Abstract
Purpose
The aim of this study was to compare health-care expenditures and survival of these terminally ill patients receiving or not receiving hospice care in their last month of life.
Methods
Using Taiwan’s National Health Insurance Claims Database, we analyzed hospitalizations, OPD visits, associated costs, and survival. Logistic regression was used to identify predictors of high cost.
Results
We identified 3850 liver cancer patients who died during the 1997–2011 study period, 644 (16.6 %) of whom were hospice care patients. No significant difference was found in mean survival time between the hospice and non-hospice groups (1.77 ± 2.44 vs. 1.84 ± 2.37 years, p = 0.217). The mean health-care expenditures per person were US$2370 ± 3421 and US$2072 ± 1900 (p = 0.130). A total of 385 patients (10 %) received high-cost care (above US$5422) using 38.6 % of the total health-care expenditures spent on the entire population. The significant predictors of high costs were non-hospice care [odds ratio (OR) = 3.06, 95 % confidence interval (CI) 2.09–4.60], days of admission [risk increase per admission day being (OR = 1.19, 95 % CI 1.17–1.21)], admission into an intensive care unit (OR = 3.17, 95 % CI 1.94 to 5.15), use of ventilator (OR = 3.54, 95 % CI 1.91–6.52), cancer therapy (OR = 1.82, 95 % CI 1.33–2.48), hemodialysis (OR = 2.62, 95 % CI 1.07–6.02), and higher socioeconomic status (OR = 1.65, 95 % CI 1.10–2.45).
Conclusion
Hospice care did not significantly affect survival, and hospice patients had lower per-patient expenditures and were less likely to require high-cost medical care than their non-hospice counterparts.
Similar content being viewed by others
Introduction
The goal of hospice care is to relieve pain and suffering of the terminally ill patients. In Taiwan, of all those receiving hospice care, 12.4 % receive it at home while 87.6 % receive it in the hospital. Still the overall use of either hospital- and home-based hospice services in Taiwan by those during their last year of life has only gradually increased for over the last 20 years, and it remains underutilized at 7.34 % in 2000 and 16.83 % in 2006 [1]. This underutilization has also been reported in the USA [2].
Meanwhile, over the last 10 years, overall care for terminally ill patients has become increasingly aggressive with the hope of extending survival [1, 3, 4]. Some who believe that hospice care is performed to relieve pain and suffering but not extend life are concerned that hospice may in fact hasten death [5]. However, one non-blinded randomized control trial by Temel et al. [6] reported that patients with metastatic non-small cell lung cancer who received early palliative care integrated with standard oncologic care lived 2 months longer than those receiving standard care only. Saito et al. [7] in a cohort study of elderly patients with lung cancer in the USA [8] reported that hospice did not shorten survival. Connor et al. [8] found that receiving hospice care did not affect the survival of patients with breast, prostate, and colon cancer, but it extended the survival of those with pancreatic and lung cancer as well as congestive heart failure. Liver cancer is another important disease, especially in Taiwan, where it was the second leading cause of cancer-related mortality in 2004 and accounted for 8116 (18.6 %) of 43,665 cancer deaths in 2012 [9]. It is not known to what extent hospice affects the survival of terminally ill patients with liver cancer in Taiwan.
Another concern is the possibly disproportionate cost of providing end-of-life care. Although it has been reported that over one quarter of Medicare expenditures for hospice or otherwise in the USA from 1978–2006 were spent on recipients during their last year of life [10], a review of studies of palliative care from different parts of the world by Smith et al. found hospice care to frequently be less costly than other types of end-of-life care [11]. In Japan, on the other hand, Morishima et al., performing a cross-sectional retrospective study comparing different care models for patients in the last 3 months of their life, found an association between hospice care as well as death at acute-care hospitals, chemotherapy, and opioid and higher health-care expenditures [12]. How hospice might affect the cost of end-of-life care in Taiwan has not been investigated.
This study compared survival and health-care expenditures of patients with liver cancer who received hospice care and those of patients who receive such care during their last month of life using claims data from Taiwan’s National Health Insurance (NHI) program.
