Abstract
Purpose
Taste alterations (TA) and oral discomfort in cancer patients are neglected side effects of the disease and treatments. They contribute to poor appetite, decrease food intake and affect quality of life, leading to adverse outcomes such as malnutrition and depression. The study aimed to explore TAs in relation to other oral conditions causing discomfort in cancer patients. Additionally, the correlation between patients’ acidity of saliva and experienced TAs and oral discomfort was evaluated.
Methods
A case study including 100 patients diagnosed with cancer receiving chemotherapy or immunotherapy. Data were collected using two questionnaire forms: the Chemotherapy-induced Taste Alteration Scale (CiTAS) and an additional information questionnaire. Saliva samples were collected for each patient and measured with a pocket pH meter. Data were analysed using descriptive statistics, and comparisons were performed using the Kruskal–Wallis H test, Mann–Whitney U test and Fisher’s exact test.
Results
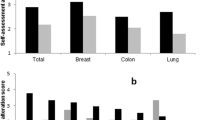
The prevalence of reported TAs was 93%. Patient age, oral discomfort and swallowing difficulty were found to be significant factors for experienced TAs (p < 0.05). No correlation between patients’ acidity of saliva and reported TAs and oral discomfort was found.
Conclusion
CiTAS proved to be a convenient tool to collect information about TAs in cancer patients. Using the CiTAS tool, a high prevalence (93%) of reported TAs in cancer patients receiving chemo- or immunotherapy was found. CiTAS provides a fast and cheap recognition of symptoms and causes of TAs that can be addressed.
Similar content being viewed by others
Data availability
All data were collected during the study and have not previously been published. The corresponding author has full control and access to all primary data. If requested, the journal Supportive Care in Cancer may review the data. The saliva samples are not kept.
Code availability
Not applicable.
References
Zabernigg A, Gamper E-M, Giesinger JM et al (2010) Taste alterations in cancer patients receiving chemotherapy: a neglected side effect? Oncologist 15:913–920. https://doi.org/10.1634/theoncologist.2009-0333
Van Oort S, Kramer E, De Groot JW, Visser O (2018) Taste alterations and cancer treatment. Curr Opin Support Palliat Care 12:162–167. https://doi.org/10.1097/SPC.0000000000000346
Drareni K, Dougkas A, Giboreau A et al (2019) Relationship between food behavior and taste and smell alterations in cancer patients undergoing chemotherapy: a structured review. Semin Oncol 46:160–172. https://doi.org/10.1053/j.seminoncol.2019.05.002
Nolden AA, Hwang LD, Boltong A, Reed DR (2019) Chemosensory changes from cancer treatment and their effects on patients’ food behavior: a scoping review. Nutrients 11:2285. https://doi.org/10.3390/nu11102285
Epstein JB, Smutzer G, Doty RL (2016) Understanding the impact of taste changes in oncology care. Support Care Cancer 24:1917–1931. https://doi.org/10.1007/s00520-016-3083-8
Bernhardson BM, Tishelman C, Rutqvist LE (2007) Chemosensory changes experienced by patients undergoing cancer chemotherapy: a qualitative interview study. J Pain Symptom Manage 34:403–412. https://doi.org/10.1016/j.jpainsymman.2006.12.010
McLaughlin L, Mahon SM (2012) Understanding taste dysfunction in patients with cancer. Clin J Oncol Nurs 16:171–178. https://doi.org/10.1188/12.CJON.171-178
Brisbois TD, De Kock IH, Watanabe SM et al (2011) Characterization of chemosensory alterations in advanced cancer reveals specific chemosensory phenotypes impacting dietary intake and quality of life. J Pain Symptom Manage 41:673–683. https://doi.org/10.1016/j.jpainsymman.2010.06.022
Doty RL (2015) Handbook of olfaction and gustation, 3rd edn. John Wiley & Sons Inc. (United States)
Murtaza B, Hichami A, Khan AS et al (2017) Alteration in taste perception in cancer: causes and strategies of treatment. Front Physiol 8:134. https://doi.org/10.3389/fphys.2017.00134
Hutton JL, Baracos VE, Wismer WV (2007) Chemosensory dysfunction is a primary factor in the evolution of declining nutritional status and quality of life in patients with advanced cancer. J Pain Symptom Manage 33:156–165. https://doi.org/10.1016/j.jpainsymman.2006.07.017
Pribitkin E, Rosenthal MD, Cowart BJ (2003) Prevalence and causes of severe taste loss in a chemosensory clinic population. Ann Otol Rhinol Laryngol 112:971–978. https://doi.org/10.1177/000348940311201110
