Abstract
Background
Palliative care (PC) education for fellows in hematology/oncology (H/O) training programs is widely accepted, but no studies to date have assessed PC education practices and values among program leadership.
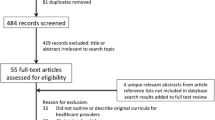
Methods
Program Directors and Associate Program Directors of active H/O fellowship programs in the U.S.A. were surveyed.
Results
Of 149 programs contacted, 84 completed the survey (56% response rate), of which 100% offered some form of PC education. The most frequently utilized methods of PC education were didactic lectures/conferences (93%), required PC rotations (68%), and simulation/role-playing (42%). Required PC rotations were ranked highest, and formal didactic seminars/conferences were ranked fifth in terms of perceived effectiveness. The majority felt either somewhat (60%) or extremely satisfied (30%) with the PC education at their program. Among specific PC domains, communication ranked highest, addressing spiritual distress ranked lowest, and care for the imminently dying ranked second lowest in importance and competency. Solid tumor oncologists reported more personal comfort with pain management (p = 0.042), non-pain symptom management (p = 0.014), ethical/legal issues (p = 0.029), reported their fellows were less competent in pain assessment/management (p = 0.006), and communication (p = 0.011), and were more satisfied with their program’s PC education (p = 0.035) as compared with hematologists.
Conclusions
Significant disparities exist between those modalities rated most effective for PC education and those currently in use. Clinical orientation of program leadership can affect both personal comfort with PC skills and estimations of PC curriculum effectiveness and fellows’ competency. H/O fellowship programs would benefit from greater standardization and prioritization of active PC education modalities and content.


Similar content being viewed by others
Data availability
Deidentified data for this study are available online via Open Science Framework at the following link: https://osf.io/eq5u2/?view_only=d1e6dd41f0dc4c98ac48f5936959650f
References
Dittrich C, Kosty M, Jezdic S et al (2016) ESMO/ASCO recommendations for a global curriculum in medical oncology edition 2016. ESMO Open 1(5):1–96.https://doi.org/10.1136/esmoopen-2016-000097
American Society of Hematology (2014) HEMATOLOGY-ONCOLOGY CURRICULAR MILESTONES: a collaboration of the American Society of Hematology & American Society of Clinical Oncology 4/18/14 EDITION. https://www.hematology.org/Educators/Training-Directors/2720.aspx. Accessed 07 July 2020
Ferris FD, Bruera E, Cherny N, Cummings C, Currow D, Dudgeon D, JanJan N, Strasser F, von Gunten CF, von Roenn JH (2009) Palliative cancer care a decade later: accomplishments, the need, next steps—from the American Society of Clinical Oncology. J Clin Oncol 27:3052–3058
Bickel KE, McNiff K, Buss MK et al (2016) Defining high-quality palliative care in oncology practice: an American Society of Clinical Oncology/American Academy of hospice and palliative medicine guidance statement. J Oncol Pract 12(9):828–838
Accreditation Council of Graduate Medical Education (2019) ACGME program requirements for graduate medical education in hematology and medical oncology.https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/155_HematologyAndMedicalOncology_2019.pdf?ver=2019-06-13-093131-547. Accessed 07 July 2020
Buss MK, Lessen DS, Sullivan AM, von Roenn J, Arnold RM, Block SD (2011) Hematology/ oncology fellows’ training in palliative care. Cancer 117:4304–4311
Thomas RA, Curley B, Wen S, Zhang J, Abraham J, Moss AH (2015) Palliative care training during fellowship: a national survey of U.S. hematology and oncology fellows. J Palliat Med 18(9):747–751
Hui D, Finlay E, Buss MK, Prommer EE, Bruera E (2015) Palliative oncologists: specialists in the science and art of patient care. J Clin Oncol 33(20):2314–2317. https://doi.org/10.1200/JCO.2014.60.3274
Mehta AK, May N, Verga S et al (2018) Palliative care education in U.S. adult neuro-oncology fellowship programs. J Neuro-Oncol 140:377. https://doi.org/10.1007/s11060-018-2963-9
Richman PS, Saft HL, Messina CR (2016) Palliative and end-of-life educational practices in US pulmonary and critical care training programs. J Crit Care 31(1):172–177
Larrieux G, Wachi BI, Miura JT et al (2015) Palliative care training in surgical oncology and hepatobiliary fellowships: a national survey of program directors. Ann Surg Oncol 22:S1181–S1186
Mougalian SS, Lessen DS, Levine RL, Panagopoulos G, von Roenn J, Arnold R, Block S, Buss M (2013) Palliative care training and associations with burnout in oncology fellows. J Support Oncol 11:95–102
Beaussant Y, Daguindau E, Chauchet A, Rochigneux P, Tournigand C, Aubry R, Morin L (2018) Hospital end-of-life care in haematological malignancies. BMJ Support Palliat Care 8(3):314–324
Hui D, Didwaniya N, Vidal M, Shin SH, Chisholm G, Roquemore J, Bruera E (2014) Quality of end-of-life care in patients with hematologic malignancies: a retrospective cohort study. Cancer 120(10):1572–1578
LeBlanc TW, Smith JM, Currow DC (2015) Symptom burden of haematological malignancies as death approaches in a community palliative care service: a retrospective cohort study of a consecutive case series. Lancet Haematol 2(8):e334–e338
Odejide OO, Cronin AM, Earle CC, LaCasce AS, Abel GA (2016) Hospice use among patients with lymphoma: impact of disease aggressiveness and curability. J Natl Cancer Inst 108(1):djv280
Weissman DE, Block SD (2002) ACGME requirements for end- of-life training in selected residency and fellowship programs: a status report. Acad Med 77:299–304
Hurst WJ (2004) The over lecturing and under teaching of clinical medicine. (reprinted) arch. Intern Med 164:1605–1608
Fink LD (2003) Creating significant learning experiences. Jossey-Bass, San Francisco
Kern DE, Thomas PA, Hughes MT (1998) Curriculum development for medical education: a six-step approach. Johns Hopkins University Press, Baltimore
Roth M, Wang D, Kim M, Moody K (2009) An assessment of the current state of palliative care education in pediatric hematology/oncology fellowship training. Pediatr Blood Cancer 53:647–651
Spiker M, Paulsen K, Mehta AK (2020) Primary palliative care education in US residencies and fellowships: a systematic review of program leadership perspectives. J Palliat Med 23(10):1392–1399. https://doi.org/10.1089/jpm.2020.0331
Lefkowits C, Sukumvanich P, Claxton R, Courtney-Brooks M, Kelley JL, McNeil MA, Goodman A (2014) Needs assessment of palliative care education in gynecologic oncology fellowship: we’re not teaching what we think is most important. Gynecol Oncol 135(2):255–260. https://doi.org/10.1016/j.ygyno.2014.08.016
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
The University of California, Los Angeles Institutional Review Board committee reviewed this study and declared it exempt from further review.
Consent to participate
Informed consent was obtained from all individual participants in this study.
Consent for publication
Participants consented to publication of submitted responses in aggregate. No individual identifying information of participants is included in this study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Al-Mondhiry, J.H., Burkenroad, A.D., Zhang, E. et al. Needs assessment of current palliative care education in U.S. hematology/oncology fellowship programs. Support Care Cancer 29, 4285–4293 (2021). https://doi.org/10.1007/s00520-020-05919-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05919-7