Abstract
Objective
Evidence on municipality-based cancer rehabilitation is sparse. This longitudinal study explores the following: (1) Rehabilitation needs, (2) effectiveness of municipality-based rehabilitation, and (3) whether rehabilitative services are stratified according to individual needs in breast cancer patients.
Methods
We collected data from a longitudinal survey among 82 breast cancer patients referred to municipality-based rehabilitation at the Copenhagen Centre for Cancer and Health. Rehabilitation needs, health-related quality of life (HRQoL), and functional status were collected using patient-reported outcomes (PROs) including distress thermometer, problem list, Functional Assessment of Cancer Therapy-Breast questionnaire (FACT-B), and upper body function with the abbreviated disability of the arm, shoulder, and hand (Quick-DASH) questionnaire. Data collection time points are as follows: entry, follow-up, and end of intervention.
Results
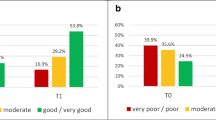
At referral, scores were (mean (range)) distress 4.0 (0–10), problems 9.5 (0–24), and FACT-B 103.0 (49.8–135.5). HRQoL increased during rehabilitation (FACT-B ∆ mean 8.1 points (> MID, p < 0.0001)); 56% had a positive change, 34% no difference, and 11% a decline. Those with the lowest FACT-B entry score had significantly longer duration of rehabilitation (10.9 vs 8.7 months, p < 0.001), higher number of services (7.0 vs 5.3, p < 0.003), and participated more in group-based exercise (+3 sessions: 57% vs 8%, p < 0.001).
Conclusion
This is the first study to report on pragmatic municipality-based cancer rehabilitation. The results suggest that services are aimed at patients with rehabilitation needs, improve HRQoL, and are properly stratified to those who need it the most. We suggest future monitoring of municipality-based rehabilitation services to ensure quality of care.

Similar content being viewed by others
References
Ammitzbøll G, Søgaard K, Karlsen RV, Tjønneland A, Johansen C, Frederiksen K, Bidstrup P (2016) Physical activity and survival in breast cancer. Eur J Cancer 66:67–74. https://doi.org/10.1016/j.ejca.2016.07.010
Ibrahim EM, Al-Homaidh A (2011) Physical activity and survival after breast cancer diagnosis: meta-analysis of published studies. Med Oncol 28:753–765. https://doi.org/10.1007/s12032-010-9536-x
Tomlinson D, Diorio C, Beyene J, Sung L (2014) Effect of exercise on cancer-related fatigue: a meta-analysis. Am J Phys Med Rehabil 93:675–686. https://doi.org/10.1097/PHM.0000000000000083
Buffart LM, Kalter J, Sweegers MG, Courneya KS, Newton RU, Aaronson NK, Jacobsen PB, May AM, Galvão DA, Chinapaw MJ, Steindorf K, Irwin ML, Stuiver MM, Hayes S, Griffith KA, Lucia A, Mesters I, van Weert E, Knoop H, Goedendorp MM, Mutrie N, Daley AJ, McConnachie A, Bohus M, Thorsen L, Schulz KH, Short CE, James EL, Plotnikoff RC, Arbane G, Schmidt ME, Potthoff K, van Beurden M, Oldenburg HS, Sonke GS, van Harten WH, Garrod R, Schmitz KH, Winters-Stone KM, Velthuis MJ, Taaffe DR, van Mechelen W, Kersten MJ, Nollet F, Wenzel J, Wiskemann J, Verdonck-de Leeuw IM, Brug J (2017) Effects and moderators of exercise on quality of life and physical function in patients with cancer: an individual patient data meta-analysis of 34 RCTs. Cancer Treat Rev 52:91–104. https://doi.org/10.1016/j.ctrv.2016.11.010
Mewes JC, Steuten LMG, IJzerman MJ, van Harten WH (2012) Effectiveness of multidimensional cancer survivor rehabilitation and cost-effectiveness of cancer rehabilitation in general: a systematic review. Oncologist 17:1581–1593. https://doi.org/10.1634/theoncologist.2012-0151
The Danish Health Authority (2018) Forløbsprogram for rehabilitering og palliation i forbindelse med kræft. Sundhedsstyrelsen/The Danish Health Authority
(2016) WHO Framework on integrated people-centred health services, A report by the Secretariat. In: WHO. http://www.who.int/servicedeliverysafety/areas/people-centred-care/en/ http://www.webcitation.org/6xrVctlJR. Accessed 11 May 2017
Ministry of the Interior and Health (2011) Vejledning om kommunal rehabilitering. Indenrigs- og Sundhedsministeriet
Lindström Egholm C, Rossau HK, Nilsen P, Bunkenborg G, Rod MH, Doherty P, Bartels P, Helmark L, Zwisler AD (2018) Implementation of a politically initiated national clinical guideline for cardiac rehabilitation in hospitals and municipalities in Denmark. Health Policy Amst Neth 122:1043–1051. https://doi.org/10.1016/j.healthpol.2018.07.015
