Abstract
Purpose
To examine cancer patients and their family caregivers’ perspectives of care coordination (CC) using a dyadic research design.
Methods
In this pilot cross-sectional study, 54 patient-family caregiver dyads completed a validated care coordination instrument (CCI) and its parallel family caregiver instrument (CCICG) from June to September 2019. The sample available for analysis included data from 32 dyads, which included patients receiving active therapy for any cancer type and their primary family caregivers aged 18 years or older. Mixed regression models were used to examine dyadic differences.
Results
The overall family caregiver scores demonstrated a bimodal pattern; thus, we conducted analyses using aggregate data as well as by highCG and lowCG subgroups. Among dyads in the lowCG subgroup, family caregivers reported significantly lower scores than patients on the total CCI and the three CC domains: Communication, Navigation, and Operational. Caregiver gender, the absence of a patient navigator, and practice setting (hospital-based ambulatory) significantly predicted dyadic differences in the lowCG subgroup. In item-level analyses, family caregivers in the lowCG subgroup reported lower scores than patients on the items related to patient-physician communication.
Conclusion
A subgroup of family caregivers reported poorer perception of CC than patients, suggesting that those family caregivers and providers may benefit from intervention. Further understanding of patient-family caregiver dyads’ perspectives of CC can inform development of strategies to integrate family caregivers into the cancer care team, develop effective CC interventions for family caregivers, and contribute to improved quality and value of cancer care.


Similar content being viewed by others
Availability of data and materials
The survey instruments used in this study are available by request from the corresponding author.
References
National Alliance for Caregiving (2016) Caregiving in the U.S. An intense, episodic, and challenging care experience
Agency for Healthcare Research and Quality (2014) Care Coordination Measures Atlas Update. Chapter 3: Care Coordination Measurement Framework. https://www.ahrq.gov/ncepcr/care/coordination/atlas/chapter3.html. Accessed 03/01/2020
IOM (2013) Delivering high-quality cancer care: charting a new course for a system in crisis. In: Levit L, Balogh E, Nass S, Ganz PA (eds) Delivering high-quality cancer care: charting a new course for a system in crisis, Washington. https://doi.org/10.17226/18359
Shrank WH, Rogstad TL, Parekh N (2019) Waste in the US health care system: estimated costs and potential for savings. JAMA 322(15):1501–1509. https://doi.org/10.1001/jama.2019.13978
Kvedar J, Coye MJ, Everett W (2014) Connected health: a review of technologies and strategies to improve patient care with telemedicine and telehealth. Health Aff (Millwood) 33(2):194–199. https://doi.org/10.1377/hlthaff.2013.0992
Bredart A, Kop JL, Efficace F, Beaudeau A, Brito T, Dolbeault S, Aaronson N, Group EQoL (2015) Quality of care in the oncology outpatient setting from patients’ perspective: a systematic review of questionnaires’ content and psychometric performance. Psychooncology 24(4):382–394. https://doi.org/10.1002/pon.3661
Kent EE, Mollica MA, Buckenmaier S, Wilder Smith A (2019) The characteristics of informal cancer caregivers in the United States. Semin Oncol Nurs 35(4):328–332. https://doi.org/10.1016/j.soncn.2019.06.002
Hassett MJ, McNiff KK, Dicker AP, Gilligan T, Hendricks CB, Lennes I, Murray T, Krzyzanowska MK (2014) High-priority topics for cancer quality measure development: results of the 2012 America006E Society of Clinical Oncology Collaborative Cancer Measure Summit. 10(3):e160–e166. https://doi.org/10.1200/jop.2013.001240
Mitchell K-AR, Brassil KJ, Fujimoto K, Fellman BM, Shay LA, Springer AE (2019) Exploratory factor analysis of a patient-centered cancer care measure to support improved assessment of patients’ experiences. Value Health
