Abstract
Purposes
The purposes of this discrete choice experiment are as follows: (1) to investigate the preferences of gastric cancer survivors for follow-up care, and (2) to quantify the importance of follow-up care–related characteristics that may affect the gastric cancer survivors’ choices of their follow-up, so as to provide references for the development of the follow-up strategy of gastric cancer survivors.
Methods
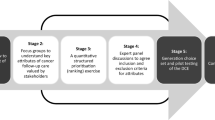
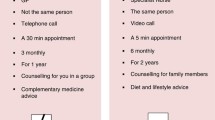
Discrete choice experimental design principle was applied to develop the survey instrument. All questionnaires were filled out by the respondents and collected on site. A mixed logit model was used to estimate gastric cancer survivors’ preferences. Willingness to pay estimates and simulations of follow-up uptake rates were calculated.
Results
All six attributes are significantly important for the follow-up care of gastric cancer survivors (p < 0.05). Achieving very thorough follow-up contents was the most valued attribute level (coefficient = 1.995). Specialist doctors are the most preferred providers followed by specialist nurses, and gastric cancer survivors were willing to pay more for these attribute levels. Changes in attribute levels affected uptake rate of follow-up. When the multiple attribute levels were changed at the same time, a very thorough follow-up content was provided by the same specialist doctor (specialist nurse), and the probability of receiving follow-up increases by 95.82% (94.90%).
Conclusions
The characteristics of follow-up care in our study reflect the health management services’ expectations of gastric cancer survivors. A dedicated specialist nurse involved in follow-up care should be developed to contribute to solve the complex and multifaceted personal needs of gastric cancer survivors.

Similar content being viewed by others
Data availability
The data used to support the findings of this study are included within the article, and all data included in this study are available upon request by contact with the corresponding authors.
References
Ferro A, Peleteiro B, Malvezzi M, Bosetti CBP, Levi FNE, La Vecchia C, Lunet N (2014) Worldwide trends in gastric cancer mortality (1980–2011), with predictions to 2015, and incidence by subtype. Eur J Cancer 50(7):1330–1344. https://doi.org/10.1016/j.ejca.2014.01.029
Bray F, Ferlay J, Soerjomataram I, Siegel R, Torre L (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424. https://doi.org/10.3322/caac.21492
Jemal A, Thomas MA, Murray MT (2002) Thun DM (2002) Cancer Statistics. CA Cancer J Clin 52(1):23–47
Jin H, Pinheiro P, Callahan K, Altekruse S (2017) Examining the gastric cancer survival gap between Asians and whites in the United States. Gastric cancer: official journal of the International Gastric Cancer Association and the Japanese Gastric Cancer Association 20(4):573–582. https://doi.org/10.1007/s10120-016-0667-4
Dirven L, van de Poll-Franse L, Aaronson N, Reijneveld J (2015) Controversies in defining cancer survivorship. Lancet Oncol 16(6):610–612. https://doi.org/10.1016/s1470-2045(15)70236-6
Moser E, Meunier F (2014) Cancer survivorship: a positive side-effect of more successful cancer treatment. EJC Suppl 12(1):1–4. https://doi.org/10.1016/j.ejcsup.2014.03.001
Su M, Hua X, Wang J, Yao N, Zhao D, Liu W, Zou Y, Anderson R, Sun X (2018) Health-related quality of life among cancer survivors in rural China. Qual Life Res 28(3):695–702
Kong H, Kwon OK, Yu W (2012) Changes of quality of life after gastric cancer surgery. Journal of gastric cancer 12(3):194–200
Jentschura D, Winkler M, Strohmeier N, Rumstadt B, Hagmüller E (1997) Quality-of-life after curative surgery for gastric cancer: a comparison between total gastrectomy and subtotal gastric resection. HEPATO-GASTROENTEROL 44(16):1137–1142
Bang WE, Ryu KW, Lee JH, Choi IJ, Kook MC, Cho SJ, Lee JY, Kim CG, Park SR, Lee JS (2011) Oncologic effectiveness of regular follow-up to detect recurrence after curative resection of gastric cancer. Ann Surg Oncol 18(2):358–364