Thuesen J, Rossau H, Frausing S, et al (2017) Kræftrehabilitering i Danmark: kortlægning af praksis på hospitaler og i kommuner. REHPA - The Danish knowledge Centre for Rehabilitation and Palliative Care
Kristiansen M, Adamsen L, Piil K, Halvorsen I, Nyholm N, Hendriksen C (2017) A three-year national follow-up study on the development of community-level cancer rehabilitation in Denmark. Scand J Public Health. https://doi.org/10.1177/1403494817746535
Thisted LB, Høstrup H (2015) Support in living with cancer - development of preparedness form for patients and relatives. Dan J Nurs:72–76
WHO | International Classification of Functioning, Disability and Health (ICF). In: WHO. http://www.who.int/classifications/icf/en/. Accessed 1 Nov 2018
Bandura A (1977) Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev 84:191–215. https://doi.org/10.1037/0033-295X.84.2.191
Miller WR (1996) Motivational interviewing: research, practice, and puzzles. Addict Behav 21:835–842
Borg GA (1982) Psychophysical bases of perceived exertion. Med Sci Sports Exerc 14:377–381
Jensen VM, Rasmussen AW (2011) Danish education registers. Scand J Public Health 39:91–94. https://doi.org/10.1177/1403494810394715
Webster K, Cella D, Yost K (2003) The Functional Assessment of Chronic Illness Therapy (FACIT) measurement system: properties, applications, and interpretation. Health Qual Life Outcomes 1:79. https://doi.org/10.1186/1477-7525-1-79
Eton DT, Cella D, Yost KJ, Yount SE, Peterman AH, Neuberg DS, Sledge GW, Wood WC (2004) A combination of distribution- and anchor-based approaches determined minimally important differences (MIDs) for four endpoints in a breast cancer scale. J Clin Epidemiol 57:898–910. https://doi.org/10.1016/j.jclinepi.2004.01.012
Yost KJ, Eton DT (2005) Combining distribution- and anchor-based approaches to determine minimally important differences: the FACIT experience. Eval Health Prof 28:172–191. https://doi.org/10.1177/0163278705275340
Beaton DE, Wright JG, Katz JN, Upper Extremity Collaborative Group (2005) Development of the QuickDASH: comparison of three item-reduction approaches. J Bone Joint Surg Am 87:1038–1046. https://doi.org/10.2106/JBJS.D.02060
Gummesson C, Ward MM, Atroshi I (2006) The shortened disabilities of the arm, shoulder and hand questionnaire (QuickDASH): validity and reliability based on responses within the full-length DASH. BMC Musculoskelet Disord 7:44. https://doi.org/10.1186/1471-2474-7-44
Jayadevappa R, Cook R, Chhatre S (2017) Minimal important difference to infer changes in health-related quality of life—a systematic review. J Clin Epidemiol 89:188–198. https://doi.org/10.1016/j.jclinepi.2017.06.009
National Comprehensive Cancer Network (2019) NCCN Clinical practice guidelines for oncology - Distress Management
Head BA, Schapmire TJ, Keeney CE, Deck SM, Studts JL, Hermann CP, Scharfenberger JA, Pfeifer MP (2012) Use of the distress thermometer to discern clinically relevant quality of life differences in women with breast cancer. Qual Life Res 21:215–223. https://doi.org/10.1007/s11136-011-9934-3
Bidstrup PE, Mertz BG, Dalton SO, Deltour I, Kroman N, Kehlet H, Rottmann N, Gärtner R, Mitchell AJ, Johansen C (2012) Accuracy of the Danish version of the ‘distress thermometer.’. Psychooncology 21:436–443. https://doi.org/10.1002/pon.1917
Bantema-Joppe EJ, de Bock GH, Woltman-van Iersel M, Busz DM, Ranchor AV, Langendijk JA, Maduro JH, van den Heuvel ER (2015) The impact of age on changes in quality of life among breast cancer survivors treated with breast-conserving surgery and radiotherapy. Br J Cancer 112:636–643. https://doi.org/10.1038/bjc.2014.632
Goyal NG, Levine BJ, Van Zee KJ et al (2018) Trajectories of quality of life following breast cancer diagnosis. Breast Cancer Res Treat 169:163–173. https://doi.org/10.1007/s10549-018-4677-2
Harrison SA, Hayes SC, Newman B (2010) Age-related differences in exercise and quality of life among breast cancer survivors. Med Sci Sports Exerc 42:67–74. https://doi.org/10.1249/MSS.0b013e3181b0f2cb
King MT, Kenny P, Shiell A, Hall J, Boyages J (2000) Quality of life three months and one year after first treatment for early stage breast cancer: influence of treatment and patient characteristics. Qual Life Res Int J Qual Life Asp Treat Care Rehabil 9:789–800
Idler E, Cartwright K (2018) What do we rate when we rate our health? Decomposing age-related contributions to self-rated health. J Health Soc Behav 59:74–93. https://doi.org/10.1177/0022146517750137
