Abstract
Purpose
This study aimed to investigate the changes of the posterior paraspinal muscles (PPM) and psoas muscle in patients with low back pain (LBP) over time.
Methods
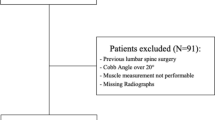
Patients with LBP who had a repeat lumbar MRI with a minimum of 3-years apart at a tertiary referral center were analyzed. MRI-based quantitative assessments of the PPM and the psoas muscle were conducted for the baseline and follow-up MRI. The cross sectional area (CSA), the functional cross sectional area (fCSA) and the fat area (FAT) were calculated using a dedicated software program. The fatty infiltration (FI,%) of the regions of interest was calculated. Differences between the 1st and 2nd MRI were calculated for all assessed muscular parameters.
Results
A total of 353 patients (54.4%female) with a median age of 60.1 years and BMI of 25.8 kg/m2 at baseline were analyzed. The mean time between the 1st and 2nd MRI was 3.6 years. The fCSAPPM declined in both sexes significantly from the 1st to the 2nd MRI, whereas the FATPPM increased. In line with this result, the FIPPM increased in both males (29.9%) and females (19.4%). Females had a higher FIPPM and FIPsoas than males in both MRIs. In females, no significant changes were found for the psoas muscle. The CSAPsoas and fCSAPsoas in males were significantly smaller in the 2nd MRI. With increasing age, a significant trend in a decrease in ∆FIPPM was observed for both sexes.
Conclusion
The study revealed significant quantitatively muscular changes in males and females, especially in the posterior paraspinal muscles in only three years’ time.


Similar content being viewed by others
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Shi L, Yan B, Jiao Y, Chen Z, Zheng Y, Lin Y et al (2022) Correlation between the fatty infiltration of paraspinal muscles and disc degeneration and the underlying mechanism. BMC Musculoskelet Disord 23(1):509
Lee ET, Lee SA, Soh Y, Yoo MC, Lee JH, Chon J (2021) Association of lumbar paraspinal muscle morphometry with degenerative spondylolisthesis. Int J Environ Res Public Health 18(8):4037
Thakar S, Sivaraju L, Aryan S, Mohan D, Sai Kiran NA, Hegde AS (2016) Lumbar paraspinal muscle morphometry and its correlations with demographic and radiological factors in adult isthmic spondylolisthesis: a retrospective review of 120 surgically managed cases. J Neurosurg Spine 24(5):679–685
Kang CH, Shin MJ, Kim SM, Lee SH, Lee CS (2007) MRI of paraspinal muscles in lumbar degenerative kyphosis patients and control patients with chronic low back pain. Clin Radiol 62(5):479–486
Wu A, March L, Zheng X, Huang J, Wang X, Zhao J et al (2020) Global low back pain prevalence and years lived with disability from 1990 to 2017: estimates from the global burden of disease study 2017. Ann Transl Med 8(6):299
Thiese MS, Hegmann KT, Wood EM, Garg A, Moore JS, Kapellusch J et al (2014) Prevalence of low back pain by anatomic location and intensity in an occupational population. BMC Musculoskelet Disord 15:283
Hoy D, Bain C, Williams G, March L, Brooks P, Blyth F et al (2012) A systematic review of the global prevalence of low back pain. Arthritis Rheum 64(6):2028–2037
Dagenais S, Caro J, Haldeman S (2008) A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J 8(1):8–20
Pai S, Sundaram LJ (2004) Low back pain: an economic assessment in the United States. Orthop Clin North Am 35(1):1–5
Knezevic NN, Candido KD, Vlaeyen JWS, Van Zundert J, Cohen SP (2021) Low back pain. Lancet 398(10294):78–92
Noonan AM, Brown SHM (2021) Paraspinal muscle pathophysiology associated with low back pain and spine degenerative disorders. JOR Spine 4(3):e1171
Ranger TA, Cicuttini FM, Jensen TS, Peiris WL, Hussain SM, Fairley J et al (2017) Are the size and composition of the paraspinal muscles associated with low back pain? A Syst Rev Spine J 17(11):1729–1748
Kalichman L, Carmeli E, Been E (2017) The association between imaging parameters of the paraspinal muscles, spinal degeneration, and low back pain. Biomed Res Int 2017:2562957
