Abstract
Background
The introduction of laparoscopy in 1989 revolutionized surgical practices, reducing post-operative complications, and enhancing outcomes. Despite its benefits, limitations in laparoscopic tools have led to continued use of open surgery. Robotic-assisted surgery emerged to address these limitations, but its adoption trends and potential impact on open and laparoscopic surgery require analysis.
Methods
A retrospective analysis used the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) databases from 2012 to 2021. The study encompassed various abdominal procedures, employing Vector Autoregressive (VAR) models to analyze the dynamic relationships between surgical techniques. The models predicted future trends in open, laparoscopic, and robotic surgery until Q2 of 2025.
Results
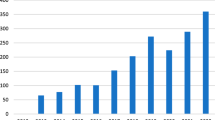
The analysis included 360,171 patients across diverse procedures. In urology, robotic surgery dominated prostatectomies (83.1% in 2021) and nephrectomies (55.1% in 2021), while the open approach remained the predominant surgical technique for cystectomies (72.5% in 2021). In general surgery, robotic colectomies were forecasted to surpass laparoscopy, becoming the primary approach by 2024 (45.7% in 2025). Proctectomies also showed a shift towards robotic surgery, predicted to surpass laparoscopy and open surgery by 2025 (32.3%). Pancreatectomies witnessed a steady growth in robotic surgery, surpassing laparoscopy in 2021, with forecasts indicating further increase. While hepatectomies remained predominantly open (70.0% in 2025), esophagectomies saw a rise in robotic surgery, predicted to become the primary approach by 2025 (52.3%).
Conclusions
The study suggests a transformative shift towards robotic-assisted surgery, poised to dominate various minimally invasive procedures. The forecasts indicate that robotic surgery may surpass laparoscopy and open surgery in colectomies, proctectomies, pancreatectomies, and esophagectomies by 2025. This anticipated change emphasizes the need for proactive adjustments in surgical training programs to align with evolving surgical practices. The findings have substantial implications for future healthcare practices, necessitating a balance between traditional laparoscopy and the burgeoning role of robotic-assisted surgery.





Similar content being viewed by others
References
Brunt LM (2015) SAGES presidential address: a SAGES Magical Mystery Tour. Surg Endosc 29(12):3423–3431. https://doi.org/10.1007/s00464-015-4524-z
Perissat J, Belliard R, Collet D (1989) Lithiase vesiculaire: lithotritie interne sous laparoscopie: technique personnelle. Chirurgie, Paris, p 115
Reynolds W Jr (2001) The first laparoscopic cholecystectomy. JSLS 5(1):89–94
Brunt L, Greene F, Forde K, Perissat J (2013) SAGES video classics. Surg Endosc 27(12):4581–4588. https://doi.org/10.1007/s00464-013-3131-0
Nezhat C, Pennington E, Nezhat F, Silfen SL (1991) Laparoscopically assisted anterior rectal wall resection and reanastomosis for deeply infiltrating endometriosis. Surg Laparosc Endosc Percutaneous Tech 1(2):106–108
Kelley WE Jr (2008) The evolution of laparoscopy and the revolution in surgery in the decade of the 1990s. JSLS 12(4):351–357
Litynski GS (1996) Highlights in the history of laparoscopy: the development of laparoscopic techniques—a cumulative effort of internists, gynecologists, and surgeons. Barbara Bernert Verlag, Frankfurt
Redwine DB, Sharpe DR (1991) Laparoscopic segmental resection of the sigmoid colon for endometriosis. J Laparoendosc Surg 1(4):217–220
Fowler DL, White SA (1991) Laparoscopy-assisted sigmoid resection. Surg Laparosc Endosc 1(3):183–188
Jacobs M, Verdeja J, Goldstein H (1991) Minimally invasive colon resection (laparoscopic colectomy). Surg Laparosc Endosc Percutaneous Tech 1(3):144–150
Perissat J, Collet D, Monguillon N (1998) Advances in laparoscopic surgery. Digestion 59(5):606–618
