Abstract
Background
Rituximab (RTX) is increasingly being used in place of calcineurin inhibitors (CNI) in pediatric patients with steroid-dependent nephrotic syndrome (SDNS). However, despite its favorable safety profile, its unit cost is prohibitive. We therefore compared the healthcare costs associated with the use of both agents in a retrospective cohort.
Methods
This study was a retrospective analysis of data retrieved from the medical charts and electronic databases of pediatric patients (age range 2–18 years) with SDNS who were treated with either CNI or RTX from January 2008 to December 2012 at Children’s Hospital of New Orleans, Louisiana. The minimum follow-up period was 12 months.
Results
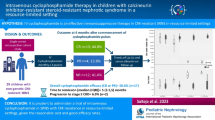
Of the 18 patients whose medical data were analyzed, ten received RTX and eight were treated with CNI. The annualized healthcare cost for the rituximab group was $197,031 versus $189,857 (all values in US dollars) for the CNI group (p > 0.05). At the 12-month follow-up, more patients in the RTX group were in remission (40 vs. 25%). Duration of freedom from steroid use was longer in the RTX group, while body mass index was higher in the CNI arm (p > 0.05). No significant adverse events occurred in either group.
Conclusion
The expenditure for the RTX and CNI groups was comparable, but there were fewer clinical encounters in the former group, potentially reducing the burden of healthcare on the patient’s family.
Similar content being viewed by others
References
Oh J, Kemper MJ (2012) Minimal change (steroid sensitive) nephrotic syndrome in children: new aspects on pathogenesis and treatment. Minerva Pediatr 64:197–203
Bamgbola O (2016) Metabolic consequences of modern immunosuppressive agents in solid organ transplantation. Ther Adv Endocrinol Metab 7:110–127
Latta K, von Schnakenburg C, Ehrich JH (2001) A meta-analysis of cytotoxic treatment for frequently relapsing nephrotic syndrome in children. Pediatr Nephrol 16:271–282
Esfahani ST, Madani A, Asgharian F, Ataei N, Roohi A, Moghtaderi M, Rahimzadeh P, Moradinejad MH (2011) Clinical course and outcome of children with steroid-sensitive nephrotic syndrome. Pediatr Nephrol 26:1089–1093
van Husen M, Kemper MJ (2011) New therapies in steroid-sensitive and steroid-resistant idiopathic nephrotic syndrome. Pediatr Nephrol 26:881–892
de Mello VR, Rodrigues MT, Mastrocinque TH, Martins SP, de Andrade OV, Guidoni EB, Scheffer DK, Martini Filho D, Toporovski J, Benini V (2010) Mycophenolate mofetil in children with steroid/cyclophosphamide-resistant nephrotic syndrome. Pediatr Nephrol 25:453–460
Gargah TT, Lakhoua MR (2011) Mycophenolate mofetil in treatment of childhood steroid-resistant nephrotic syndrome. J Nephrol 24:203–207
Hodson EM, Wong SC, Willis NS, Craig JC (2016) Interventions for idiopathic steroid-resistant nephrotic syndrome in children. Cochrane Database Syst Rev 10:CD003594
Mahmoud I, Basuni F, Sabry A, El-Husseini A, Hassan N, Ahmad NS, Elbaz M, Moustafa F, Sobh M (2005) Single-center experience with cyclosporine in 106 children with idiopathic focal segmental glomerulosclerosis. Nephrol Dial Transplant 20:735–742
El-Husseini A, El-Basuony F, Mahmoud I, Sheashaa H, Sabry A, Hassan R, Taha N, Hassan N, Sayed-Ahmad N, Sobh M (2005) Long-term effects of cyclosporine in children with idiopathic nephrotic syndrome: a single-center experience. Nephrol Dial Transplant 20:2433–2438
Ishikura K, Yoshikawa N, Nakazato H, Sasaki S, Iijima K, Nakanishi K, Matsuyama T, Ito S, Yata N, Ando T, Honda M, Japanese Study Group of Renal Disease in Children (2012) Two-year follow-up of a prospective clinical trial of cyclosporine for frequently relapsing nephrotic syndrome in children. Clin J Am Soc Nephrol 7:1576–1583