Evensen CTYK, Keller S, Arora NK, Frentzel E, Cowans T, Garfinkel SA (2019) Development and testing of the CAHPS cancer care survey. J Oncol Pract 15(11):e969–e977
Okado I, Cassel K, Pagano I, Holcombe RF (2020) Development and psychometric evaluation of a questionnaire to measure cancer patients’ perception of care coordination. BMC Health Serv Res 20(1):52. https://doi.org/10.1186/s12913-020-4905-4
Young JM, Walsh J, Butow PN, Solomon MJ, Shaw J (2011) Measuring cancer care coordination: development and validation of a questionnaire for patients. BMC Cancer 11:298. https://doi.org/10.1186/1471-2407-11-298
Ayanian JZ, Zaslavsky AM, Guadagnoli E, Fuchs CS, Yost KJ, Creech CM, Cress RD, O'Connor LC, West DW, Wright WE (2005) Patients’ perceptions of quality of care for colorectal cancer by race, ethnicity, and language. J Clin Oncol 23(27):6576–6586. https://doi.org/10.1200/JCO.2005.06.102
Durcinoska I, Young JM, Solomon MJ (2017) Patterns and predictors of colorectal cancer care coordination: a population-based survey of Australian patients. Cancer 123(2):319–326. https://doi.org/10.1002/cncr.30326
Okado I, Cassel K, Pagano I, Holcombe RF (In Press) Assessing patients’ perception of cancer care coordination in a community-based setting. JCO Oncology Practice
Gorin SS, Haggstrom D, Han PKJ, Fairfield KM, Krebs P, Clauser SB (2017) Cancer care coordination: a systematic review and meta-analysis of over 30 years of empirical studies. Ann Behav Med 51(4):532–546. https://doi.org/10.1007/s12160-017-9876-2
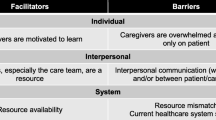
Walsh J, Harrison JD, Young JM, Butow PN, Solomon MJ, Masya L (2010) What are the current barriers to effective cancer care coordination? A qualitative study. BMC Health Serv Res 10:132. https://doi.org/10.1186/1472-6963-10-132
Patel MI, Periyakoil VS, Blayney DW, Moore D, Nevedal A, Asch S, Milstein A, Coker TR (2017) Redesigning cancer care delivery: views from patients and caregivers. J Oncol Pract 13(4):e291–e302. https://doi.org/10.1200/JOP.2016.017327
Mazor KM, Beard RL, Alexander GL, Arora NK, Firneno C, Gaglio B, Greene SM, Lemay CA, Robinson BE, Roblin DW, Walsh K, Street RL, Gallagher TH (2013) Patients’ and family members' views on patient-centered communication during cancer care. Psychooncology 22(11):2487–2495. https://doi.org/10.1002/pon.3317
Fletcher BS, Miaskowski C, Given B, Schumacher K (2012) The cancer family caregiving experience: an updated and expanded conceptual model. Eur J Oncol Nurs 16(4):387–398. https://doi.org/10.1016/j.ejon.2011.09.001
Gillick MR (2013) The critical role of caregivers in achieving patient-centered care. JAMA 310(6):575–576. https://doi.org/10.1001/jama.2013.7310
SAS Institute I (2019). Version 9.4 edn., Cary, NC
Bevans M, Sternberg EM (2012) Caregiving burden, stress, and health effects among family caregivers of adult cancer patients. JAMA 307(4):398–403. https://doi.org/10.1001/jama.2012.29
Shulman LN, Sheldon LK, Benz EJ (2020) The future of cancer care in the United States—overcoming workforce capacity limitations. JAMA Oncology 6(3):327–328. https://doi.org/10.1001/jamaoncol.2019.5358
Funding
This study was supported in part from a grant from the Hawaii Community Foundation, P30CA071789, and University of Hawaii Cancer Center.
Author information
Authors and Affiliations
Contributions
RFH, IO, and KC designed the study presented in the manuscript. IO administered surveys. IP conducted study analyses. All authors drafted, read, and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the University of Hawaii’s Institutional Review Board.
Code availability
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 76 kb)
Rights and permissions
About this article
Cite this article
Okado, I., Pagano, I., Cassel, K. et al. Perceptions of care coordination in cancer patient-family caregiver dyads. Support Care Cancer 29, 2645–2652 (2021). https://doi.org/10.1007/s00520-020-05764-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05764-8