Methods
Data source
In this national population-based cohort study, we analyzed data obtained from the computerized National Health Insurance Research Database (NHIRD) of Taiwan. Implemented in March 1995, Taiwan’s National Health Insurance (NHI) program is a single-payer health insurance system which covered up to 98.4 % in 2007 [13]. The NHIRD, a nationwide representative database containing all original claims data for one million NHI beneficiaries from 1996 to 2012, is a random, systemic sample of the 23.22 million NHI enrollees. In Taiwan, patients with cancer must be examined to receive what is known as a catastrophic illness certificate (CIC). We used the NHIRD to identify patient with liver cancer and the catastrophic illness database to identify patients receiving hospice care for terminally ill liver cancer. Patients under 20 years old were excluded in this study. We followed up patients to December 2012 using what is known as the 2000 Longitudinal Health Insurance Database (LHID2000).
Identification
The subjects were linked to the LHID2000 to obtain the hospital care visit data collected from 1997 to 2011. The International Classification of Diseases, Ninth Revision, Clinical Modification and A codes were used to define liver cancer (155, 155.0, 155.1, A095), liver cirrhosis (571.5, 571.6, and 571.2), HBV (070.20–070.23, 070.30–070.33, V0261, and A046), and HCV (070.41, 070.44, 070.51, 070.54, V0262, and A046). To increase the validity of the diagnosis of diabetes as well as hypertension, we included only patients who had three instances of the ICD-9-CM or A codes for these disease entities in their medical claims.
Definition of variables
The socioeconomic status (SES) of individuals
According to previous studies [14, 15], we classified SES into three group: low being those earning below than US$571 monthly (New Taiwan Dollars NT$20,000), moderate being those earning between US$571 and US$1141 monthly (NT$20,000–40,000), and high being those earning more than US$1141 monthly (NT$ 40,000).
Charlson comorbidity index (CCI)
CCI was calculated by examining ICD-9 Clinical Modification diagnosis and procedure codes recorded in the year prior to diagnosis, according to the Deyo method and applied to inpatient and outpatients claims as it was by Klabunde et al. [16–18].
Health-care expenditures
Each patient’s health-care expenditures were categorized into inpatient service and outpatient services. We converted costs based on the US dollar and NT dollar year 2006 exchange rate (US$1.00 = NT$32.53).
The protocol for this study was reviewed and approved by the Research Ethics Committee of the Buddhist Dalin Tzu Chi Hospital, Taiwan (No. B10301001). Since the NHIRD files only contained de-identified secondary data, the review board waived the need for informed consent.
Statistical analysis
Statistical analysis was performed using the R 3.0.2 software (R Foundation for Statistical Computing, Vienna, Austria). Two-sided p value ≤0.05 was considered significant. The survival duration (years) was defined as the duration from the day of diagnosis to the day of death (in years). The distributional properties of continuous variables were expressed by mean ± standard deviation (SD); categorical variables were presented by frequency and percentage. In univariate analysis, two-sample t test, Wilcoxon rank-sum test, chi-square test, and Fisher’s exact test were used to examine the differences in the distributions of continuous variables and categorical variables between two groups.
Patient’s demographic and clinical characteristics including age, gender, Charlson comorbidity index (CCI), geographic area of residence, and treatment modality (see Table 1) were considered in this regression analysis.
Multivariate analysis was conducted by fitting multiple logistic regression models with the stepwise variable selection procedure to identify important predictors of high cost during the last month of life, where the high cost = 1 if the health-care expenditure was higher than the 10th percentile of the total health-care expenditure, 0 if otherwise. Generalized additive models (GAMs) were fitted to detect potential nonlinear effects of continuous covariates and identify appropriate cutoff points for discretizing continuous covariates if necessary during the stepwise variable selection. Computationally, the vgam function (with the default values of smoothing parameters) of the VGAM package was used to fit GAMs for the binary outcome in R [19, 20].
The goodness-of-fit (GOF) of the final logistic regression model was assessed by the estimated area under the receiver operating characteristic (ROC) curve (also called the c statistic), where 0 ≤ c ≤ 1, and the Hosmer-Lemeshow GOF test. In practice, c ≥ 0.7 suggests an acceptable level of discrimination power for a fitted logistic regression model. And, the p value of the Hosmer-Lemeshow test >0.05 passes the assessment.
Finally, the statistical tools of regression diagnostics for residual analysis, detection of influential cases, and check of multicollinearity were applied to discover any problems with the model or data. The values of variance inflating factor (VIF) ≥10 in continuous covariates or ≥2.5 in categorical covariates indicate the occurrence of the multicollinearity problem among some of the covariates in the fitted logistic regression model.