Bailey RW, Flowers JL, Graham SM, Zucker KA (1991) Combined laparoscopic cholecystectomy and selective vagotomy. Surg Laparosc Endosc 1(1):45–49
Katkhouda N, Mouiel J (1991) A new technique of surgical treatment of chronic duodenal ulcer without laparotomy by videocoelioscopy. Am J Surg 161(3):361–364
Clayman RV, Kavoussi LR, Soper NJ, Dierks SM, Meretyk S, Darcy MD et al (1991) Laparoscopic nephrectomy. N Engl J Med 324(19):1370–1371
Tierney J, Kusminsky R, Boland J, Oliver R Jr (1991) Laparoscopic pelvic lymph node dissection. West Va Med J 87(4):151–152
Flowers JL, Feldman J, Jacobs SC (1991) Laparoscopic pelvic lymphadenectomy. Surg Laparosc Endosc Percutaneous Tech 1(2):62–70
Kovac SR, Cruikshank SH, Retto HF (1990) Laparoscopy-assisted vaginal hysterectomy. J Gynecol Surg 6(3):185–193
Agha R, Muir G (2003) Does laparoscopic surgery spell the end of the open surgeon? J R Soc Med 96(11):544–546. https://doi.org/10.1177/014107680309601107
Jiménez-Rodríguez RM, Rubio-Dorado-Manzanares M, Díaz-Pavón JM, Reyes-Díaz ML, Vazquez-Monchul JM, Garcia-Cabrera AM et al (2016) Learning curve in robotic rectal cancer surgery: current state of affairs. Int J Colorectal Dis 31(12):1807–1815. https://doi.org/10.1007/s00384-016-2660-0
Feng Q, Yuan W, Li T, Tang B, Jia B, Zhou Y et al (2022) Robotic versus laparoscopic surgery for middle and low rectal cancer (REAL): short-term outcomes of a multicentre randomised controlled trial. Lancet Gastroenterol Hepatol 7(11):991–1004. https://doi.org/10.1016/s2468-1253(22)00248-5
Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ et al (2005) Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol 6(7):477–484. https://doi.org/10.1016/s1470-2045(05)70221-7
Bonjer HJ, Deijen CL, Abis GA, Cuesta MA, van der Pas MHGM, de Lange-de Klerk ESM et al (2015) A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med 372(14):1324–1332. https://doi.org/10.1056/NEJMoa1414882
van der Veen A, Brenkman HJF, Seesing MFJ, Haverkamp L, Luyer MDP, Nieuwenhuijzen GAP et al (2021) Laparoscopic versus open gastrectomy for gastric cancer (LOGICA): a multicenter randomized clinical trial. J Clin Oncol 39(9):978–989. https://doi.org/10.1200/jco.20.01540
Jiang WZ, Xu JM, Xing JD, Qiu HZ, Wang ZQ, Kang L et al (2022) Short-term outcomes of laparoscopy-assisted vs open surgery for patients with low rectal cancer: the LASRE randomized clinical trial. JAMA Oncol 8(11):1607–1615. https://doi.org/10.1001/jamaoncol.2022.4079
Poves I, Burdío F, Morató O, Iglesias M, Radosevic A, Ilzarbe L et al (2018) Comparison of perioperative outcomes between laparoscopic and open approach for pancreatoduodenectomy: the PADULAP randomized controlled trial. Ann Surg 268(5):731–739. https://doi.org/10.1097/sla.0000000000002893
Elm EV, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP (2007) Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 335(7624):806–808. https://doi.org/10.1136/bmj.39335.541782.AD
Lütkepohl H (2006) New introduction to multiple time series analysis, 1st edn. Springer, Berlin
Hamilton JD (1994) Time series analysis. Princeton University Press, Princeton
Johansen S (1995) Likelihood-based inference in cointegrated vector autoregressive models. Oxford University Press, Oxford
Schulz KF, Altman DG, Moher D (2010) CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ 340:c332. https://doi.org/10.1136/bmj.c332
Quenouille MH (1958) The analysis of multiple time-series. Griffin, Duxbury
Sims CA (1980) Macroeconomics and reality. Econometrica 48(1):1–48. https://doi.org/10.2307/1912017
Granger CWJ (1981) Some properties of time series data and their use in econometric model specification. J Econom 16(1):121–130. https://doi.org/10.1016/0304-4076(81)90079-8
Engle RF, Granger CWJ (1987) Co-integration and error correction: representation, estimation, and testing. Econometrica 55(2):251–276. https://doi.org/10.2307/1913236
