Abstract
Purpose
Breast cancer survivors face a high risk of developing breast cancer-related lymphedema (BCRL). Besides physical symptoms such as swelling, BCRL can have a psychosocial impact and lead to problems in daily functioning. Understanding contributing variables to problems in functioning yields possibilities to improve treatment modalities and consequently patients’ quality of life. Therefore, the aim of this study was to explore the association between patient-, lymphedema-, and cancer treatment-related variables with problems in functioning in patients with BCRL.
Methods
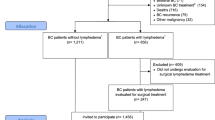
A cross-sectional study was performed in 185 patients with BCRL. Problems in daily functioning (dependent variable) were evaluated with the Lymph-ICF-UL questionnaire. Following independent variables were analysed by bi-variate and multivariable analyses, including a stepwise regression analysis: patient-related variables (age, BMI, physical activity level, education), lymphedema-related variables (excessive arm volume, duration of lymphedema, total pitting score, presence of hand edema, hardness of the tissue, lymphedema stage), and cancer treatment-related variables (type of surgery, surgery at the dominant side, radiotherapy, chemotherapy, hormone therapy, immunotherapy, TNM-classification).
Results
The Lymph-ICF-UL mean total score was 38% (± 21), representing a moderate amount of problems in general functioning. Multivariable regression analyses revealed that lower physical activity level and lower age are contributing factors to more problems in daily functioning. Stepwise regression analysis indicated that up to 8% of the variance in problems in functioning could be explained by physical activity level and age of patients with BCRL.
Conclusion
Especially patients with low physical activity level and younger patients experience more problems in functioning. For the determination of certain causal interactions, future longitudinal studies including other independent variables that might explain a higher amount of problems in functioning in this population, are warranted.
Trial registration
The study makes part of a double-blind, multi-center, randomized controlled trial (EFforT-BCRL trial), which is registered in clinicaltrials.gov (NCT02609724). CME reference S58689, EudraCT Number 2015-004822-33.
Similar content being viewed by others
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: Globocan estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424
Norman SA, Localio AR, Potashnik SL, Simoes Torpey HA, Kallan MJ, Weber AL, Miller LT, Demichele A, Solin LJ (2009) Lymphedema in breast cancer survivors: incidence, degree, time course, treatment, and symptoms. J Clin Oncol 27(3):390–397
DiSipio T, Rye S, Newman B, Hayes S (2013) Incidence of unilateral arm lymphoedema after breast cancer: a systematic review and meta-analysis. Lancet Oncol 14(6):500–515
Nguyen TT, Hoskin TL, Habermann EB, Cheville AL, Boughey JC (2017) Breast cancer-related lymphedema risk is related to multidisciplinary treatment and not surgery alone: results from a large cohort study. Ann Surg Oncol 24(10):2972–2980
Zhu YQ, Xie YH, Liu FH et al (2014) Systemic analysis on risk factors for breast cancer related lymphedema. Asian Pac J Cancer Prev 15(16):6535–6541
Kim M, Kim SW, Lee SU et al (2013) A model to estimate the risk of breast cancer-related lymphedema: combinations of treatment-related factors of the number of dissected axillary nodes, adjuvant chemotherapy, and radiation therapy. Int J Radiat Oncol Biol Phys 86(3):498–503
Shah C, Wilkinson JB, Baschnagel A et al (2012) Factors associated with the development of breast cancer-related lymphedema after whole-breast irradiation. Int J Radiat Oncol Biol Phys 83(4):1095–1100