Kim JH, Park SJ, Yoon SJ, Lim BJ, Jeong HJ, Lee JS, Kim PK, Shin JI (2011) Predictive factors for cyclosporine-associated nephrotoxicity in children with minimal change nephrotic syndrome. J Clin Pathol 64:516–519
Hulton SA, Neuhaus TJ, Dillon MJ, Barratt TM (1994) Long-term cyclosporine a treatment of minimal-change nephrotic syndrome of childhood. Pediatr Nephrol 8:401–403
Kamei K, Ito S, Nozu K, Fujinaga S, Nakayama M, Sako M, Saito M, Yoneko M, Iijima K (2009) Single dose of rituximab for refractory steroid-dependent nephrotic syndrome in children. Pediatr Nephrol 24:1321–1328
Zhao Z, Liao G, Li Y, Zhou S, Zoua H (2015) The efficacy and safety of rituximab in treating childhood refractory nephrotic syndrome: a meta-analysis. Sci Rep 5:8219. https://doi.org/10.1038/srep08219
Maratea D, Bettio M, Corti MG, Montini G, Venturini F (2016) The efficacy and safety of rituximab in treating childhood nephrotic syndrome: an Italian perspective. Ital J Pediatr 42:63. https://doi.org/10.1186/s13052-016-0271-6
Ruggenenti P, Ruggiero B, Cravedi P, Vivarelli M, Massella L, Marasà M, Chianca A, Rubis N, Ene-Iordache B, Rudnicki M, Pollastro RM, Capasso G, Pisani A, Pennesi M, Emma F, Remuzzi G (2014) Rituximab in Nephrotic syndrome of steroid-dependent or frequently relapsing minimal change disease or focal segmental Glomerulosclerosis (NEMO) study group. Rituximab in steroid-dependent or frequently relapsing idiopathic nephrotic syndrome. J Am Soc Nephrol 25:850–863
Iijima K, Sako M, Nozu K, Mori R, Tuchida N, Kamei K, Miura K, Aya K, Nakanishi K, Ohtomo Y, Takahashi S, Tanaka R, Kaito H, Nakamura H, Ishikura K, Ito S, Ohashi Y (2014) Rituximab for childhood-onset refractory Nephrotic syndrome (RCRNS) study group. Rituximab for childhood-onset, complicated, frequently relapsing nephrotic syndrome or steroid-dependent nephrotic syndrome: a multicenter, double-blind, randomized, placebo-controlled trial. Lancet 384:1273–1281
Takura T, Takei T, Nitta K (2017) Cost-effectiveness of administering Rituximab for steroid-dependent Nephrotic syndrome and frequently relapsing Nephrotic syndrome: a preliminary study in Japan. Sci Rep 7:46036. https://doi.org/10.1038/srep46036
Van Horebeek I, Knops N, Van Dyck M, Levtchenko E, Mekahli D (2017) Rituximab in children with steroid-dependent nephrotic syndrome: experience of a tertiary center and review of the literature. Acta Clin Belg 72:147–155
Niu XL, Hao S, Wang P, Zhang W, Guo GM, Wu Y, Kuang XY, Zhu GH, Huang WY (2016) Single dose of rituximab in children with steroid-dependent minimal change nephrotic syndrome. Biomed Rep 5:237–242
Gulati A, Sinha A, Jordan SC, Hari P, Dinda AK, Sharma S, Srivastava RN, Moudgil A, Bagga A (2010) Efficacy and safety of treatment with rituximab for difficult steroid-resistant and -dependent nephrotic syndrome: multicentric report. Clin J Am Soc Nephrol 5:2207–2212
Mishra K, Ramachandran S, Firdaus S, Rath B (2015) The impact of pediatric nephrotic syndrome on parents' health-related quality of life and family functioning: an assessment made by the PedsQL 4.0 family impact module. Saudi J Kidney Dis Transpl 26:285–292
Santoro D, Pellicanò V, Visconti L, Trifirò G, Cernaro V, Buemi M (2015) Monoclonal antibodies for renal diseases: current concepts and ongoing treatments. Expert Opin Biol Ther 15:1119–1143
Cravedi P, Remuzzi G, Ruggenenti P (2014) Rituximab in primary membranous nephropathy: first-line therapy, why not? Nephron Clin Pract 128:261–269
Acknowledgements
We thank Dr. Susan Gottlieb and Dr. Fasika Tedla for editorial assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Iorember, F., Aviles, D., Kallash, M. et al. Cost analysis on the use of rituximab and calcineurin inhibitors in children and adolescents with steroid-dependent nephrotic syndrome. Pediatr Nephrol 33, 261–267 (2018). https://doi.org/10.1007/s00467-017-3789-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-017-3789-y