SC (2016) Fatty degeneration of the paraspinal muscle in patients with degenerative lumbar kyphosis: a new evaluation method of quantitative digital analysis using MRI and CT scan. Clin Spine Surg 29:441–447. doi:10.1097/BSD.0b013e3182aa28b0
Bok DH, Kim J, Kim TH (2017) Comparison of MRI-defined back muscles volume between patients with ankylosing spondylitis and control patients with chronic back pain: age and spinopelvic alignment matched study. Eur Spine J 26:528–537. doi:10.1007/s00586-016-4889-2
Pezolato A, de Vasconcelos EE, Defino HL, Nogueira-Barbosa MH (2012) Fat infiltration in the lumbar multifidus and erector spinae muscles in subjects with sway-back posture. Eur Spine J 21:2158–2164. doi:10.1007/s00586-012-2286-z
Kalichman L, Klindukhov A, Li L, Linov L (2016) Indices of paraspinal muscles degeneration: reliability and association with facet joint osteoarthritis: feasibility study. Clin Spine Surg 29:465–470. doi:10.1097/BSD.0b013e31828be943
Teichtahl AJ, Urquhart DM, Wang Y, Wluka AE, Wijethilake P, O’Sullivan R, Cicuttini FM (2015) Fat infiltration of paraspinal muscles is associated with low back pain, disability, and structural abnormalities in community-based adults. Spine J 15:1593–1601. doi:10.1016/j.spinee.2015.03.039
Fortin M, Lazary A, Varga PP, McCall I, Battie MC (2016) Paraspinal muscle asymmetry and fat infiltration in patients with symptomatic disc herniation. Eur Spine J 25:1452–1459. doi:10.1007/s00586-016-4503-7
Brinjikji W, Luetmer PH, Comstock B, Bresnahan BW, Chen LE, Deyo RA, Halabi S, Turner JA, Avins AL, James K, Wald JT, Kallmes DF, Jarvik JG (2015) Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. Am J Neuroradiol 36:811–816. doi:10.3174/ajnr.A4173
Kirkaldy-Willis WH, Wedge JH, Yong-Hing K, Reilly J (1978) Pathology and pathogenesis of lumbar spondylosis and stenosis. Spine 3:319–328
Park S-W (2016) Sample sizes for Lee et al. study. Email communications with RJ Crawford between 21/11/2016 to 6/12/2016. Sample sizes provided 5/12/2016
Crawford R, Cornwall J, Abbott R, Elliott J (2017) Manually defining regions of interest when quantifying paravertebral muscles fatty infiltration from axial magnetic resonance imaging: a proposed method for the lumbar spine with anatomical cross-reference. BMC Musculoskelet Disord 18:25. doi:10.1186/s12891-016-1378-z
Milborrow S (2016) Earth: multivariate adaptive regression splines. Derived from mda:mars by Trevor Hastie and Rob Tibshirani. Uses Alan Miller’s Fortran utilities with Thomas Lumley’s leaps wrapper. https://CRAN.R-project.org/package=earth. Accessed 10 July 2017
Maatta J, Karppinen J, Luk KD, Cheung KM, Samartzis D (2015) Phenotype profiling of Modic changes of the lumbar spine and its association with other MRI phenotypes: a large-scale, population-based study. Spine J 15:1933–1942. doi:10.1016/j.spinee.2015.06.056
Dahlqvist JR, Vissing CR, Hedermann G, Thomsen C, Vissing J (2016) Fat replacement of paraspinal muscles with aging in healthy adults. Med Sci Sports Exerc. doi:10.1249/mss.0000000000001119
Fortin M, Videman T, Gibbons LE, Battie MC (2014) Paraspinal muscle morphology and composition: a 15-yr longitudinal magnetic resonance imaging study. Med Sci Sports Exerc 46:893–901. doi:10.1249/mss.0000000000000179
Chang DG, Healey RM, Snyder AJ, Sayson JV, Macias BR, Coughlin DG, Bailey JF, Parazynski SE, Lotz JC, Hargens AR (2016) Lumbar spine paraspinal muscle and intervertebral disc height changes in astronauts after long-duration spaceflight on the international space station. Spine 41:1917–1924. doi:10.1097/brs.0000000000001873
Ploumis A, Michailidis N, Christodoulou P, Kalaitzoglou I, Gouvas G, Beris A (2011) Ipsilateral atrophy of paraspinal and psoas muscle in unilateral back pain patients with monosegmental degenerative disc disease. Br J Radiol 84:709–713. doi:10.1259/bjr/58136533
Claus AP, Hides JA, Moseley GL, Hodges PW (2009) Different ways to balance the spine: subtle changes in sagittal spinal curves affect regional muscle activity. Spine 34:E208–E214. doi:10.1097/BRS.0b013e3181908ead
Crawford RJ, Gizzi L, Ni Mhuiris Á, Falla D (2016) Are regions of the lumbar multifidus differentially activated during walking at varied speed and inclination? J Electromyogr Kinesiol 30:177–183
Lee HS, Shim JS, Lee ST, Kim M, Ryu JS (2014) Facilitating effects of fast and slope walking on paraspinal muscles. Ann Rehabil Med 38:514–522. doi:10.5535/arm.2014.38.4.514
MacDonald D, Moseley GL, Hodges PW (2009) Why do some patients keep hurting their back? Evidence of ongoing back muscle dysfunction during remission from recurrent back pain. Pain 142:183–188. doi:10.1016/j.pain.2008.12.002
Saunders SW, Rath D, Hodges PW (2004) Postural and respiratory activation of the trunk muscles changes with mode and speed of locomotion. Gait Posture 20:280–290. doi:10.1016/j.gaitpost.2003.10.003
Vos et al (2015) Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 385:117–171. doi:10.1016/s0140-6736(14)61682-2
Heymsfield SB, Adamek M, Gonzalez MC, Jia G, Thomas DM (2014) Assessing skeletal muscle mass: historical overview and state of the art. J Cachexia Sarcopenia Muscle 5:9–18. doi:10.1007/s13539-014-0130-5
Prado CM, Heymsfield SB (2014) Lean tissue imaging: a new era for nutritional assessment and intervention. JPEN J Parenter Enteral Nutr 38:940–953. doi:10.1177/0148607114550189
Acknowledgements
We would like to thank Dr. Seung Won Park as corresponding author for the Lee et al. [11] study for his helpful communications in providing sample sizes for each of their three age cohorts.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors RC and TV declare they have no conflicts of interest. Author JE is in receipt of an NIH research Grant (2014-19) for a cervical spine investigation, and provides consultation outside the submitted work as part-owner/investor in a medical consulting startup.
Funding
No funding was received for or in relation to this study.
Rights and permissions
About this article
Cite this article
Crawford, R.J., Elliott, J.M. & Volken, T. Change in fatty infiltration of lumbar multifidus, erector spinae, and psoas muscles in asymptomatic adults of Asian or Caucasian ethnicities. Eur Spine J 26, 3059–3067 (2017). https://doi.org/10.1007/s00586-017-5212-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-017-5212-6