Ugur S, Arici C, Yaprak M et al (2013) Risk factors of breast cancer-related lymphedema. Lymphat Res Biol 11(2):72–75
Morcos B, Al Ahmad F, Anabtawi I et al (2014) Development of breast cancer-related lymphedema: is it dependent on the patient, the tumor or the treating physicians? Surg Today 44(1):100–106
Basta MN, Wu LC, Kanchwala SK et al (2017) Reliable prediction of postmastectomy lymphedema: the risk assessment tool evaluating lymphedema. Am J Surg 213(6):1125–33.e1
Chachaj A, Malyszczak K, Pyszel K et al (2010) Physical and psychological impairments of women with upper limb lymphedema following breast cancer treatment. Psycho-oncology. 19(3):299–305
Organization WH (ed) (2001) International classification of functioning, disability and health. Icf, Geneva
Kostanjsek N (2011) Use of the international classification of functioning, disability and health (icf) as a conceptual framework and common language for disability statistics and health information systems. BMC Public Health 11(Suppl 4):S3
Cornelissen AJM, Kool M, Keuter XHA et al (2018) Quality of life questionnaires in breast cancer-related lymphedema patients: review of the literature. Lymphat Res Biol
Park JE, Jang HJ, Seo KS (2012) Quality of life, upper extremity function and the effect of lymphedema treatment in breast cancer related lymphedema patients. Ann Rehabil Med 36(2):240–247
Penha TR, Botter B, Heuts EM, Voogd AC, von Meyenfeldt M, van der Hulst R (2016) Quality of life in patients with breast cancer-related lymphedema and reconstructive breast surgery. J Reconstr Microsurg 32(6):484–490
Tsauo JY, Hung HC, Tsai HJ, Huang CS (2011) Can icf model for patients with breast-cancer-related lymphedema predict quality of life? Support Care Cancer 19(5):599–604
Sagen A, Kaaresen R, Sandvik L, Thune I, Risberg MA (2014) Upper limb physical function and adverse effects after breast cancer surgery: a prospective 2.5-year follow-up study and preoperative measures. Arch Phys Med Rehabil 95(5):875–881
O'Toole JA, Ferguson CM, Swaroop MN, Horick N, Skolny MN, Brunelle CL, Miller CL, Jammallo LS, Specht MC, Taghian AG (2015) The impact of breast cancer-related lymphedema on the ability to perform upper extremity activities of daily living. Breast Cancer Res Treat 150(2):381–388
Gärtner R, Jensen MB, Kronborg L et al (2010) Self-reported arm-lymphedema and functional impairment after breast cancer treatment—a nationwide study of prevalence and associated factors. Breast (Edinburgh, Scotland) 19(6):506–515
Pinto M, Gimigliano F, Tatangelo F, Megna M, Izzo F, Gimigliano R, Iolascon G (2013) Upper limb function and quality of life in breast cancer related lymphedema: a cross-sectional study. Eur J Phys Rehabil Med 49(5):665–673
Dawes DJ, Meterissian S, Goldberg M, Mayo NE (2008) Impact of lymphoedema on arm function and health-related quality of life in women following breast cancer surgery. J Rehabil Med 40(8):651–658
Beaulac SM, McNair LA, Scott TE et al (2002) Lymphedema and quality of life in survivors of early-stage breast cancer. Arch Surg (Chicago, Ill : 1960) 137(11):1253–1257
Hormes JM, Bryan C, Lytle LA, Gross CR, Ahmed RL, Troxel AB, Schmitz KH (2010) Impact of lymphedema and arm symptoms on quality of life in breast cancer survivors. Lymphology. 43(1):1–13
De Vrieze T, Vos L, Gebruers N et al (2017) Protocol of a randomised controlled trial regarding the effectiveness of fluoroscopy-guided manual lymph drainage for the treatment of breast cancer-related lymphoedema (effort-bcrl trial). Eur J Obstet Gynecol Reprod Biol
De Vrieze T, Vos L, Gebruers N et al (2019) Revision of the lymphedema functioning, disability and health questionnaire for upper limb lymphedema (lymph-icf-ul): reliability and validity. Lymphat Res Biol
Devoogdt N, Van Kampen M, Geraerts I et al (2011) Lymphoedema functioning, disability and health questionnaire (lymph-icf): reliability and validity. Phys Ther 91:944–957
