Abstract
Purpose
Moderate-to-vigorous physical activity (MVPA) can improve the quality of life (QoL) for breast cancer survivors (BCS), yet, most do not achieve 150 + weekly minutes of MVPA. This study investigated moderators of response to a physical activity (PA) behavior change intervention for BCS.
Methods
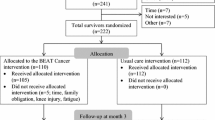
BCS (N = 222) were randomized to the 3-month intervention (BEAT Cancer) or usual care. Measurements occurred at baseline, post-intervention, and 3 months post-intervention. Measures included accelerometry, self-reported MVPA, and Functional Assessment of Cancer Therapy (FACT-General, FACT-Breast, physical well-being (PWB), social well-being (SWB), emotional well-being (EWB), functional well-being (FWB), additional concerns (AC), and Trial Outcome Index (TOI)).
Results
Adjusted linear mixed-model analyses indicated individuals ≤ 24 months post-diagnosis and who were single reported smaller increases in weekly self-reported MVPA than those > 24 months (44.07 vs 111.93) and partnered (− 16.24 vs. 49.16 min), all p < 0.05. As for QoL, participants < 12 months post-diagnosis who received chemotherapy experienced smaller improvements than those ≥ 12 months in FACT-General, FACT-Breast, PWB, and SWB scores. Survivors with a history of chemotherapy had smaller improvements in FACT-General, FACT-Breast, PWB, SWB, TOI, and AC scores, all p < 0.05.
Conclusion
These findings indicate that being < 2 years post-diagnosis, single, and prior chemotherapy may limit MVPA and QOL responses to a PA intervention. Further studies are needed to determine if and/or what additional PA supports and resources these subgroups of BCS might find beneficial and effective.
Trial registration
ClinicalTrials.gov number: NCT00929617.






Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon request.
Abbreviations
- QoL:
-
Quality of life
- BCS:
-
Breast cancer survivor
- PA:
-
Physical activity
- PWB:
-
Physical well-being
- SWB:
-
Social well-being
- EWB:
-
Emotional well-being
- FWB:
-
Functional well-being
- AC:
-
Additional concerns
- TOI:
-
Trial outcome index
- BMI:
-
Body mass index
- BEAT Cancer:
-
Better exercise adherence after treatment for cancer
- IRB:
-
Institutional review board
- UC:
-
Usual care
- MVPA:
-
Moderate-to-vigorous physical activity
- WOMAC:
-
Western Ontario and McMaster Universities Osteoarthritis
- FACT-Breast:
-
Functional Assessment of Cancer Therapy-Breast
- FACT-G:
-
Functional Assessment of Cancer Therapy-General
- RUCC:
-
Agriculture Rural–Urban Continuum Codes
References
Siegel RL, Miller KD, Fuchs HE, Jemal A (2022) “Cancer statistics, 2022”, (in eng). CA Cancer J Clin 72(1):7–33. https://doi.org/10.3322/caac.21708
Bower JE, Wiley J, Petersen L, Irwin MR, Cole SW, Ganz PA (2018) “Fatigue after breast cancer treatment: biobehavioral predictors of fatigue trajectories”, (in eng). Health Psychol 37(11):1025–1034. https://doi.org/10.1037/hea0000652
Hamer J et al (2017) Quality of life (QOL) and symptom burden (SB) in patients with breast cancer. Support Care Cancer 25(2):409–419. https://doi.org/10.1007/s00520-016-3417-6
Joly F, Lange M, Dos Santos M, Vaz-Luis I and Di Meglio A (2019) “Long-term fatigue and cognitive disorders in breast cancer survivors,” Cancers (Basel), 11(12) https://doi.org/10.3390/cancers11121896
Sabiston CM, Lacombe J, Faulkner G, Jones J, Trinh L (2018) Profiling sedentary behavior in breast cancer survivors: links with depression symptoms during the early survivorship period. Psychooncology 27(2):569–575. https://doi.org/10.1002/pon.4520
Caspersen CJ, Powell KE, Christenson GM (1985) “Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research”, (in eng). Public Health Rep 100(2):126–31
Campbell KL et al (2019) Exercise guidelines for cancer survivors: consensus statement from International Multidisciplinary Roundtable. Med Sci Sports Exerc 51(11):2375–2390. https://doi.org/10.1249/MSS.0000000000002116
Cormie P, Zopf EM, Zhang X, Schmitz KH (2017) The impact of exercise on cancer mortality, recurrence, and treatment-related adverse effects. Epidemiol Rev 39(1):71–92. https://doi.org/10.1093/epirev/mxx007
Hong F, Ye W, Kuo CH, Zhang Y, Qian Y, Korivi M (2019) “Exercise intervention improves clinical outcomes, but the “time of session” is crucial for better quality of life in breast cancer survivors: a systematic review and meta-analysis,” (in eng), Cancers (Basel), 11(5), https://doi.org/10.3390/cancers11050706