Results
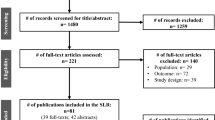
A total of 3850 adult patients with liver cancer who died in 1997–2011 were enrolled. In total, we collected 2735 men and 1115 women (ratio = 2.4:1). This study design was presented in Fig. 1. The mean ± SD (median) survival in years after diagnosis for patients receiving hospice care (H group) and not receiving hospice care (non-H group) were 1.77 ± 2.44 (0.70) and 1.84 ± 2.37 (0.83) years, respectively. The mean ± SD (median) days from hospice enrollment to death were 39.5 ± 85.5 (16) days. Among 644 patients who received hospice palliative care, 91 patients (14.1 %) were referred to hospice care in the last 3 days of their life, and 80 patients (12.4 %) also received home hospice care. Compared with the non-hospice group, there was a significant association among the following variables and receiving hospice care: being female (p = 0.008), older (p < 0.001), worse hypertension (p < 0.001), less cirrhosis comorbidity (p < 0.001), and lower Charlson comorbidity index (CCI) score (p = 0.021). The non-H group were more likely to reside in a suburban area (p = 0.035) and less likely to receive care in a teaching hospital than the H group (p < 0.001). Other demographic characteristics are shown in Table 1.
The H group had significantly fewer intensive care unit (ICU) admissions (p < 0.001), fewer than one emergency room (ER) visit (p = 0.001), fewer intubations (p < 0.001), fewer mechanical ventilation (p < 0.001), fewer new hemodialysis (p < 0.001), and fewer transarterial chemoembolizations (TACE; p = 0.002). They were more likely to ever have been admitted to a hospital (p = 0.002), to have more than one hospital admission (p < 0.001), to have hospital stays more than 14 days (p = 0.002), and to die in a hospital (p < 0.001) (Table 2).
The mean health-care expenditure of the hospice group in the last month of their life was less than that of the non-hospice care recipients, though the difference did not reach significance (US$2072 vs. US$2370, p = 0.130).
Three hundred eighty-five subjects (10 %) had health-care expenditure falling above the 90th percentile (US$5422), defined as high cost in this study. They consumed 38.6 % of total health-care expenditure. There were fewer high-cost subjects in the hospice group (35, 0.9 %) than in the non-hospice group (350, 9.1 %) (p < 0.001). High cost of last month of life care was significantly associated with non-hospice care (OR = 3.06, 95 % CI 2.09–4.60, p < 0.010), admission days (OR = 1.19, 95 % CI 1.17–1.21, p < 0.001), having an ICU admission (OR = 3.17, 95 % CI 1.94–5.15, p < 0.001), use of a ventilator (OR = 3.54, 95 % CI 1.91–6.52, p < 0.001), cancer therapy (OR = 1.82, 95 % CI 1.33–2.48, p < 0.001) and hemodialysis (OR = 2.62, 95 % CI 1.07–6.02, p = 0.028), and higher socioeconomic status (HES; OR = 1.65, 95 % CI 1.10–2.45, p < 0.001) (Table 3). The Nagelkerke R 2 was 0.421, and the Hosmer-Lemeshow test was passed (p = 0.229). ROC curve analyses revealed that this model for cost more than the 90th percentile yielded a sensitivity of 86.2 % (95 CI 82.4–89.5 %), a specificity of 79.3 % (95 CI 77.9–80.7 %), a positive predictive value of 31.7 % (95 CI 28.9–34.6 %), a negative predictive value of 98.1 % (95 CI 97.5–98.6 %), and an area under the ROC curve (AUC) of 0.898 (95 % CI 0.885–0.910) for the prediction of high cost (Fig. 2).
Discussion
This study found that the mean survival values of the hospice group and non-hospice group were not significantly different and that those not receiving hospice care were 3.06 times more likely to receive high-cost care than those receiving hospice care after an adjustment for various confounders.
This study found the mean survival after the date of diagnosis in hospice and non-hospice group to be 1.77 ± 2.44 and 1.84 ± 2.37 years, respectively, a result similar to that reported for liver cancer patients by Zhang et al. (1.87 ± 0.19 years) [21] and for lung cancer patients by Saito et al. [7]. Considering these findings together, it is clear that hospice care does no hasten death and this notion should not be used as a barrier to hospice service.