Lee PH, Macfarlane DJ, Lam TH et al (2011) Validity of the international physical activity questionnaire short form (ipaq-sf): a systematic review. Int J Behav Nutr Phys Activity 8:115
Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, O'Brien WL, Bassett DR Jr, Schmitz KH, Emplaincourt PO, Jacobs DR Jr, Leon AS (2000) Compendium of physical activities: an update of activity codes and met intensities. Med Sci Sports Exerc 32(9 Suppl):S498–S504
De Vrieze T, Gebruers N, Nevelsteen I et al (2019) Reliability of the moisturemeterd compact device and the pitting test to evaluate local tissue water in subjects with breast cancer-related lymphedema. Lymphat Res Biol
Sun D, Yu Z, Chen J, Wang L, Han L, Liu N (2017) The value of using a skinfibrometer for diagnosis and assessment of secondary lymphedema and associated fibrosis of lower limb skin. Lymphat Res Biol 15(1):70–76
Caban ME (2002) Trends in the evaluation of lymphedema. Lymphology. 35(1):28–38
De Vrieze T GN, De Groef A, Dams L, Van der Gucht E, Nevelsteen I, Devoodt N. Reliability and time efficiency of five different methods to determine arm volume in patients with breast cancer-related lymphoedema. 2019
Martignon MVS, Fung LH, Vandermeeren L, Belgrado JP, Editor Evaluation of the reliability of four measuring methods of hand's perimeter and volume: buoyancy forces valgrado system, circumference measurement, figure-of-eight method and manu3metrix scanner. 8th International Lymphoedema Framework Conference; 2018; Rotterdam, The Netherlands
The diagnosis and treatment of peripheral lymphedema (2016) 2016 consensus document of the international society of lymphology. Lymphology 49(4):170–184
Evans JD (1996) Straightforward statistics for the behavioral sciences. Brooks/Cole Pub. Co, Pacific Grove
Forde DC (2019) Scoring the international physical activity questionnaire (ipaq) Dublin: Trinity College Dublin. Available from: https://ugc.futurelearn.com/uploads/files/bc/c5/bcc53b14-ec1e-4d90-88e3-1568682f32ae/IPAQ_PDF.pdf
Ryan DJ, Wullems JA, Stebbings GK, Morse CI, Stewart CE, Onambele-Pearson GL (2018) Reliability and validity of the international physical activity questionnaire compared to calibrated accelerometer cut-off points in the quantification of sedentary behaviour and physical activity in older adults. PLoS One 13(4):e0195712
Devoogdt N, Van Kampen M, Christiaens MR et al (2011) Short- and long-term recovery of upper limb function after axillary lymph node dissection. Eur J Cancer Care 20(1):77–86
Iioka Y, Iwata T, Yamauchi H (2019) Symptoms and qol in breast cancer patients receiving hormone therapy in japan. Breast Cancer (Tokyo, Japan)
Acknowledgments
All authors critically revised the manuscript for important intellectual content and approved the final manuscript.
Funding
This study is financed by the Agency for Innovation by Science and Technology, applied Biomedical Research (IWT 150178). In order to arrange such financing, a separate collaboration agreement has been signed by the KU Leuven and the beneficiaries.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare. The authors have full control of all primary data and allow the journal to review the data if requested.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Support statement: ADG is a post-doctoral research fellow of the FWO-Flanders.
Appendices
Appendix 1
Appendix 2
Rights and permissions
About this article
Cite this article
De Vrieze, T., Gebruers, N., Nevelsteen, I. et al. Physical activity level and age contribute to functioning problems in patients with breast cancer-related lymphedema: a multicentre cross-sectional study. Support Care Cancer 28, 5717–5731 (2020). https://doi.org/10.1007/s00520-020-05375-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05375-3