Abstract
Purpose
Dental evaluation and management prior to hematopoietic stem cell transplant (HSCT) plays a vital role in identifying and treating infections that may be life-threatening. The purpose of this study is to describe the dental management of patients undergoing pre-HSCT examination with the Dental Service at Memorial Sloan Kettering Cancer Center (MSKCC) and to report on odontogenic complications.
Methods
Patients referred for evaluation as part of the standard preparation for HSCT were included. Following clinical and radiological examination, patients were assigned to one of three groups based on risk of odontogenic infection, and treatment was provided as indicated. Patients were followed, and their medical records were reviewed for odontogenic complications during the transplant admission.
Results
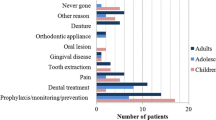
Of the 375 patients evaluated, 350 patients underwent HSCT: allogeneic 143 (40.9%) and autologous 207 (59.1%). The distribution of primary cancer diagnosis was as follows: multiple myeloma 104 (29.7%), leukemias 95 (27.1%), Hodgkin’s lymphoma 28 (8.0%), non-Hodgkin’s Lymphoma 99 (28.3%), and other conditions 24 (6.9%). The median time from dental evaluation to transplant was 29 days. The median Decayed, Missing, Filled Teeth Index was 17. The median Community Periodontal Index was 1. Based on dental status, 145 patients (41.4%) were classified as low risk, 133 (38%) as moderate risk and 72 (20.6%) as high risk of odontogenic infection. One hundred fourteen patients (32.6%) required dental treatment prior to HSCT, and 100 of these (28.6%) completed treatment. Two (0.57%) patients had odontogenic complications.
Conclusions
With conservative pre-HSCT dental treatment based on an infection risk classification system, a low odontogenic complication rate was observed.

Similar content being viewed by others
Data availability
The authors affirm that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned have been explained.
References
Epstein JB, Raber-Drulacher JE, Wilkins A, Chavarria MG, Myint H (2009) Advances in hematologic stem cell transplant: an update for oral health care providers. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 107(3):301–312
Copelan EA (2006) Hematopoietic stem-cell transplantation. N Engl J Med 354(17):1813–1826
Gratwohl A, Baldomero H, Aljurf M, Pasquini MC, Bouzas LF, Yoshimi A, Szer J, Lipton J, Schwendener A, Gratwohl M, Frauendorfer K, Niederwieser D, Horowitz M, Kodera Y (2010) Hematopoietic stem cell transplantation: a global perspective. Jama 303(16):1617–1624. https://doi.org/10.1001/jama.2010.491
Greenberg MS, Cohen SG, McKitrick JC, Cassileth PA (1982) The oral flor as a source of septicemia in patients with acute leukemia. Oral Surg Oral Med Oral Pathol 53(1):32–36
Heimdahl A, Mattsson T, Dahllof G, Lonnquist B, Ringden O (1989) The oral cavity as a port of entry for early infections in patients treated with bone marrow transplantation. Oral Surg Oral Med Oral Pathol 68(6):711–716
Elad S, Raber-Durlacher JE, Brennan MT, Saunders DP, Mank AP, Zadik Y, Quinn B, Epstein JB, Blijlevens NM, Waltimo T, Passweg JR, Correa ME, Dahllof G, Garming-Legert KU, Logan RM, Potting CM, Shapira MY, Soga Y, Stringer J, Stokman MA, Vokurka S, Wallhult E, Yarom N, Jensen SB (2015) Basic oral care for hematology-oncology patients and hematopoietic stem cell transplantation recipients: a position paper from the joint task force of the Multinational Association of Supportive Care in Cancer/International Society of Oral Oncology (MASCC/ISOO) and the European Society for Blood and Marrow Transplantation (EBMT). Support Care Cancer 23(1):223–236. https://doi.org/10.1007/s00520-014-2378-x