Tan IT, So BYJ (2010) Value of intensive follow-up of patients after curative surgery for gastric carcinoma. J Surg Oncol 96(6):503–506
Nilsson, Cancer MJG (2017) Postgastrectomy follow-up in the West: evidence base, guidelines, and daily practice. Gastric Cancer 20(1 Supplement):135–140
Heneghan HM, Zaborowski A, Fanning M, Mchugh A, Reynolds JVJAoS (2015) Prospective study of malabsorption and malnutrition after esophageal and gastric cancer surgery. Ann Surg 262(5):803–808
Nilsson, Cancer MJG (2017) Postgastrectomy follow-up in the West: evidence base, guidelines, and daily practice. Gastric Cancer 20(1):135–140
Jeon BH, Choi M, Lee JH, Noh SHJN, Sciences H (2016) Relationships between gastrointestinal symptoms, uncertainty, and perceived recovery in patients with gastric cancer after gastrectomy. Nurs Health Sci 18(1):23–29
Hu J-K, Chen X-Z, Zhang W-H (2014) Follow-up strategies for postoperative patients with gastric cancer. Chinese Journal of Practical Surgery 34(07):669–671. https://doi.org/10.7504/CJPS
Li J-p, Zhou ZP, Wei QF (2020) Study on the status quo and intervention of the patients’ unmet needs after gastric cancer operation. J Nurs Manag 20(12):882–885+890
Jian-kun H, Xin-zu C, Wei-han Z (2014) Follow-up strategy for postoperative gastric cancer patients. Chinese Journal of Practical Surgery 34(07):669–671
Gu J (2020) Study on the effectiveness and management measures of follow-up after discharge from the oncology department. Journal of Traditional Chinese Medicine Management 28(09):159–160
Zhang-jun H (2020) Analyzing the clinical efficacy of laparoscopic surgery for advanced distal gastric cancer and the impact of patient follow-up on the quality of life. Systems Medicine 5(17):84–86
Jian-kun H, Lin-yong Z, Xin-zu C (2015) Follow-up and monitoring of postoperative recurrence and metastasis of gastric cancer. Chinese Journal of Practical Surgery 35(10):1082–1085
Marcial LH, Richardson JE, Lasater B, Middleton B, Osheroff JA, Kawamoto K, Ancker JS, Leeuwen DV, Lomotan EA, Al-Showk S (2018) The imperative for patient-centered clinical decision support. EGEMS (Wash DC) 6(1):12–12. https://doi.org/10.5334/egems.259
Richardson J, Middleton B, Platt J, Blumenfeld B (2020) Building and maintaining trust in clinical decision support: recommendations from the Patient-Centered CDS Learning Network. J Learning health systems 4(2):e10208. https://doi.org/10.1002/lrh2.10208
Lancsar E, Louviere J (2008) Conducting discrete choice experiments to inform healthcare decision making. Pharmacoeconomics 26(8):661–677. https://doi.org/10.2165/00019053-200826080-00004
de Bekker-Grob E, Ryan M, Gerard K (2012) Discrete choice experiments in health economics: a review of the literature. Health Econ 21(2):145–172. https://doi.org/10.1002/hec.1697
Clark M, Determann D, Petrou S, Moro D, de Bekker-Grob E (2014) Discrete choice experiments in health economics: a review of the literature. Pharmacoeconomics 32(9):883–902. https://doi.org/10.1007/s40273-014-0170-x
Lancsar E, Louviere J (2008) Conducting discrete choice experiments to inform healthcare decision making: a user’s guide. Pharmacoeconomics 26(8):661–677. https://doi.org/10.2165/00019053-200826080-00004
Bridges JFPP, Hauber ABP, Marshall DP, Lloyd AD, Prosser LAP, Regier DAP, Johnson FRP, Mauskopf JP (2011) Conjoint analysis applications in health—a checklist: a report of the ISPOR Good Research Practices for Conjoint Analysis Task Force. Value in Health 14(4):403–413. https://doi.org/10.1016/j.jval.2010.11.013
Trapero-Bertran M, Rodríguez-Martín B, López-Bastida J (2019) What attributes should be included in a discrete choice experiment related to health technologies? A systematic literature review. PLOS ONE 14(1):12–19
Burgess L, Street DJJS (n.d.) The optimal size of choice sets in choice experiments.(Berlin, DDR) 40(6):507–515
Bessen T, Chen G, Street J, Eliott J, Karnon J, Keefe D, Ratcliffe J (2014) What sort of follow-up services would Australian breast cancer survivors prefer if we could no longer offer long-term specialist-based care? A discrete choice experiment. Br J Cancer 110(4):859–867. https://doi.org/10.1038/bjc.2013.800