Shen Y, Giannakis GB, Baingana B (2019) Nonlinear structural vector autoregressive models with application to directed brain networks. IEEE Trans Signal Process 67(20):5325–5339. https://doi.org/10.1109/tsp.2019.2940122
Lu F, Zheng Y, Cleveland H, Burton C, Madigan D (2018) Bayesian hierarchical vector autoregressive models for patient-level predictive modeling. PLoS ONE 13(12):e0208082. https://doi.org/10.1371/journal.pone.0208082
Matsukawa S, Wada T (1997) Vector autoregressive modeling for analyzing feedback regulation between heart rate and blood pressure. Am J Physiol 273(1 Pt 2):H478–H486. https://doi.org/10.1152/ajpheart.1997.273.1.H478
Ito K, Wada T, Makimura H, Matsuoka A (1998) Vector autoregressive modeling analysis of frequently sampled oral glucose tolerance test results. 1. A new method for quantifying insulin resistance and secretion. Keio J Med 47(1):28–36. https://doi.org/10.2302/kjm.47.28
Ren W, Fu X, Tarimo CS, Kasanga M, Wang Y, Wu J (2021) The scale and structure of government financial investment in traditional medicine based on optimal efficiency: evidence from public traditional Chinese medicine hospitals (PTHs) of Henan province, China. BMC Health Serv Res 21(1):182. https://doi.org/10.1186/s12913-021-06185-x
Shimamura T, Imoto S, Yamaguchi R, Fujita A, Nagasaki M, Miyano S (2009) Recursive regularization for inferring gene networks from time-course gene expression profiles. BMC Syst Biol 3:41. https://doi.org/10.1186/1752-0509-3-41
Marohn MR, Hanly EJ (2004) Twenty-first century surgery using twenty-first century technology: surgical robotics. Curr Surg 61(5):466–473. https://doi.org/10.1016/j.cursur.2004.03.009
Parekh DJ, Reis IM, Castle EP, Gonzalgo ML, Woods ME, Svatek RS et al (2018) Robot-assisted radical cystectomy versus open radical cystectomy in patients with bladder cancer (RAZOR): an open-label, randomised, phase 3, non-inferiority trial. Lancet 391(10139):2525–2536. https://doi.org/10.1016/s0140-6736(18)30996-6
Venkatramani V, Reis IM, Castle EP, Gonzalgo ML, Woods ME, Svatek RS et al (2020) Predictors of recurrence, and progression-free and overall survival following open versus robotic radical cystectomy: analysis from the RAZOR trial with a 3-year followup. J Urol 203(3):522–529. https://doi.org/10.1097/ju.0000000000000565
Khan MS, Omar K, Ahmed K, Gan C, Van Hemelrijck M, Nair R et al (2020) Long-term oncological outcomes from an early phase randomised controlled three-arm trial of open, robotic, and laparoscopic radical cystectomy (CORAL). Eur Urol 77(1):110–118. https://doi.org/10.1016/j.eururo.2019.10.027
Ballantyne GH (2002) The pitfalls of laparoscopic surgery: challenges for robotics and telerobotic surgery. Surg Laparosc Endosc Percutan Tech 12(1):1–5. https://doi.org/10.1097/00129689-200202000-00001
El Aziz MAA, Grass F, Behm KT, Shawki S, D’Angelo AL, Mathis KL et al (2021) Trends of complications and innovative techniques’ utilization for colectomies in the United States. Updates Surg 73(1):101–110. https://doi.org/10.1007/s13304-020-00862-y
Larson DW, Nelson H (2004) Laparoscopic colectomy for cancer. J Gastrointest Surg 8(5):636–642. https://doi.org/10.1016/j.gassur.2004.03.002
Achilli P, Grass F, Larson DW (2021) Robotic surgery for rectal cancer as a platform to build on: review of current evidence. Surg Today 51(1):44–51. https://doi.org/10.1007/s00595-020-02008-4
Law KE, Lowndes BR, Kelley SR, Blocker RC, Larson DW, Hallbeck MS et al (2020) NASA-task load index differentiates surgical approach: opportunities for improvement in colon and rectal surgery. Ann Surg 271(5):906–912
Crippa J, Grass F, Dozois EJ, Mathis KL, Merchea A, Colibaseanu DT et al (2021) Robotic surgery for rectal cancer provides advantageous outcomes over laparoscopic approach: results from a large retrospective cohort. Ann Surg 274(6):e1218–e1222
Casarin J, Multinu F, Ubl DS, Dowdy SC, Cliby WA, Glaser GE et al (2018) Adoption of minimally invasive surgery and decrease in surgical morbidity for endometrial cancer treatment in the United States. Obstet Gynecol 131(2):304–311. https://doi.org/10.1097/aog.0000000000002428