Heimdahl A (1999) Prevention and management of oral infections in cancer patients. Support Care Cancer 7(4):224–228
(1990) Consensus statement: oral complications of cancer therapies. National Institutes of Health Consensus Development Panel. NCI Monogr (9):3–8
Elad S, Thierer T, Bitan M, Shapira MY, Meyerowitz C (2008) A decision analysis: the dental management of patients prior to hematology cytotoxic therapy or hematopoietic stem cell transplantation. Oral Oncol 44(1):37–42
Graber CJ, De Almeida KNF, Atkinson JC, Javaheri D, Fukuda CD, Gill VJ, Barrett AJ, Bennett JE (2001) Dental health and viridans streptococcal bacteremia in allogeneic hematopoietic stem cell transplant recipients. Bone Marrow Transplant 27(5):537–542
CDC (2000) Guidelines for preventing opportunistic infections among hematopoietic stem cell transplant recipients. Recommendations of CDC, the Infectious Disease Society of America, and the American Society of Blood and Marrow Transplantation. https://www.cdc.gov/mmwr/preview/mmwrhtml/rr4910a1.htm. Accessed 1 May 2020
WHO (2013) World Health Organization Oral Health Surveys Basic Methods. http://www.who.int/oral_health/publications/9789241548649/en/. Accessed 1 May 2020
Nuernberg MA, Nabhan SK, Bonfim CM, Funke VA, Torres-Pereira CC (2016) Access to oral care before hematopoietic stem cell transplantation: understand to improve. Support Care Cancer 24(8):3307–3313. https://doi.org/10.1007/s00520-016-3142-1
Epstein JB, Guneri P, Barasch A (2014) Appropriate and necessary oral care for people with cancer: guidance to obtain the right oral and dental care at the right time. Support Care Cancer 22(7):1981–1988. https://doi.org/10.1007/s00520-014-2228-x
Durey K, Patterson H, Gordon K (2009) Dental assessment prior to stem cell transplant: treatment need and barriers to care. Br Dent J 206(9):E19–E19; discussion 479
Akashi M, Shibuya Y, Kusumoto J, Furudoi S, Inui Y, Yakushijin K, Okamura A, Matsuoka H, Komori T (2013) Myelosuppression grading of chemotherapies for hematologic malignancies to facilitate communication between medical and dental staff: lessons from two cases experienced odontogenic septicemia. BMC Oral Health 13:41. https://doi.org/10.1186/1472-6831-13-41
Sculean A, Gruber R, Bosshardt DD (2014) Soft tissue wound healing around teeth and dental implants. J Clin Periodontol 41(Suppl 15):S6–S22. https://doi.org/10.1111/jcpe.12206
Toljanic JA, Bedard JF, Larson RA, Fox JP (1999) A prospective pilot study to evaluate a new dental assessment and treatment paradigm for patients scheduled to undergo intensive chemotherapy for cancer. Cancer 85(8):1843–1848
Melkos AB, Massenkeil G, Arnold R, Reichart PA (2003) Dental treatment prior to stem cell transplantation and its influence on the posttransplantation outcome. Clin Oral Investig 7(2):113–115
Yamagata K, Onizawa K, Yanagawa T, Hasegawa Y, Kojima H, Nagasawa T, Yoshida H (2006) A prospective study to evaluate a new dental management protocol before hematopoietic stem cell transplantation. Bone Marrow Transplant 38(3):237–242
Peters E, Monopoli M, Woo SB, Sonis S (1993) Assessment of the need for treatment of postendodontic asymptomatic periapical radiolucencies in bone marrow transplant recipients. Oral Surg Oral Med Oral Pathol 76(1):45–48
Schuurhuis JM, Span LF, Stokman MA, van Winkelhoff AJ, Vissink A, Spijkervet FK (2016) Effect of leaving chronic oral foci untreated on infectious complications during intensive chemotherapy. Br J Cancer 114(9):972–978. https://doi.org/10.1038/bjc.2016.60
Sultan AS, Zimering Y, Petruzziello G, Alyea EP 3rd, Antin JH, Soiffer RJ, Ho VT, Sonis ST, Woo SB, Marty FM, Treister NS (2017) Oral health status and risk of bacteremia following allogeneic hematopoietic cell transplantation. Oral Surg Oral Med Oral Pathol Oral Radiol 124(3):253–260. https://doi.org/10.1016/j.oooo.2017.06.003