Murchie P, Norwood P, Pietrucin-Materek M, Porteous T, Hannaford P, Ryan M (2016) Determining cancer survivors’ preferences to inform new models of follow-up care. BMJ 115(12):1495–1503. https://doi.org/10.1038/bjc.2016.352
Faller H, Schuler M, Richard M, Heckl U, Weis J, Küffner R (2013) Effects of psycho-oncologic interventions on emotional distress and quality of life in adult patients with cancer: systematic review and meta-analysis. J Clin Oncol 31(6):782–793. https://doi.org/10.1200/jco.2011.40.8922
Stagl J, Lechner S, Carver C, Bouchard L, Gudenkauf L, Jutagir D, Diaz A, Yu Q, Blomberg B, Ironson G, Glück S, Antoni M (2015) A randomized controlled trial of cognitive-behavioral stress management in breast cancer: survival and recurrence at 11-year follow-up. Breast Cancer Res Treat 154(2):319–328. https://doi.org/10.1007/s10549-015-3626-6
Cox A, Lucas G, Marcu A, Piano M, Grosvenor W, Mold F, Maguire R, Ream E (2017) Cancer survivors’ experience with telehealth: a systematic review and thematic synthesis. J Med Internet Res 19(1):e11. https://doi.org/10.2196/jmir.6575
Burnette C, Roh S, Liddell J, Lee Y (2019) American Indian women cancer survivor’s needs and preferences: community support for cancer experiences. J Cancer Educ 34(3):592–599. https://doi.org/10.1007/s13187-018-1346-4
Arch J, Vanderkruik R, Kirk A, Carr A (2018) A closer lens: cancer survivors’ supportive intervention preferences and interventions received. Psychooncology 27(5):1434–1441. https://doi.org/10.1002/pon.4526
McMullen C, Bulkley J, Altschuler A, Wendel C, Grant M, Hornbrook M, Sun V, Krouse R (2016) Greatest challenges of rectal cancer survivors: results of a population-based survey. Diseases of the colon rectum 59(11):1019–1027. https://doi.org/10.1097/dcr.0000000000000695
Smith T, Strollo S, Hu X, Earle C, Leach C, Nekhlyudov L (2019) Understanding long-term cancer survivors’ preferences for ongoing medical care. J Gen Intern Med 34(10):2091–2097. https://doi.org/10.1007/s11606-019-05189-y
Nyarko E, Metz JM, Nguyen GT, Hampshire MK, Jacobs LA, Mao JJ (2015) Cancer survivors’ perspectives on delivery of survivorship care by primary care physicians: an internet-based survey. BMC Fam Pract 16(1):143–143. https://doi.org/10.1186/s12875-015-0367-x
Tsiachristas A, Wallenburg I, Bond C, Elliot R, Busse R, van Exel J, Rutten-van Mölken M, de Bont A (2015) Costs and effects of new professional roles: evidence from a literature review. Health policy (Amsterdam, Netherlands) 119(9):1176–1187. https://doi.org/10.1016/j.healthpol.2015.04.001
McFarlane K, Dixon L, Wakeman C, Robertson G, Eglinton T, Frizelle F (2012) The process and outcomes of a nurse-led colorectal cancer follow-up clinic. Colorectal Dis 14(5):e245-249. https://doi.org/10.1111/j.1463-1318.2011.02923.x
Moloney J, Partridge C, Delanty S, Lloyd D, Nguyen M (2019) High efficacy and patient satisfaction with a nurse-led colorectal cancer surveillance programme with 10-year follow-up. ANZ J Surg 89(10):1286–1290. https://doi.org/10.1111/ans.15333
Howell D, Hack T, Oliver T, Chulak T, Mayo S, Aubin M, Chasen M, Earle C, Friedman A, Green E, Jones G, Jones J, Parkinson M, Payeur N, Sabiston C, Sinclair S (2012) Models of care for post-treatment follow-up of adult cancer survivors: a systematic review and quality appraisal of the evidence. Journal of cancer survivorship: research and practice 6(4):359–371. https://doi.org/10.1007/s11764-012-0232-z
Lewis R, Neal R, Williams N, France B, Wilkinson C, Hendry M, Russell D, Russell I, Hughes D, Stuart N, Weller D (2009) Nurse-led vs. conventional physician-led follow-up for patients with cancer: systematic review. J Adv Nurs 65(4):706–723. https://doi.org/10.1111/j.1365-2648.2008.04927.x
Greenfield D, Absolom K, Eiser C, Walters S, Michel G, Hancock B, Snowden J, Coleman R (2009) Follow-up care for cancer survivors: the views of clinicians. Br J Cancer 101(4):568–574. https://doi.org/10.1038/sj.bjc.6605160
Viklund P, Wengström YJL (2006) Supportive care for patients with oesophageal and other upper gastrointestinal cancers: the role of a specialist nurse in the team. Eur J Oncol Nurs 10(5):353–363.