Casarin J, Song C, Multinu F, Cappuccio S, Liu E, Butler KA et al (2020) Implementing robotic surgery for uterine cancer in the United States: better outcomes without increased costs. Gynecol Oncol 156(2):451–458. https://doi.org/10.1016/j.ygyno.2019.11.016
Leitao MM Jr, Kreaden US, Laudone V, Park BJ, Pappou EP, Davis JW et al (2023) The RECOURSE study: long-term oncologic outcomes associated with robotically assisted minimally invasive procedures for endometrial, cervical, colorectal, lung, or prostate cancer: a systematic review and meta-analysis. Ann Surg 277(3):387–396. https://doi.org/10.1097/sla.0000000000005698
Steffens D, Thanigasalam R, Leslie S, Maneck B, Young JM, Solomon M (2017) Robotic surgery in uro-oncology: a systematic review and meta-analysis of randomized controlled trials. Urology 106:9–17. https://doi.org/10.1016/j.urology.2017.03.015
Nickel F, Haney CM, Kowalewski KF, Probst P, Limen EF, Kalkum E et al (2020) Laparoscopic versus open pancreaticoduodenectomy: a systematic review and meta-analysis of randomized controlled trials. Ann Surg 271(1):54–66. https://doi.org/10.1097/sla.0000000000003309
Venkat R, Edil BH, Schulick RD, Lidor AO, Makary MA, Wolfgang CL (2012) Laparoscopic distal pancreatectomy is associated with significantly less overall morbidity compared to the open technique: a systematic review and meta-analysis. Ann Surg 255(6):1048–1059. https://doi.org/10.1097/SLA.0b013e318251ee09
Azagra JS, Goergen M, Gilbart E, Jacobs D (1996) Laparoscopic anatomical (hepatic) left lateral segmentectomy-technical aspects. Surg Endosc 10(7):758–761. https://doi.org/10.1007/bf00193052
Nguyen KT, Gamblin TC, Geller DA (2009) World review of laparoscopic liver resection-2,804 patients. Ann Surg 250(5):831–841. https://doi.org/10.1097/SLA.0b013e3181b0c4df
Belli G, Fantini C, D’Agostino A, Cioffi L, Langella S, Russolillo N et al (2007) Laparoscopic versus open liver resection for hepatocellular carcinoma in patients with histologically proven cirrhosis: short- and middle-term results. Surg Endosc 21(11):2004–2011. https://doi.org/10.1007/s00464-007-9503-6
Cherqui D (2003) Laparoscopic liver resection. Br J Surg 90(6):644–646. https://doi.org/10.1002/bjs.4197
Giulianotti PC, Sbrana F, Coratti A, Bianco FM, Addeo P, Buchs NC et al (2011) Totally robotic right hepatectomy: surgical technique and outcomes. Arch Surg 146(7):844–850. https://doi.org/10.1001/archsurg.2011.145
Liu R, Wakabayashi G, Kim HJ, Choi GH, Yiengpruksawan A, Fong Y et al (2019) International consensus statement on robotic hepatectomy surgery in 2018. World J Gastroenterol 25(12):1432–1444. https://doi.org/10.3748/wjg.v25.i12.1432
Giulianotti PC, Bianco FM, Daskalaki D, Gonzalez-Ciccarelli LF, Kim J, Benedetti E (2016) Robotic liver surgery: technical aspects and review of the literature. Hepatobiliary Surg Nutr 5(4):311–321. https://doi.org/10.21037/hbsn.2015.10.05
Swanstrom LL, Hansen P (1997) Laparoscopic total esophagectomy. Arch Surg 132(9):943–949. https://doi.org/10.1001/archsurg.1997.01430330009001
Bonavina L, Incarbone R, Bona D, Peracchia A (2004) Esophagectomy via laparoscopy and transmediastinal endodissection. J Laparoendosc Adv Surg Tech A 14(1):13–16. https://doi.org/10.1089/109264204322862298
Luketich JD, Alvelo-Rivera M, Buenaventura PO, Christie NA, McCaughan JS, Litle VR et al (2003) Minimally invasive esophagectomy: outcomes in 222 patients. Ann Surg 238(4):486–494; discussion 94–95. https://doi.org/10.1097/01.sla.0000089858.40725.68
Biere SS, van Berge Henegouwen MI, Maas KW, Bonavina L, Rosman C, Garcia JR et al (2012) Minimally invasive versus open oesophagectomy for patients with oesophageal cancer: a multicentre, open-label, randomised controlled trial. Lancet 379(9829):1887–1892