The study found non-hospice care as well as number of admission days, ICU admission, use of ventilator, cancer therapy, hemodialysis, and higher socioeconomic status to be associated with high-cost health care. Hospice care has been found to significantly reduce health-care expenditures. Smith et al., in a review study of hospice research reports from various counties, found significant reductions in health-care expenditures for hospice care patients [11]. Emanuel also reported significant reductions in health-care expenditure for hospice patients in their last month of life in the USA, compared to non-hospice patients, and 25–40 % savings [22]. Gozalo et al., performing a retrospective cohort study of nursing home recipients of hospice care in the USA, also found a 6 % reduction in expenditures, based on Medicare-Medicaid data [23]. In addition, in Spain, a multicenter prospective study of cancer patients receiving palliative care performed by Gomez-Batiste et al. reported that hospice care reduced the National Health Service costs by 61 % in patients during their last 6 weeks of life, compared to those who did not receive palliative care [24]. We found the mean health-care expenditure per person of advanced liver cancer patients receiving hospice care to be 12.6 % less than that of those not receiving hospice care in the last month of their life in Taiwan (H group US$2072 vs. non-H group US$2370). In a previous nationwide survey in Taiwan, Lin et al. reported that advanced cancer patients who received hospice care had 15.4 % less health-care expenditure per person than those who did not (US$4314 vs. US$5099) [25]. The difference in findings might be related to the fact that our study was limited to liver cancer patients; the percentage of elderly patients was 55.1 %, and the percentage of receiving hospice home care was 2.1 % in their last month of life. We also found that subjects with health-care expenditure falling into the 90th percentile (high cost) consumed 38.6 % of total health-care expenditure for all patients in their last month of life. In the USA, the cost of end-of-life medical care accounts for 10–12 % of total health-care budget [22]. Carlson et al. reported that Medicare subjects with health-care expenditures falling into the 95th percentile consumed 40 % of total Medicare expenditures during 1998–2002 [26]. The reason our findings were lower may be related to the differences in our studies. They studied a population who was 65 years older and who had a higher number of possible comorbidities, while our study included terminally ill patients 20 years or older and the number of elderly patients we studied was 2121 (55.1 %). In addition, most of their patients (86.4 %) received hospice care at home [26], which might involve greater health-care transportation and time costs, while most of our patients (87.6 %) received in-hospital hospice care.
Limitation
This study has some limitations. One limitation is the possibility of misclassification bias due to the accuracy of some of the variables used, including the identification of hospice use and the calculation of the comorbidity score. Another limitation is a possible selection bias, which might occur because the study was not randomized. This study also has a potential limitation of the retrospective nature.
Conclusion
This study found no significant difference in survival between advanced liver cancer patients receiving hospice and those who were not. The mean cost of health care of advanced liver cancer patients receiving hospice care was 12.6 % less than that of those not receiving hospice care during their last month of life. Hospice patients were less likely to receive high-cost care than non-hospice patients after adjustment. Further study is needed to estimate the effect of high cost of health care on patient and family satisfaction with care and perceptions of quality in the last month of life.
Abbreviations
- AUC:
-
Area under the receiver operating characteristic curve
- CCI:
-
Charlson comorbidity index
- CIC:
-
Catastrophic illness certificate
- ER:
-
Emergency room
- HBV:
-
Hepatitis B virus
- HCV:
-
Hepatitis C virus
- ICU:
-
Intensive care unit
- NHI:
-
National Health Insurance
- NHIRD:
-
National Health Insurance Research Database
- PEI:
-
Percutaneous ethanol injection
- ROC:
-
Receiver operating characteristic
- RFA:
-
Radiofrequency ablation
- SES:
-
Socioeconomic status
References
Tang ST, Wu SC, Hung YN et al (2009) Trends in quality of end-of-life care for Taiwanese cancer patients who died in 2000–2006. Ann Oncol 20:343–348
Han B, Remsburg RE, McAuley WJ et al (2006) National trends in adult hospice use: 1991–1992 to 1999–2000. Health Aff (Millwood) 25:792–799
Barnato AE, McClellan MB, Kagay CR, Garber AM (2004) Trends in inpatient treatment intensity among Medicare beneficiaries at the end of life. Health Serv Res 39:363–375
Earle CC, Neville BA, Landrum MB et al (2004) Trends in the aggressiveness of cancer care near the end of life. J Clin Oncol 22:315–321
Gawande A (2010) Letting go. What should medicine do when it can’t save your life? In New Yorker, August 2, 2010. http://www.newyorker.com/reporting/2010/08/02/100802fa_fact_gawande?currentPage = all. Accessed 25 January 2014.