Kalichman L, Hodges P, Li L, Guermazi A, Hunter DJ (2010) Changes in paraspinal muscles and their association with low back pain and spinal degeneration: CT study. Eur Spine J 19(7):1136–1144
Teichtahl AJ, Urquhart DM, Wang Y, Wluka AE, Wijethilake P, O’Sullivan R et al (2015) Fat infiltration of paraspinal muscles is associated with low back pain, disability, and structural abnormalities in community-based adults. Spine J 15(7):1593–1601
Abbas J, Slon V, May H, Peled N, Hershkovitz I, Hamoud K (2016) Paraspinal muscles density: a marker for degenerative lumbar spinal stenosis? BMC Musculoskelet Disord 17(1):422
Zhu R, Niu WX, Zeng ZL, Tong JH, Zhen ZW, Zhou S et al (2017) The effects of muscle weakness on degenerative spondylolisthesis: a finite element study. Clin Biomech (Bristol, Avon) 41:34–38
Hori Y, Hoshino M, Inage K, Miyagi M, Takahashi S, Ohyama S et al (2019) ISSLS PRIZE IN CLINICAL SCIENCE 2019: clinical importance of trunk muscle mass for low back pain, spinal balance, and quality of life-a multicenter cross-sectional study. Eur Spine J 28(5):914–921
Muellner M, Haffer H, Moser M, Chiapparelli E, Dodo Y, Amini DA, Carrino JA, Tan ET, Shue J, Zhu J, Sama AA, Cammisa FP, Girardi FP, Hughes AP (2022) Paraspinal musculature impairment is associated with spinopelvic and spinal malalignment in patients undergoing lumbar fusion surgery. Spine J 22(12):2006–2016. https://doi.org/10.1016/j.spinee.2022.07.103
Stanuszek A, Jedrzejek A, Gancarczyk-Urlik E, Kolodziej I, Pisarska-Adamczyk M, Milczarek O et al (2022) Preoperative paraspinal and psoas major muscle atrophy and paraspinal muscle fatty degeneration as factors influencing the results of surgical treatment of lumbar disc disease. Arch Orthop Trauma Surg 142(7):1375–1384
Leng J, Han G, Zeng Y, Chen Z, Li W (2020) The effect of paraspinal muscle degeneration on distal pedicle screw loosening following corrective surgery for degenerative lumbar scoliosis. Spine 45(9):590–608
Kim JY, Ryu DS, Paik HK, Ahn SS, Kang MS, Kim KH et al (2016) Paraspinal muscle, facet joint, and disc problems: risk factors for adjacent segment degeneration after lumbar fusion. Spine J 16(7):867–875
Wang W, Sun Z, Li W, Chen Z (2020) The effect of paraspinal muscle on functional status and recovery in patients with lumbar spinal stenosis. J Orthop Surg Res 15(1):235
Dallaway A, Kite C, Griffen C, Duncan M, Tallis J, Renshaw D et al (2020) Age-related degeneration of the lumbar paravertebral muscles: Systematic review and three-level meta-regression. Exp Gerontol 133:110856
Marcus RL, Addison O, Kidde JP, Dibble LE, Lastayo PC (2010) Skeletal muscle fat infiltration: impact of age, inactivity, and exercise. J Nutr Health Aging 14(5):362–366
Dahlqvist JR, Vissing CR, Hedermann G, Thomsen C, Vissing J (2017) Fat replacement of paraspinal muscles with aging in healthy adults. Med Sci Sports Exerc 49(3):595–601
Muellner M, Chiapparelli E, Moser M, Haffer H, Dodo Y, Amini DA, Carrino JA, Tan ET, Shue J, Zhu J, Sama AA, Cammisa FP, Girardi FP, Hughes AP (2022) The effect of age on psoas and paraspinal muscle morphology in patients undergoing posterior lumbar fusion surgery. Eur Spine J 31(10):2619–2628. https://doi.org/10.1007/s00586-022-07346-0
Crawford RJ, Filli L, Elliott JM, Nanz D, Fischer MA, Marcon M et al (2016) Age- and level-dependence of fatty infiltration in lumbar paravertebral muscles of healthy volunteers. AJNR Am J Neuroradiol 37(4):742–748
Faron A, Luetkens JA, Schmeel FC, Kuetting DLR, Thomas D, Sprinkart AM (2019) Quantification of fat and skeletal muscle tissue at abdominal computed tomography: associations between single-slice measurements and total compartment volumes. Abdom Radiol (NY) 44(5):1907–1916
Yushkevich PA, Piven J, Hazlett HC, Smith RG, Ho S, Gee JC et al (2006) User-guided 3D active contour segmentation of anatomical structures: significantly improved efficiency and reliability. Neuroimage 31(3):1116–1128