Mishra SI et al (2012) “Exercise interventions on health-related quality of life for cancer survivors”, (in eng). Cochrane Database Syst Rev 2012(8):Cd007566. https://doi.org/10.1002/14651858.CD007566.pub2
Rogers LQ et al (2015) Effects of the BEAT Cancer physical activity behavior change intervention on physical activity, aerobic fitness, and quality of life in breast cancer survivors: a multicenter randomized controlled trial. Breast Cancer Res Treat 149(1):109–119. https://doi.org/10.1007/s10549-014-3216-z
Rogers LQ et al (2016) Effects of a multicomponent physical activity behavior change intervention on breast cancer survivor health status outcomes in a randomized controlled trial. Breast Cancer Res Treat 159(2):283–291. https://doi.org/10.1007/s10549-016-3945-2
Gavin KL et al (2019) Sedentary behavior after breast cancer: motivational, demographic, disease, and health status correlates of sitting time in breast cancer survivors. Cancer Causes Control 30(6):569–580. https://doi.org/10.1007/s10552-019-01153-7
Phillips SM, Dodd KW, Steeves J, McClain J, Alfano CM, McAuley E (2015) Physical activity and sedentary behavior in breast cancer survivors: new insight into activity patterns and potential intervention targets. Gynecol Oncol 138(2):398–404. https://doi.org/10.1016/j.ygyno.2015.05.026
Buffart LM et al (2017) Effects and moderators of exercise on quality of life and physical function in patients with cancer: an individual patient data meta-analysis of 34 RCTs. Cancer Treat Rev 52:91–104. https://doi.org/10.1016/j.ctrv.2016.11.010
Buffart LM et al (2015) The effect, moderators, and mediators of resistance and aerobic exercise on health-related quality of life in older long-term survivors of prostate cancer. Cancer 121(16):2821–2830. https://doi.org/10.1002/cncr.29406
Courneya KS et al (2008) Moderators of the effects of exercise training in breast cancer patients receiving chemotherapy: a randomized controlled trial. Cancer 112(8):1845–1853. https://doi.org/10.1002/cncr.23379
Courneya KS et al (2009) Moderator effects in a randomized controlled trial of exercise training in lymphoma patients. Cancer Epidemiol Biomarkers Prev 18(10):2600–2607. https://doi.org/10.1158/1055-9965.EPI-09-0504
Griffith K, Wenzel J, Shang J, Thompson C, Stewart K, Mock V (2009) Impact of a walking intervention on cardiorespiratory fitness, self-reported physical function, and pain in patients undergoing treatment for solid tumors. Cancer 115(20):4874–4884. https://doi.org/10.1002/cncr.24551
Kalter J et al (2015) Moderators of the effects of group-based physical exercise on cancer survivors’ quality of life. Support Care Cancer 23(9):2623–2631. https://doi.org/10.1007/s00520-015-2622-z
Pinto B, Stein K, Dunsiger S (2015) Peer mentorship to promote physical activity among cancer survivors: effects on quality of life. Psychooncology 24(10):1295–1302. https://doi.org/10.1002/pon.3884
Speck RM et al (2010) Changes in the body image and relationship scale following a one-year strength training trial for breast cancer survivors with or at risk for lymphedema. Breast Cancer Res Treat 121(2):421–430. https://doi.org/10.1007/s10549-009-0550-7
Steindorf K et al (2014) Randomized, controlled trial of resistance training in breast cancer patients receiving adjuvant radiotherapy: results on cancer-related fatigue and quality of life. Ann Oncol 25(11):2237–2243. https://doi.org/10.1093/annonc/mdu374
Gudina AT et al (2021) “Health related quality of life in adult cancer survivors: importance of social and emotional support”, (in eng). Cancer Epidemiol 74:101996. https://doi.org/10.1016/j.canep.2021.101996
Mama SK, Bhuiyan N, Smyth JM, Schmitz KH (2020) Stress and physical activity in rural cancer survivors: the moderating role of social support. J Rural Health 36(4):543–548. https://doi.org/10.1111/jrh.12455
McDonough MH et al (2021) “Social support and physical activity for cancer survivors: a qualitative review and meta-study”, (in eng). J Cancer Surviv 15(5):713–728. https://doi.org/10.1007/s11764-020-00963-y
Pekmezi D, Martin MY, Kvale E, Meneses K, Demark-Wahnefried W (2012) “Enhancing exercise adherence for the breast cancer survivors”, (in eng). ACSMs Health Fit J 16(4):8–13. https://doi.org/10.1249/FIT.0b013e31825a6db6