Temel JS, Greer JA, Muzikansky A et al (2010) Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med 363:733–742
Saito AM, Landrum MB, Neville BA et al (2011) Hospice care and survival among elderly patients with lung cancer. J Palliat Med 14:929–939
Connor SR, Pyenson B, Fitch K et al (2007) Comparing hospice and nonhospice patient survival among patients who die within a three-year window. J Pain Symptom Manage 33:238–246
Ministry of Health and Welfare. Statistics of causes of death, Volume 1. http://www.mohw.gov.tw/cht/DOS/Statistic.aspx?f_list_no=312 & fod_list_no=2747 Accessed 18 January 2014.
Riley GF, Lubitz JD (2010) Long-term trends in Medicare payments in the last year of life. Health Serv Res 45:565–576
Smith S, Brick A, O’Hara S, Normand C (2013) Evidence on the cost and cost-effectiveness of palliative care: a literature review. Palliat Med 28:130–150
Morishima T, Lee J, Otsubo T, Imanaka Y (2014) Association of healthcare expenditures with aggressive versus palliative care for cancer patients at the end of life: a cross-sectional study using claims data in Japan. Int J Qual Health Care 26:79–86
National Health Insurance Research Database (NHIRD), Taiwan. http://nhird.nhri.org.tw/date_01.html Accessed 19 December 2013.
Lee CC, Su YC, Ho HC et al (2011) Risk of stroke in patients hospitalized for isolated vertigo: a four-year follow-up study. Stroke 42:48–52
Chang CM, Huang KY, Hsu TW et al (2012) Multivariate analyses to assess the effects of surgeon and hospital volume on cancer survival rates: a nationwide population-based study in Taiwan. PLoS One 7:e40590
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Deyo RA, Cherkin DC, Ciol MA (1992) Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 45:613–619
Klabunde CN, Potosky AL, Legler JM, Warren JL (2000) Development of a comorbidity index using physician claims data. J Clin Epidemiol 53:1258–1267
Yee TW, Wild CJ (1996) Vector generalized additive models. J R Stat Soc Series B Stat Methodol 58:481–493
Yee TW (2013) VGAM: Vector generalized linear and additive models. R package, version 0.9-2 (URL: http://CRAN.R-project.org/package=VGAM).
Zhang SM, Zeng ZC, Tang ZY et al (2008) Prognostic analysis of pulmonary metastases from hepatocellular carcinoma. Hepatol Int 2:237–243
Emanuel EJ (1996) Cost savings at the end of life. What do the data show? JAMA 275:1907–1914
Gozalo PL, Miller SC, Intrator O et al (2008) Hospice effect on government expenditures among nursing home residents. Health Serv Res 43:134–153
Gomez-Batiste X, Tuca A, Corrales E et al (2006) Resource consumption and costs of palliative care services in Spain: a multicenter prospective study. J Pain Symptom Manage 31:522–532
Lin WY, Chiu TY, Ho CT et al (2014) Hospice shared-care saved medical expenditure and reduced the likelihood of intensive medical utilization among advanced cancer patients in Taiwan—a nationwide survey. Support Care Cancer 22:1907–1914
Carlson MD, Herrin J, Du Q et al (2010) Impact of hospice disenrollment on health care use and Medicare expenditures for patients with cancer. J Clin Oncol 28:4371–4375
Acknowledgments
This study is based in part on data from the National Health Insurance Research Database provided by the Bureau of National Health Insurance, Department of Health and managed by the National Health Research Institutes. The interpretation and conclusions contained herein do not represent those of the Bureau of National Health Insurance, Department of Health or National Health Research Institutes. JK Chiang received research grants from Buddhist Dalin Tzu Chi Hospital (DTCRD 102 (2)-E-01). We also thank James Steed for the editing and advice on this manuscript.
Conflict of interest
The authors declare that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chiang, JK., Kao, YH. The impact of hospice care on survival and cost saving among patients with liver cancer: a national longitudinal population-based study in Taiwan. Support Care Cancer 23, 1049–1055 (2015). https://doi.org/10.1007/s00520-014-2447-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-014-2447-1