Ganz PA, Kwan L, Stanton AL, Bower JE, Belin TR (2011) Physical and psychosocial recovery in the year after primary treatment of breast cancer. J Clin Oncol 29:1101–1109. https://doi.org/10.1200/JCO.2010.28.8043
Shimozuma K, Ganz PA, Petersen L, Hirji K (1999) Quality of life in the first year after breast cancer surgery: rehabilitation needs and patterns of recovery. Breast Cancer Res Treat 56:45–57
Taira N, Shimozuma K, Shiroiwa T, Ohsumi S, Kuroi K, Saji S, Saito M, Iha S, Watanabe T, Katsumata N (2011) Associations among baseline variables, treatment-related factors and health-related quality of life 2 years after breast cancer surgery. Breast Cancer Res Treat 128:735–747. https://doi.org/10.1007/s10549-011-1631-y
De Gournay E, Guyomard A, Coutant C et al (2013) Impact of sentinel node biopsy on long-term quality of life in breast cancer patients. Br J Cancer 109:2783–2791. https://doi.org/10.1038/bjc.2013.658
Gordon LG, Battistutta D, Scuffham P, Tweeddale M, Newman B (2005) The impact of rehabilitation support services on health-related quality of life for women with breast cancer. Breast Cancer Res Treat 93:217–226. https://doi.org/10.1007/s10549-005-5151-5
Round T, Hayes SC, Newman B (2006) How do recovery advice and behavioural characteristics influence upper-body function and quality of life among women 6 months after breast cancer diagnosis? Support Care Cancer Off J Multinatl Assoc Support Care Cancer 14:22–29. https://doi.org/10.1007/s00520-005-0838-z
DiSipio T, Hayes S, Newman B, Janda M (2008) Health-related quality of life 18 months after breast cancer: comparison with the general population of Queensland, Australia. Support Care Cancer Off J Multinatl Assoc Support Care Cancer 16:1141–1150. https://doi.org/10.1007/s00520-007-0392-y
Scott DA, Mills M, Black A, Cantwell M, Campbell A, Cardwell CR, Porter S, Donnelly M, Cochrane Gynaecological, Neuro-oncology and Orphan Cancer Group (2013) Multidimensional rehabilitation programmes for adult cancer survivors. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD007730.pub2
Duncan M, Moschopoulou E, Herrington E, Deane J, Roylance R, Jones L, Bourke L, Morgan A, Chalder T, Thaha MA, Taylor SC, Korszun A, White PD, Bhui K, SURECAN Investigators (2017) Review of systematic reviews of non-pharmacological interventions to improve quality of life in cancer survivors. BMJ Open 7:e015860. https://doi.org/10.1136/bmjopen-2017-015860
Gebruers N, Camberlin M, Theunissen F, Tjalma W, Verbelen H, van Soom T, van Breda E (2019) The effect of training interventions on physical performance, quality of life, and fatigue in patients receiving breast cancer treatment: a systematic review. Support Care Cancer Off J Multinatl Assoc Support Care Cancer 27:109–122. https://doi.org/10.1007/s00520-018-4490-9
Hayes SC, Rye S, DiSipio T, Yates P, Bashford J, Pyke C, Saunders C, Battistutta D, Eakin E (2013) Exercise for health: a randomized, controlled trial evaluating the impact of a pragmatic, translational exercise intervention on the quality of life, function and treatment-related side effects following breast cancer. Breast Cancer Res Treat 137:175–186. https://doi.org/10.1007/s10549-012-2331-y
Danish Health Authority (2012) Forløbsprogram for rehabilitering og palliation i forbindelse med kræft - del afsamlet forløbsprogram for kræft. Kbh
McEwen S, Egan M, Chasen M, Fitch M (2013) Consensus recommendations for cancer rehabilitation: research and education priorities. Curr Oncol 20. https://doi.org/10.3747/co.20.1277
Zwisler A-D, Rossau HK, Nakano A, Foghmar S, Eichhorst RI, Prescott EIB, Cerqueira CS, Soja AMB, Gislason GH, Larsen ML, Andersen UO, Gustafsson I, Thomsen KK, Hansen LB, Hammer S, Viggers L, Christensen B, Kvist B, Egholm ACL, May O (2016) The Danish cardiac rehabilitation database. Clin Epidemiol 8:451–456. https://doi.org/10.2147/CLEP.S99502
Acknowledgements
The authors would like to thank the patients and staff at the rehabilitation center who participated in the study and Malene Strømberg Rasmussen for handling registry data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Online Resource 1
(PDF 137 kb)
Online Resource 2
(PDF 97 kb)
Rights and permissions
About this article
Cite this article
Rossen, S., Trier, K., Christensen, B. et al. Municipality-based pragmatic rehabilitation stratified in accordance with individual needs—results from a longitudinal survey study. Support Care Cancer 28, 1951–1961 (2020). https://doi.org/10.1007/s00520-019-04993-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-019-04993-w