Pruitt SL, McQueen A, Deshpande AD, Jeffe DB, Schootman M (2012) “Mediators of the effect of neighborhood poverty on physical functioning among breast cancer survivors: a longitudinal study”, (in eng). Cancer Causes Control 23(9):1529–1540. https://doi.org/10.1007/s10552-012-0030-y
Pekmezi D et al (2013) “Developing an intervention to address physical activity barriers for African-American women in the deep south (USA)”, (in eng). Womens Health (Lond) 9(3):301–312. https://doi.org/10.2217/whe.13.20
Rogers LQ et al (2012) Better exercise adherence after treatment for cancer (BEAT Cancer) study: rationale, design, and methods. Contemp Clin Trials 33(1):124–137. https://doi.org/10.1016/j.cct.2011.09.004
Freedson PS, Melanson E, Sirard J (1998) “Calibration of the Computer Science and Applications, Inc. accelerometer”, (in eng). Med Sci Sports Exerc 30(5):777–81. https://doi.org/10.1097/00005768-199805000-00021
Sirard JR, Melanson EL, Li L, Freedson PS (2000) Field evaluation of the Computer Science and Applications, Inc. physical activity monitor. Med Sci Sports Exerc 32(3):695–700. https://doi.org/10.1097/00005768-200003000-00022
Godin G, Jobin J, Bouillon J (1986) Assessment of leisure time exercise behavior by self-report: a concurrent validity study. Can J Public Health 77(5):359–62 [Online]. Available: https://www.ncbi.nlm.nih.gov/pubmed/3791117. Accessed 21 Apr 2021
Godin G, Shephard RJ (1985) “A simple method to assess exercise behavior in the community”, (in eng). Can J Appl Sport Sci. Journal canadien des sciences appliquees au sport 10(3):141–146
U. S. D. o. Health and S. Human (2008) Physical activity guidelines for Americans: be active, healthy, and happy! http://www.health.gov/paguidelines/guidelines/default.aspx, [Online]. Available: https://cir.nii.ac.jp/crid/1571417124999913088. Accessed 21 Apr 2021
Smith WJ et al (2021) Promoting physical activity in rural settings: effectiveness and potential strategies. Transl J Am Coll Sports Med 6(4):e000180. https://doi.org/10.1249/tjx.0000000000000180
Brady MJ et al (1997) Reliability and validity of the Functional Assessment of Cancer Therapy-Breast quality-of-life instrument. J Clin Oncol 15(3):974–986. https://doi.org/10.1200/JCO.1997.15.3.974
Cella DF et al (1993) The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. J Clin Oncol 11(3):570–579. https://doi.org/10.1200/JCO.1993.11.3.570
Niravath P (2013) Aromatase inhibitor-induced arthralgia: a review. Ann Oncol 24(6):1443–1449. https://doi.org/10.1093/annonc/mdt037
U. S. D. o. Agriculture and E. R. Service. Rural-urban continuum code [Online]. Available: https://www.ers.usda.gov/data-products/rural-urban-continuum-codes/. Accessed 21 Apr 2021
Groll DL, To T, Bombardier C, Wright JG (2005) The development of a comorbidity index with physical function as the outcome. J Clin Epidemiol 58(6):595–602. https://doi.org/10.1016/j.jclinepi.2004.10.018
Rogers JC et al (2003) Concordance of four methods of disability assessment using performance in the home as the criterion method. Arthritis Rheum 49(5):640–647. https://doi.org/10.1002/art.11379
Weir CB, Jan A (2022) BMI classification percentile and cut off points. In: StatPearls [Internet]. StatPearls Publishing, Treasure Island. Accessed 10 Oct 2022
Yost KJ, Eton DT (2005) Combining distribution- and anchor-based approaches to determine minimally important differences: the FACIT experience. Eval Health Prof 28(2):172–191. https://doi.org/10.1177/0163278705275340
Milne HM, Wallman KE, Gordon S, Courneya KS (2008) Effects of a combined aerobic and resistance exercise program in breast cancer survivors: a randomized controlled trial. Breast Cancer Res Treat 108(2):279–288. https://doi.org/10.1007/s10549-007-9602-z
Courneya KS (2010) Efficacy, effectiveness, and behavior change trials in exercise research. Int J Behav Nutr Phys Act 7:81. https://doi.org/10.1186/1479-5868-7-81
McDonough MH et al (2019) “The role of social support in physical activity for cancer survivors: a systematic review”, (in eng). Psychooncology 28(10):1945–1958. https://doi.org/10.1002/pon.5171
Russo S et al (2014) Factors affecting patient’s perception of anticancer treatments side-effects: an observational study. Expert Opin Drug Saf 13(2):139–150. https://doi.org/10.1517/14740338.2013.830710