Laurant M, van der Biezen M, Wijers N, Watananirun K, Kontopantelis E, van Vught A (2018) Nurses as substitutes for doctors in primary care. Cochrane Database Syst Rev 7:CD001271. https://doi.org/10.1002/14651858.CD001271.pub3
Burg M, Adorno G, Lopez E, Loerzel V, Stein K, Wallace C, Sharma D (2015) Current unmet needs of cancer survivors: analysis of open-ended responses to the American Cancer Society Study of Cancer Survivors II. Cancer 121(4):623–630. https://doi.org/10.1002/cncr.28951
Molassiotis A, Brunton L, Hodgetts J, Green A, Beesley V, Mulatero C, Newton-Bishop J, Lorigan P (2014) Prevalence and correlates of unmet supportive care needs in patients with resected invasive cutaneous melanoma. Ann Oncol 25(10):2052–2058. https://doi.org/10.1093/annonc/mdu366
Hubbard G, Venning C, Walker A, Scanlon K, Kyle R (2015) Supportive care needs of women with breast cancer in rural Scotland. Support Care Cancer 23(6):1523–1532. https://doi.org/10.1007/s00520-014-2501-z
Russell L, Gough K, Drosdowsky A, Schofield P, Aranda S, Butow P, Westwood J, Krishnasamy M, Young J, Phipps-Nelson J, King D, Jefford M (2015) Psychological distress, quality of life, symptoms and unmet needs of colorectal cancer survivors near the end of treatment. J Cancer Surviv 9(3):462–470. https://doi.org/10.1007/s11764-014-0422-y
Watson E, Shinkins B, Frith E, Neal D, Hamdy F, Walter F, Weller D, Wilkinson C, Faithfull S, Wolstenholme J, Sooriakumaran P, Kastner C, Campbell C, Neal R, Butcher H, Matthews M, Perera R, Rose P (2016) Symptoms, unmet needs, psychological well-being and health status in survivors of prostate cancer: implications for redesigning follow-up. BJU Int 117(6b):E10–E19. https://doi.org/10.1111/bju.13122
Funding
This work was supported by the funds of Undergraduates’ Teaching Reform Project of Jilin University (2019XYB295, 2019XYB252, ALK201946, SK202083, 2020zsjpk58); Scientific Research Projects of Higher Education in Jilin Province (JGJX2019D10, JGJX2019D6); and the National Natural Science Foundation of China (31800895).
Author information
Authors and Affiliations
Contributions
Made substantial contributions to the conception and design, or acquisition of data, or analysis and interpretation of data: LHQ, ZXY, XH.
Involved in drafting the manuscript or revising it critically for important intellectual content: LHQ, YH, XH.
Given final approval of the version to be published. Each author has participated sufficiently in the work to take public responsibility for appropriate portions of the content: LHQ, YH, WGY, XH, ZXY.
Agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved: ZXY, XH, LHQ.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was performed in accordance with the Declaration of Helsinki and was approved by the Ethics Committee of School of Nursing, Jilin University. We introduced the study to all participants and obtained their consent.
Consent for publication
The manuscript contains any individual person’s data in any form (including individual details, images or videos); consent for publication was obtained from that person.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Li, Hq., Yuan, H., Wan, Gy. et al. Preferences of gastric cancer survivors for follow-up care—a multicenter discrete choice experiment study. Support Care Cancer 30, 1221–1229 (2022). https://doi.org/10.1007/s00520-021-06505-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-021-06505-1