Soter A, Kim J, Jackman A et al (2008) Accuracy of self-report in detecting taste dysfunction. Laryngoscope 118:611–617. https://doi.org/10.1097/MLG.0b013e318161e53a
Cohen J, Wakefield CE, Laing DG (2016) Smell and taste disorders resulting from cancer and chemotherapy. Curr Pharm Des 22:2253–2263
Kirkova J, Walsh D, Rybicki L et al (2010) Symptom severity and distress in advanced cancer. Palliat Med 24:330–339. https://doi.org/10.1177/0269216309356380
Uí Dhuibhir P, Barrett M, O’Donoghue N et al (2020) Self-reported and objective taste and smell evaluation in treatment-naive solid tumour patients. Support Care Cancer 28:2389–2396. https://doi.org/10.1007/s00520-019-05017-3
Spotten LE, Corish CA, Lorton CM et al (2017) Subjective and objective taste and smell changes in cancer. Ann Oncol Off J Eur Soc Med Oncol 28:969–984. https://doi.org/10.1093/annonc/mdx018
Likhterov I, Ru M, Ganz C et al (2018) Objective and subjective hyposalivation after treatment for head and neck cancer: Long-term outcomes. Laryngoscope 128:2732–2739. https://doi.org/10.1002/lary.27224
Ramya AS, Uppala D, Majumdar S et al (2015) Are salivary amylase and pH - prognostic indicators of cancers? J Oral Biol Craniofacial Res 5:81–85. https://doi.org/10.1016/j.jobcr.2015.04.002
Baliga S, Muglikar S, Kale R (2013) Salivary pH: a diagnostic biomarker. J Indian Soc Periodontol 17:461–465. https://doi.org/10.4103/0972-124X.118317
Granot M, NAGLER R, (2005) Association between regional idiopathic neuropathy and salivary involvement as the possible mechanism for oral sensory complaints. J Pain 6:581–587. https://doi.org/10.1016/j.jpain.2005.03.010
Tueros I, Uriarte M (2018) Innovative food products for cancer patients: future directions. J Sci Food Agric 98:1647–1652. https://doi.org/10.1002/jsfa.8789
Simeone S, Esposito MR, Gargiulo G et al (2019) The CiTAS scale for evaluating taste alteration induced by chemotherapy: state of the art on its clinical use. Acta Biomed 90:17–25. https://doi.org/10.23750/abm.v90i6-S.8278
Kano T, Kanda K (2013) Development and validation of a chemotherapy-induced taste alteration scale. Oncol Nurs Forum 40:E79–E85. https://doi.org/10.1188/13.ONF.E79-E85
Wild D, Grove A, Martin M et al (2005) Principles of good practice for the translation and cultural adaptation process for patient-reported outcomes (PRO) measures: report of the ISPOR task force for translating adaptation. Value Heal 8:94–104. https://doi.org/10.1111/j.1524-4733.2005.04054.x
Amézaga J, Alfaro B, Ríos Y et al (2018) Assessing taste and smell alterations in cancer patients undergoing chemotherapy according to treatment. Support Care Cancer 26:4077–4086. https://doi.org/10.1188/12.CJON.171-178
Sozeri E, Kutluturkan S (2015) Taste alteration in patients receiving chemotherapy. J Breast Heal 11:81–87. https://doi.org/10.5152/tjbh.2015.2489
Guillari Esposito AMR, Simeone S et al (2018) Dysgeusia in women undergoing cancer chemotherapy: results of a preliminary observational study. Gazz Med Ital 177:518–526
Steinbach S, Hummel T, Böhner C et al (2009) Qualitative and quantitative assessment of taste and smell changes in patients undergoing chemotherapy for breast cancer or gynecologic malignancies. J Clin Oncol 27:1899–1905. https://doi.org/10.1200/JCO.2008.19.2690
Belqaid K, Tishelman C, McGreevy J et al (2016) A longitudinal study of changing characteristics of self-reported taste and smell alterations in patients treated for lung cancer. Eur J Oncol Nurs 21:232–241. https://doi.org/10.1016/j.ejon.2015.10.009
Pugnaloni S, Vignini A, Borroni F et al (2020) Modifications of taste sensitivity in cancer patients: a method for the evaluations of dysgeusia. Support Care Cancer 28:1173–1181. https://doi.org/10.1007/s00520-019-04930-x
Fleming M, Craigs CL, Bennett MI (2020) Palliative care assessment of dry mouth: what matters most to patients with advanced disease? Support Care Cancer 28:1121–1129. https://doi.org/10.1007/s00520-019-04908-9
DeSimone JA, Lyall V (2006) Taste receptors in the gastrointestinal tract III. Salty and sour taste: Sensing of sodium and protons by the tongue. Am J Physiol - Gastrointest Liver Physiol 291:1005–1010. https://doi.org/10.1152/ajpgi.00235.2006
Abe K (2008) Studies on taste: molecular biology and food science. Biosci Biotechnol Biochem 72:1647–1656. https://doi.org/10.1271/bbb.70690
Mistretta CM, Kumari A (2017) Tongue and taste organ biology and function: homeostasis maintained by hedgehog signaling. Annu Rev Physiol 79:335–356. https://doi.org/10.1146/annurev-physiol-022516-034202
