Abstract
Purpose
The transition from active cancer treatment to palliative care often results in a shift in drug risk-benefit assessment which requires the deprescribing of various medications. Deprescribing in palliative cancer patients can benefit patients by reducing their pill burden, decrease potential side effects, and potentially decrease healthcare costs. In addition, a change in patients’ goals of care (GOC) necessitates the alteration of drug therapy which includes both deprescribing and the addition of medications intended to improve quality of life. Depending on a patient’s GOC, a medication can be considered as inappropriate.
Objectives
Primary: Comparison between potentially inappropriate medications (PIMs) prior to the palliative care consult (PCC) versus after the PCC. Secondary: Association between PIMs and GOC.
Methods
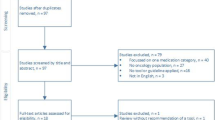
The study was a 1-year retrospective database review. The study included cancer patients seen by the PCC team at the University of Alberta Hospital. The OncPal guidelines were used to identify and determine the number of PIMs prior to the PCC and after the PCC.
Results
The reduction in PIMs prior to PCC versus after the PCC was statistically significant (p value < 0.001), demonstrating the PCC has a positive significant impact on deprescribing PIMs. For our secondary outcome, an overall decrease in PIMs was observed with the changes of GOC. The strength of the correlations was low (r < 0.1), and the p value was 0.056.
Conclusion
This study shows the positive impact a PCC has on deprescribing and reveals the importance of using guidelines for deprescribing in palliative cancer patients.
Similar content being viewed by others
References
Scott IA, Hilmer SN, Reeve E et al (2015) Reducing inappropriate polypharmacy. JAMA Intern Med Online 175(5):827–834
Oliveira L, Ferreira MO, Rola A, Magalhaes M, Ferraz GJ (2016) Deprescription in advanced cancer patients referred to palliative care. J Pain Palliat Care Pharmacother 30(3):2015
Lindsay J, Dooley M, Martin J et al (2015) The development and evaluation of an oncological palliative care deprescribing guideline: the ‘OncPal deprescribing guideline. J Support Care Cancer 23(1):71–78
Raskin W, Harle I, Hopman WM, Booth CM (2016) Prognosis, treatment benefit and goals of care: what do oncologists discuss with patients who have incurable cancer? J Clin Oncol 28(3):209–214
Stanek S (2017) Goals of care: a concept clarification. J Adv Nurs 73(6):1302–1314
Alberta Health Services. Advance care planning and goals of care designation. 2014. Available from:http://insite.albertahealthservices.ca/assets/klink/et-klink-ckv-advance-care-planning-goals-of-care-designations-all-ages-all-locations.pdf .Accessed November 23, 2017
R Core Team. R: a language and environment for statistical computing. R Foundation for Statistical Computing. Available from: https://www.R-project.org/. Accessed May 01, 2018
Parikh RB, Kirch RA, Smith TJ, Temel JS (2013) Early specialty palliative care-translating data in oncology into practice. New Engl J Med 369(24):2347–2351
Whitford K, Shah ND, Moriarty J, Branda M, Thorsteinsdottir B (2014) Impact of a palliative care consult service. Am J Hospice and Palliat Med 31(2):175–182
Wentlandt K, Krzyzanowska MK, Swami N et al (2012) Referral practices of oncologists to specialized palliative care. J of Clin Oncology 30(35):4380–4386
Fede A, Miranda M, Antonangelo D et al (2011) Use of unnecessary medications by patients with advanced cancer: cross-sectional survey. J Support Care Cancer 19(9):1313–1318
Lindsay J, Dooley M, Martin J et al (2014) Reducing potentially inappropriate medications in palliative cancer patients: evidence to support deprescribing approaches. J Support Care Cancer 22(4):1113–1119
Kierner KA, Weixler D, Masel EK, Gartner V, Watzke HH (2016) Polypharmacy in the terminal stage of cancer. J Support Care Cancer 24(5):2067–2074
Lima JD (2017) Thromboprophylaxis in cancer patients in palliative care setting. Ann of Res Hosp 1(8):9–9
Tardy B, Picard S, Guirimand F et al (2018) Bleeding risk of terminally ill patients hospitalized in palliative care units: the RHESO study. J of Thromb and Haemost 15(3):420–428
Pottie K, Thompson W, Davies S, Grenier J, Sadowski CA, Farrell B (2018) Deprescribing benzodiazepine receptor agonists. Can Fam Physician 64(5):339 LP–339351
Stone MJ (2001) Goals of care at the end of life. Proc Bayl Univ Med Cent 14(2):134–137
White N, Reid F, Harris A, Harries P, Stone P (2016) A systematic review of predictions of survival in palliative care: how accurate are clinicians and who are the experts? PLoS One 11(8):120
Acknowledgments
I would like to thank my parents Juan Jose Marin Rojas and Maria Cecilia Bejarano Meza as well as the rest of my family for their constant love and support throughout my life. I would especially like to thank the patients that I encountered during my residency; they taught me the true meaning of resilience and gratitude. This paper is dedicated to the memory of my aunts Norma and Yadira Bejarano, who inspired me to complete a residency in oncology in order to help patients during one of the biggest challenges they will face in their lives.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval was given by the Health Research Ethics Board Alberta Cancer Committee. Furthermore, we received a waiver of consent, as it was not feasible to obtain informed consent as the majority of patients would have passed away. Additionally, we restricted extracting only the limited data that was needed for our primary and secondary outcomes.
Disclaimer
The primary author has full control of all primary data and agrees to allow the journal to review the data if requested.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 144 kb)
Rights and permissions
About this article
Cite this article
Marin, H., Mayo, P., Thai, V. et al. The impact of palliative care consults on deprescribing in palliative cancer patients. Support Care Cancer 28, 4107–4113 (2020). https://doi.org/10.1007/s00520-019-05234-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-019-05234-w