Elad S, Garfunkel AA, Or R, Michaeli E, Shapira MY, Galili D (2003) Time limitations and the challenge of providing infection-preventing dental care to hematopoietic stem-cell transplantation patients. Support Care Cancer 11(10):674–677
Fernandes LL, Torres SR, Garnica M, de Souza GL, Junior AS, de Vasconcellos AC, Cavalcanti W, Maiolino A, de Barros Torres MC (2014) Oral status of patients submitted to autologous hematopoietic stem cell transplantation. Support Care Cancer 22(1):15–21. https://doi.org/10.1007/s00520-013-1940-2
Ertas ET, Kurnaz F, Zorba YO, Kocyigit I, Sisman Y, Kaynar L, Sekerci AE, Ertas H, Cetin M (2014) Comparison of chemotherapy and hematopoietic stem cell transplantation pre and postterm DMFT scores: a preliminary study. Niger J Clin Pract 17(1):32–37. https://doi.org/10.4103/1119-3077.122831
Dobr T, Passweg J, Weber C, Tichelli A, Heim D, Meyer J, Gratwohl A, Waltimo T (2007) Oral health risks associated with HLA-types of patients undergoing hematopoietic stem cell transplantation. Eur J Haematol 78(6):495–499. https://doi.org/10.1111/j.1600-0609.2007.00841.x
Raber-Durlacher JE, Laheij AM, Epstein JB, Epstein M, Geerligs GM, Wolffe GN, Blijlevens NM, Donnelly JP (2013) Periodontal status and bacteremia with oral viridans streptococci and coagulase negative staphylococci in allogeneic hematopoietic stem cell transplantation recipients: a prospective observational study. Support Care Cancer 21(6):1621–1627. https://doi.org/10.1007/s00520-012-1706-2
Raber-Durlacher JE, Epstein JB, Raber J, van Dissel JT, van Winkelhoff AJ, Guiot HF, van der Velden U (2002) Periodontal infection in cancer patients treated with high-dose chemotherapy. Support Care Cancer 10(6):466–473. https://doi.org/10.1007/s00520-002-0346-3
Akintoye SO, Brennan MT, Graber CJ, McKinney BE, Rams TE, Barrett AJ, Atkinson JC (2002) A retrospective investigation of advanced periodontal disease as a risk factor for septicemia in hematopoietic stem cell and bone marrow transplant recipients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 94(5):581–588
Yamagata K, Onizawa K, Yanagawa T, Takeuchi Y, Hasegawa Y, Chiba S, Bukawa H (2011) Prospective study establishing a management plan for impacted third molar in patients undergoing hematopoietic stem cell transplantation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 111(2):146–152. https://doi.org/10.1016/j.tripleo.2010.09.006
Öhman D, Björk Y, Bratel J, Kristiansson C, Johansson P, Johansson JE, Brune M, Hasséus B (2010) Partially erupted third molars as a potential source of infection in patients receiving peripheral stem cell transplantation for malignant diseases: a retrospective study. Eur J Oral Sci 118(1):53–58
Acknowledgments
The authors would like to thank Kant Wu for his efforts and contributions to this project.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Heidi J. Hansen and SaeHee K.Yom. The first draft of the manuscript was written by Heidi J. Hansen, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the ethics committee of Memorial Sloan Kettering Cancer Center.
Consent to participate
An exemption and waiver of informed consent was granted for this study by the Institutional Review Board of Memorial Sloan Kettering Cancer Center.
Consent for publication
Not applicable.
Code availability
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hansen, H.J., Estilo, C., Owosho, A. et al. Dental status and risk of odontogenic complication in patients undergoing hematopoietic stem cell transplant. Support Care Cancer 29, 2231–2238 (2021). https://doi.org/10.1007/s00520-020-05733-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05733-1