IJpma I, Renken RJ, ter Horst GJ, Reyners AKL, (2015) Metallic taste in cancer patients treated with chemotherapy. Cancer Treat Rev 41:179–186. https://doi.org/10.1016/j.ctrv.2014.11.006
Calvo SSC, Egan JM (2015) The endocrinology of taste receptors. Nat Rev Endocrinol 11:213–227
Campagna S, Gonella S, Stuardi M et al (2016) Italian validation of the chemotherapy induced taste alteration scale. Assist Inferm Ric 35:22–28. https://doi.org/10.1702/2228.24016
Sozeri E, Kutluturkan S (2018) The validity and reliability of turkish version of the chemotherapy-induced taste alteration scale (CiTAS). Clin Nurs Res 27:235–249. https://doi.org/10.1177/1054773816662436
Pang D, Qian L, Chen ZJ et al (2019) Psychometric properties of the Chinese version of the chemotherapy-induced taste alteration scale. Eur J Oncol Nurs 42:7–13. https://doi.org/10.1016/j.ejon.2019.07.007
US department of Health and Human Services (2010) Common terminology criteria for adverse events (CTCAE) version 4.03. National Instirutes of Health And National Cancer Institute, Washington, DC
Boltong A, Campbell K (2013) “Taste” changes: a problem for patients and their dietitians. Nutr Diet 70:262–269. https://doi.org/10.1111/1747-0080.12101
Epstein JB, Villines D, Epstein GL, Smutzer G (2020) Oral examination findings, taste and smell testing during and following head and neck cancer therapy. Support Care Cancer 28:4305–4311. https://doi.org/10.1007/s00520-019-05232-y
Epstein JB, Thariat J, Bensadoun R-J et al (2012) Oral complications of cancer and cancer therapy. CA Cancer J Clin 62:400–422. https://doi.org/10.3322/caac.21157
Murphy BA, Dietrich MS, Wells N et al (2010) Reliability and validity of the Vanderbilt head and neck symptom survey: a tool to assess symptom burden in patients treated with chemoradiation. Head Neck 32:26–37. https://doi.org/10.1002/hed.21143
Sevryugin O, Kasvis P, Vigano ML, Vigano A (2021) Taste and smell disturbances in cancer patients: a scoping review of available treatments. Support Care Cancer 29:49–66. https://doi.org/10.1007/s00520-020-05609-4
IJpma I, Timmermans ER, Renken RJ et al (2017) Metallic taste in cancer patients treated with systemic therapy: a questionnaire-based study. Nutr Cancer 69:140–145. https://doi.org/10.1080/01635581.2017.1250922
Imai H, Soeda H, Komine K et al (2013) Preliminary estimation of the prevalence of chemotherapy-induced dysgeusia in Japanese patients with cancer. BMC Palliat Care 12:38. https://doi.org/10.1186/1472-684X-12-38
Enriquez-Fernández BE, Nejatinamini S, Campbell SM et al (2019) Sensory preferences of supplemented food products among cancer patients: a systematic review. Support Care Cancer 27:333–349
Sun J, Peng Z, Zhou W et al (2015) A review on 3D printing for customized food fabrication. Procedia Manuf 1:308–319. https://doi.org/10.1016/j.promfg.2015.09.057
Funding
This work was financially supported by the Innovationsfonden (Denmark).
Author information
Authors and Affiliations
Contributions
Anne Kathrine Larsen and Marie Nerup Mortensen wrote the protocol. Anne Kathrine Larsen, Christine Thomsen, Mathilde Sanden and Camilla Bundgaard Anker collected the interview and saliva data. Lotte Boa Skadhauge collected data from the patients’ journals. Anne Kathrine Larsen and Christine Thomsen process the data. Anne Kathrine Larsen drafted the manuscript. Wender Bredie supervised the protocol and the findings of this work. All authors discussed the results and contributed to the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
In accordance with the Declaration of Helsinki, written consent was collected from each participant before inclusion. The Danish national committee on health research ethics approved the conduction of the study (ID: N-20180082). Patient information was pseudo-anonymized obeying General Data Protection Regulation (GDPR) rules.
Consent to participate and publication of results
Prior to inclusion orally and written information were presented. Participants were informed that participation was voluntarily and that they could withdraw from the study at any time. Informed consent was obtained from all individual participants included in the study and publication of study results.
Conflict of interest
The authors have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Larsen, A.K., Thomsen, C., Sanden, M. et al. Taste alterations and oral discomfort in patients receiving chemotherapy. Support Care Cancer 29, 7431–7439 (2021). https://doi.org/10.1007/s00520-021-06316-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-021-06316-4