Moser M, Amini DA, Jones C, Zhu J, Okano I, Oezel L, Chiapparelli E, Tan ET, Shue J, Sama AA, Cammisa FP, Girardi FP, Hughes AP (2023) The predictive value of psoas and paraspinal muscle parameters measured on MRI for severe cage subsidence after standalone lateral lumbar interbody fusion. Spine J 23(1):42–53. https://doi.org/10.1016/j.spinee.2022.03.009
Ding JZ, Kong C, Li XY, Sun XY, Lu SB, Zhao GG (2022) Different degeneration patterns of paraspinal muscles in degenerative lumbar diseases: a MRI analysis of 154 patients. Eur Spine J 31(3):764–773
Hamrick MW, McGee-Lawrence ME, Frechette DM (2016) Fatty infiltration of skeletal muscle: mechanisms and comparisons with bone marrow adiposity. Front Endocrinol (Lausanne) 7:69
Talbot J, Maves L (2016) Skeletal muscle fiber type: using insights from muscle developmental biology to dissect targets for susceptibility and resistance to muscle disease. Wiley Interdiscip Rev Dev Biol 5(4):518–534
Fortin M, Videman T, Gibbons LE, Battie MC (2014) Paraspinal muscle morphology and composition: a 15-yr longitudinal magnetic resonance imaging study. Med Sci Sports Exerc 46(5):893–901
Murata Y, Nakamura E, Tsukamoto M, Nakagawa T, Takeda M, Kozuma M et al (2021) Longitudinal study of risk factors for decreased cross-sectional area of psoas major and paraspinal muscle in 1849 individuals. Sci Rep 11(1):16986
Ranger TA, Cicuttini FM, Jensen TS, Heritier S, Urquhart DM (2019) Paraspinal muscle cross-sectional area predicts low back disability but not pain intensity. Spine J 19(5):862–868
Hebert JJ, Kjaer P, Fritz JM, Walker BF (2014) The relationship of lumbar multifidus muscle morphology to previous, current, and future low back pain: a 9-year population-based prospective cohort study. Spine 39(17):1417–1425. https://doi.org/10.1097/BRS.0000000000000424
Maki T, Oura P, Paananen M, Niinimaki J, Karppinen J, Junno JA (2019) Longitudinal analysis of paraspinal muscle cross-sectional area during early adulthood—A 10-year follow-up MRI study. Sci Rep 9(1):19497
Sakuma K, Yamaguchi A (2012) Sarcopenia and age-related endocrine function. Int J Endocrinol 2012:127362
Gorgey AS, Dudley GA (2007) Skeletal muscle atrophy and increased intramuscular fat after incomplete spinal cord injury. Spinal Cord 45(4):304–309
Kim HM, Galatz LM, Lim C, Havlioglu N, Thomopoulos S (2012) The effect of tear size and nerve injury on rotator cuff muscle fatty degeneration in a rodent animal model. J Shoulder Elbow Surg 21(7):847–858
Morrissey MC (1989) Reflex inhibition of thigh muscles in knee injury causes and treatment. Sports Med 7(4):263–276
Zedka M, Prochazka A, Knight B, Gillard D, Gauthier M (1999) Voluntary and reflex control of human back muscles during induced pain. J Physiol 520(Pt 2):591–604
Macefield VG (2009) Long Loop Reflexes. In: Binder MD, Hirokawa N, Windhorst U (eds). Encyclopedia of Neuroscience. Springer, Berlin Heidelberg, pp 2180–2183
Hides JA, Stokes MJ, Saide M, Jull GA, Cooper DH (1994) Evidence of lumbar multifidus muscle wasting ipsilateral to symptoms in patients with acute/subacute low back pain. Spine 19(Supplement):165–172. https://doi.org/10.1097/00007632-199401001-00009
Danneels LA, Vanderstraeten GG, Cambier DC, Witvrouw EE, De Cuyper HJ (2000) CT imaging of trunk muscles in chronic low back pain patients and healthy control subjects. Eur Spine J 9(4):266–272
James G, Chen X, Diwan A, Hodges PW (2021) Fat infiltration in the multifidus muscle is related to inflammatory cytokine expression in the muscle and epidural adipose tissue in individuals undergoing surgery for intervertebral disc herniation. Eur Spine J 30(4):837–845
Hamrick MW (2017) Role of the cytokine-like hormone leptin in muscle-bone crosstalk with aging. J Bone Metab 24(1):1–8
Klyne DM, Barbe MF, van den Hoorn W, Hodges PW (2018) ISSLS PRIZE IN CLINICAL SCIENCE 2018: longitudinal analysis of inflammatory, psychological, and sleep-related factors following an acute low back pain episode-the good, the bad, and the ugly. Eur Spine J 27(4):763–777
Funding
No funds, grants, or other support was received for the submitted work.