van Workum F, Stenstra M, Berkelmans GHK, Slaman AE, van Berge Henegouwen MI, Gisbertz SS et al (2019) Learning curve and associated morbidity of minimally invasive esophagectomy: a retrospective multicenter study. Ann Surg 269(1):88–94. https://doi.org/10.1097/sla.0000000000002469
van der Sluis PC, van der Horst S, May AM, Schippers C, Brosens LAA, Joore HCA et al (2019) Robot-assisted minimally invasive thoracolaparoscopic esophagectomy versus open transthoracic esophagectomy for resectable esophageal cancer: a randomized controlled trial. Ann Surg 269(4):621–630. https://doi.org/10.1097/sla.0000000000003031
van Boxel GI, Kingma BF, Voskens FJ, Ruurda JP, van Hillegersberg R (2020) Robotic-assisted minimally invasive esophagectomy: past, present and future. J Thorac Dis 12(2):54–62. https://doi.org/10.21037/jtd.2019.06.75
Chao YK, Li ZG, Wen YW, Kim DJ, Park SY, Chang YL et al (2019) Robotic-assisted esophagectomy vs video-assisted thoracoscopic esophagectomy (REVATE): study protocol for a randomized controlled trial. Trials 20(1):346. https://doi.org/10.1186/s13063-019-3441-1
Bianchi PP, Salaj A, Rocco B, Formisano G (2023) First worldwide report on Hugo RAS™ surgical platform in right and left colectomy. Updates Surg 75(3):775–780. https://doi.org/10.1007/s13304-023-01489-5
Raffaelli M, Gallucci P, Voloudakis N, Pennestrì F, De Cicco R, Arcuri G et al (2023) The new robotic platform Hugo™ RAS for lateral transabdominal adrenalectomy: a first world report of a series of five cases. Updates Surg 75(1):217–225. https://doi.org/10.1007/s13304-022-01410-6
Rocco B, Turri F, Sangalli M, Assumma S, Piacentini I, Grasso A et al (2023) Robot-assisted radical prostatectomy with the Versius robotic surgical system: first description of a clinical case. Eur Urol Open Sci 48:82–83. https://doi.org/10.1016/j.euros.2022.11.019
Monterossi G, Pedone Anchora L, Gueli Alletti S, Fagotti A, Fanfani F, Scambia G (2022) The first European gynaecological procedure with the new surgical robot Hugo™ RAS A total hysterectomy and salpingo-oophorectomy in a woman affected by BRCA-1 mutation. Facts Views Vis Obgyn 14(1):91–94. https://doi.org/10.52054/fvvo.14.1.014
Mottaran A, Bravi CA, Sarchi L, Paciotti M, Nocera L, Piro A et al (2023) Robot-assisted sacropexy with the novel HUGO robot-assisted surgery system: initial experience and surgical setup at a tertiary referral robotic center. J Endourol 37(1):35–41. https://doi.org/10.1089/end.2022.0495
El Dahdah J, Halabi M, Kamal J, Zenilman ME, Moussa H (2023) Initial experience with a novel robotic surgical system in abdominal surgery. J Robot Surg 17(3):841–846. https://doi.org/10.1007/s11701-022-01471-0
Wehrmann S, Tischendorf K, Mehlhorn T, Lorenz A, Gündel M, Rudolph H et al (2023) Clinical implementation of the Versius robotic surgical system in visceral surgery—a single centre experience and review of the first 175 patients. Surg Endosc 37(1):528–534. https://doi.org/10.1007/s00464-022-09526-x
Martin JR, Stefanidis D, Dorin RP, Goh AC, Satava RM, Levy JS (2021) Demonstrating the effectiveness of the fundamentals of robotic surgery (FRS) curriculum on the RobotiX Mentor Virtual Reality Simulation Platform. J Robot Surg 15(2):187–193. https://doi.org/10.1007/s11701-020-01085-4
Acknowledgements
The American College of Surgeons National Surgical Quality Improvement Program and the hospitals participating in the ACS NSQIP are the sources of the data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors.
Funding
This research did not receive external funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Davide Ferrari, Dr. Tommaso Violante, Dr. Marco Novelli, Prof. Patrick Starlinger, Prof. Rory Smoot, Prof. Janani Reisenauer and Prof. David Larson have no conflict of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ferrari, D., Violante, T., Novelli, M. et al. The death of laparoscopy. Surg Endosc (2024). https://doi.org/10.1007/s00464-024-10774-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00464-024-10774-2