Jansen SJ, Otten W, van de Velde CJ, Nortier JW, Stiggelbout AM (2004) The impact of the perception of treatment choice on satisfaction with treatment, experienced chemotherapy burden and current quality of life. Br J Cancer 91(1):56–61. https://doi.org/10.1038/sj.bjc.6601903
Silva SM, Moreira HC, Canavarro MC (2012) “Examining the links between perceived impact of breast cancer and psychosocial adjustment: the buffering role of posttraumatic growth”, (in eng). Psychooncology 21(4):409–418. https://doi.org/10.1002/pon.1913
Buffart LM, Galvao DA, Brug J, Chinapaw MJ, Newton RU (2014) Evidence-based physical activity guidelines for cancer survivors: current guidelines, knowledge gaps and future research directions. Cancer Treat Rev 40(2):327–340. https://doi.org/10.1016/j.ctrv.2013.06.007
Kaminsky LA, Ozemek C (2012) “A comparison of the Actigraph GT1M and GT3X accelerometers under standardized and free-living conditions”, (in eng). Physiol Meas 33(11):1869–1876. https://doi.org/10.1088/0967-3334/33/11/1869
Vanhelst J et al (2012) “Comparison of two ActiGraph accelerometer generations in the assessment of physical activity in free living conditions”, (in eng). BMC Res Notes 5:187. https://doi.org/10.1186/1756-0500-5-187
Williams VA et al. (2021) “A web-based lifestyle intervention for cancer survivors: feasibility and acceptability of SurvivorSHINE,” (in eng), J Cancer Educ, https://doi.org/10.1007/s13187-021-02026-x
Houghton LC et al (2021) “Free time for wellness: a co-designed intervention utilizing social networks to encourage physical activity for cancer prevention among low resourced mothers”, (in eng). BMC Public Health 21(1):1805. https://doi.org/10.1186/s12889-021-11775-9
Key KV, Adegboyega A, Bush H, Aleshire ME, Contreras OA, Hatcher J (2020) “#CRCFREE: using social media to reduce colorectal cancer risk in rural adults”, (in eng). Am J Health Behav 44(3):353–363. https://doi.org/10.5993/ajhb.44.3.8
Pope Z, Lee JE, Zeng N, Lee HY, Gao Z (2019) “Feasibility of smartphone application and social media intervention on breast cancer survivors’ health outcomes”, (in eng). Transl Behav Med 9(1):11–22. https://doi.org/10.1093/tbm/iby002
Adams JL et al (2021) “Determining patient needs to enhance exercise program implementation and uptake in rural settings for women after a cancer diagnosis”, (in eng). Support Care Cancer 29(8):4641–4649. https://doi.org/10.1007/s00520-021-05990-8
Schmitz KH, Speck RM (2010) “Risks and benefits of physical activity among breast cancer survivors who have completed treatment”, (in eng). Womens Health (Lond) 6(2):221–238. https://doi.org/10.2217/whe.10.1
Acknowledgements
The authors are exceptionally grateful for the efforts of the 222 survivors of breast cancer who participated in this study.
Funding
This research was supported by National Institutes of Health grants (grant numbers R01CA136859, P30DK056336, R25CA47888, and CA047888).
Author information
Authors and Affiliations
Contributions
Edward McAuley, Kerry S Courneya, Phillip Anton, Diane K. Ehlers, Siobhan M. Phillips, and Laura Q Rogers contributed to the study conception, design, material preparation, and data collection. Statistical analyses were conducted by Robert Oster, Laura Q Rogers, and Erica Schleicher. Erica Schleicher wrote the manuscript and all co-authors reviewed and revised. Final approval was given by all authors before submitting for publication.
Corresponding author
Ethics declarations
Ethics approval and consent
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of the University of Alabama at Birmingham (June 2009). Institutional review board (IRB) approval was obtained.
Consent to participate
All participants provided written informed consent to participant in this study.
Consent for publication
The authors affirm that human research participants provided informed consent for publication of their data.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Schleicher, E., McAuley, E., Courneya, K.S. et al. Moderators of physical activity and quality of life response to a physical activity intervention for breast cancer survivors. Support Care Cancer 31, 53 (2023). https://doi.org/10.1007/s00520-022-07477-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-022-07477-6