Author information
Authors and Affiliations
Contributions
Conception and design contributed by M. Acquisition of data contributed by M, H, M, C, D. Analysis and interpretation of data contributed by M, H, H, M. Drafting the article was contributed by M. Critically revising the article was contributed by all authors. Preparation of Graphical Content was contributed by M, H. Reviewed submitted version of manuscript was contributed by all authors. Approved the final version of the manuscript on behalf of all authors was contributed by H. Statistical analysis contributed by M, Z. Administrative/technical/material support contributed by T, S. Study Supervision contributed by H.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Sama reports royalties from Ortho Development, Corp.; private investments for Vestia Ventures MiRUS Investment, LLC, IVY II, LLC, ISPH 3, LLC, and VBros Venture Partners X Centinel Spine; consulting fee from Clariance, Inc., Kuros Biosciences AG, and Medical Device Business Service, Inc.; speaking and teaching arrangements of DePuy Synthes Products, Inc.; membership of scientific advisory board of Clariance, Inc., and Kuros Biosciences AG; and trips/travel of Medical Device Business research support from Spinal Kinetics, Inc., outside the submitted work. Dr. Cammisa reports royalties from NuVasive, Inc. Accelus; private investments for 4WEB Medical/4WEB, Inc., Bonovo Orthopedics, Inc., Healthpoint Capital Partners, LP, ISPH II, LLC, ISPH 3 Holdings, LLC, Ivy Healthcare Capital Partners, LLC, Medical Device Partners II, LLC, Medical Device Partners III, LLC, Orthobond Corporation, Spine Biopharma, LLC, Synexis, LLC, Tissue Differentiation Intelligence, LLC, VBVP VI, LLC, VBVP X, LLC (Centinel) and Woven Orthopedics Technologies; consulting fees from 4WEB Medical/4WEB, Inc., DePuy Synthes Spine, NuVasive, Inc., Spine Biopharma, LLC, and Synexis, LLC, Accelus; membership of scientific advisory board/other office of Healthpoint Capital Partners, LPIVY, Medical Device Partners III, LLC, Orthobond Corporation, Spine Biopharma, LLC, Synexis, LLC, and Woven Orthopedic Technologies; and research support from 4WEB Medical/4WEB, Inc., Mallinckrodt Pharmaceuticals, Camber Spine, and Centinel Spine, outside the submitted work. Dr. Girardi reports royalties from Lanx, Inc., and Ortho Development Corp.; private investments for Centinel Spine, and BCMID; stock ownership of Healthpoint Capital Partners, LP; and consulting fees from NuVasive, Inc., and DePuy Synthes Spine, outside the submitted work. Dr. Hughes reports research support from NuVasive, Inc. and Kuros Biosciences AG; and fellowship support from NuVasive, Inc. and Kuros Biosciences AG, outside the submitted work.
Ethical approval
The investigation was approved by the institutional review board. IRB approval: Hospital for Special Surgery #2019-2137.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The work was performed at the Hospital for Special Surgery, New York City, NY, USA. The institutional review board of the Hospital for Special Surgery approved this study.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Muellner, M., Haffer, H., Moser, M. et al. Changes of the posterior paraspinal and psoas muscle in patients with low back pain: a 3-year longitudinal study. Eur Spine J 32, 3290–3299 (2023). https://doi.org/10.1007/s00586-023-07814-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07814-1