Abstract
Purpose
Hospice shared care (HSC) is a new care model that has been adopted to treat inpatient advanced cancer patients in Taiwan since 2005. Our aim was to assess the effect of HSC on medical expenditure and the likelihood of intensive medical utilization by advanced cancer patients.
Methods
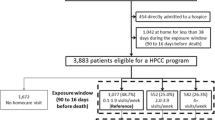
This is a nationwide retrospective study. HSC was defined as using “Hospice palliative care (HPC) teams to provide consultation and service to advanced cancer patients admitted in the nonhospice care ward.” There were 120,481 deaths due to cancer between 2006 and 2008 in Taiwan. Patients receiving HSC were matched by propensity score to patients receiving usual care. Of the 120,481 cancer deaths, 12,137 paired subjects were matched. Medical expenditures for 1 year before death were assessed between groups using a database from the Bureau of National Health Insurance. Paired t and McNemar’s tests were applied for comparing the medical expenditure and intensive medical utilization before death between paired groups.
Results
Compared to the non-HSC group, subjects receiving HSC had a lower average medical expenditure per person (US$3,939 vs. US$4,664; p < 0.001). The HSC group had an adjusted net savings of US$557 (13.3 %; p < 0.001) in inpatient medical expenditure per person compared with the non-HSC group. Subjects that received different types of HPC had 15.4–44.9 % less average medical expenditure per person and significantly lower likelihood of intensive medical utilization than those that did not receive HPC.
Conclusions
HSC is associated with significant medical expenditure savings and reduced likelihood of intensive medical utilization. All types of HPC are associated with medical expenditure savings.

Similar content being viewed by others
References
Barnato AE, McClellan MB, Kagay CR, Garber AM (2004) Trends in inpatient treatment intensity among Medicare beneficiaries at the end of life. Health Serv Res 39:363–375
Carlson MD, Herrin J, Du Q, Epstein AJ, Barry CL, Morrison RS, Back AL, Bradley EH (2010) Impact of hospice disenrollment on health care use and medicare expenditures for patients with cancer. J Clin Oncol Off J Am Soc Clin Oncol 28:4371–4375
Chen L, Yip W, Chang MC, Lin HS, Lee SD, Chiu YL, Lin YH (2007) The effects of Taiwan’s National Health Insurance on access and health status of the elderly. Health Econ 16:223–242
Congressional Budget Office (2005) High-cost medicare beneficiaries. http://www.cbo.gov/ftpdocs/63xx/doc6332/05-03-MediSpendingpdf
Dehejia RH, Wahba S (2002) Propensity score-matching methods for nonexperimental causal studies. Rev Econ Stat 84:151–161
Department of Health, Executive Yuan, R.O.C., (TAIWAN) (2010) Protect the right to bodily autonomy, and the dinity of human life. http://www.doh.gov.tw/CHT2006/DM/DM2002_p2001.aspe?class_no=2387&level_no=2001&doc_no=76172
Department of Health, Executive Yuan, Taiwan (2010) 2008 Statistics of causes of death. http://www.doh.gov.tw/EN2006/DM/DM2_p01aspx?class_no=390&now_fod_list_no=10864&level_no=2&doc_no=75601 Accessed 11 August, 2011
Emanuel EJ (1996) Cost savings at the end of life. JAMA J Am Med Assoc 275:1907
Emanuel EJ (1996) Cost savings at the end of life. What do the data show? JAMA J Am Med Assoc 275:1907–1914
Hill J, Reiter JP (2006) Interval estimation for treatment effects using propensity score matching. Stat Med 25:2230–2256
J.Ferlay, F.Bray, P.Pisani, D.M. Parkin (2001) GLOBOCAN 2000: cancer incidence, mortality and prevalence worldwide. IARC CancerBase No 5. IARCPress, Lyon
Jocham HR, Dassen T, Widdershoven G, Halfens R (2006) Quality of life in palliative care cancer patients: a literature review. J Clin Nurs 15:1188–1195
Lin WY, Chiu TY, Hsu HS, Davidson LE, Lin T, Cheng KC, Chiu CF, Li CI, Chiu YW, Lin CC, Liu CS (2009) Medical expenditure and family satisfaction between hospice and general care in terminal cancer patients in Taiwan. J Formos Med Assoc 108:794–802
Mariotto AB, Yabroff KR, Shao Y, Feuer EJ, Brown ML (2011) Projections of the cost of cancer care in the United States: 2010–2020. J Natl Cancer Inst 103:117–128
McCall N (1984) Utilization and costs of Medicare services by beneficiaries in their last year of life. Med Care 22:329–342
Morrison RS, Penrod JD, Cassel JB, Caust-Ellenbogen M, Litke A, Spragens L, Meier DE (2008) Cost savings associated with US hospital palliative care consultation programs. Arch Intern Med 168:1783–1790
Paice JA, Muir JC, Shott S (2004) Palliative care at the end of life: comparing quality in diverse settings. Am J Hosp Palliat Care 21:19–27
Pan YL (2009) Comparison of quality of life between hospice palliative care and hospice shared care patients—example of a Medical Center Taipi Medical University. http://libir.tmu.edu.tw/handle/987654321/987654601
Parsons LS (2001) Reducing bias in a propensity score matched-pair sample using greedy matching techniques. Paper 214-26. SAS Institute, Cary, NC.
Penrod JD, Deb P, Dellenbaugh C, Burgess JF Jr, Zhu CW, Christiansen CL, Luhrs CA, Cortez T, Livote E, Allen V, Morrison RS (2010) Hospital-based palliative care consultation: effects on hospital cost. J Palliat Med 13:973–979
Penrod JD, Deb P, Luhrs C, Dellenbaugh C, Zhu CW, Hochman T, Maciejewski ML, Granieri E, Morrison RS (2006) Cost and utilization outcomes of patients receiving hospital-based palliative care consultation. J Palliat Med 9:855–860
Pyenson B, Connor S, Fitch K, Kinzbrunner B (2004) Medicare cost in matched hospice and non-hospice cohorts. J Pain Symptom Manage 28:200–210
Chuang R-B (2005) Introduction of hospital-based palliative shared care program. Taiwan J Hosp Palliat Care 10:39–43
Chuang R-B, Lee I-F, Chiu T-Y, Wang J-Z, Lai Y-L, Hsiao S-C, Hsu T-H (2005) A preliminary experience of hospice shared-care model in Taiwan. Taiwan J Hosp Palliat Care 10:234–242
Spector WD, Mor V (1984) Utilization and charges for terminal cancer patients in Rhode Island inquiry. J Med Care Org Provision Financing 21:328–337
The SUPPORT, Investigators P (1995) A controlled trial to improve care for seriously ill hospitalized patients. The study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT). The SUPPORT Principal Investigators. JAMA: J Am Med Assoc 274:1591–1598
Acknowledgments
We thank the medical staff in hospice palliative medicine throughout Taiwan for their assistance in completing this study. This study was financially supported by grants from the Bureau of Health Promotion, Department of Health, Executive Yuan, Taiwan (DOH96-HP-1502, DOH97-HP-1503), from China Medical University Hospital (DMR-99-109), and from Taiwan Department of Health, China Medical University Hospital Cancer Research Center of Excellence (DOH102-TD-B-111-004).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lin, WY., Chiu, TY., Ho, CT. et al. Hospice shared-care saved medical expenditure and reduced the likelihood of intensive medical utilization among advanced cancer patients in Taiwan—a nationwide survey. Support Care Cancer 22, 1907–1914 (2014). https://doi.org/10.1007/s00520-014-2168-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-014-2168-5