Abstract
Background
Minimally invasive total gastrectomy (MITG) is a mainstay for curative treatment of patients with gastric cancer. To define and standardize optimal surgical techniques and further improve clinical outcomes through the enhanced MITG surgical quality, there must be consensus on the key technical steps of lymphadenectomy and anastomosis creation, which is currently lacking. This study aimed to determine an expert consensus from an international panel regarding the technical aspects of the performance of MITG for oncological indications using the Delphi method.
Methods
A 100-point scoping survey was created based on the deconstruction of MITG into its key technical steps through local and international expert opinion and literature evidence. An international expert panel comprising upper gastrointestinal and general surgeons participated in multiple rounds of a Delphi consensus. The panelists voted on the issues concerning importance, difficulty, or agreement using an online questionnaire. A priori consensus standard was set at > 80% for agreement to a statement. Internal consistency and reliability were evaluated using Cronbach's α.
Results
Thirty expert upper gastrointestinal and general surgeons participated in three online Delphi rounds, generating a final consensus of 41 statements regarding MITG for gastric cancer. The consensus was gained from 22, 12, and 7 questions from Delphi rounds 1, 2, and 3, which were rephrased into the 41 statetments respectively. For lymphadenectomy and aspects of anastomosis creation, Cronbach’s α for round 1 was 0.896 and 0.886, and for round 2 was 0.848 and 0.779, regarding difficulty or importance.
Conclusions
The Delphi consensus defined 41 steps as crucial for performing a high-quality MITG for oncological indications based on the standards of an international panel. The results of this consensus provide a platform for creating and validating surgical quality assessment tools designed to improve clinical outcomes and standardize surgical quality in MITG.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Gastric cancer accounts for Europe's fourth highest cause of cancer-related deaths, and its incidence is projected to rise globally [1,2,3]. The mainstay of curative treatment is surgical resection with corresponding en-bloc D2 lymphadenectomy (LND) [4, 5]. International adoption of minimally invasive techniques in treating gastric cancer has been observed [6,7,8,9,10,11]. First performed by Kitano [12], it has subsequently been evaluated in several large-scale randomized controlled trials (RCTs) in the Asian continent [13,14,15,16] and corroborated in high-quality European population-based studies and RCTs [17, 18]. Outcomes from these studies have advocated the use of minimally invasive total gastrectomy (MITG) by demonstrating superiority in short- and long-term general surgical outcomes such as post-operative length of stay [4, 15, 19] and equivalence of MITG for oncological specific outcomes. Multicenter studies such as the LOGICA and the STOMACH trials demonstrated the feasibility and oncological efficacy of MITG compared to open surgery and subsequently recommended this approach to improve long-term outcomes [17, 20,21,22].
For oncological indications, key technical steps specific to gastric cancer must be respected, such as the extent and the number of lymph nodes harvested and achieving an R0 resection margin. Therefore, MITG for oncological treatment is considered an advanced minimally invasive procedure as it involves achieving complete en-bloc dissection of lymph node stations and creating a high-quality anastomosis [23, 24]. The lack of compliance with the D2 LND in MITG has been reported in several publications and can negatively impact patient outcomes [18, 25, 26]. Combined with the technical challenges, there is heterogeneity within techniques and steps surgeons undertake to achieve a complete oncological MITG. These variations can impact clinical outcomes in patients, complicate reporting and comparing outcomes between studies, hinder the assessment of surgical quality, and pose challenges to the teaching and training of MITG.
The aim of this study was to develop an international expert consensus on the technical steps of LND and general aspects of anastomosis creation in MITG for oncological indications using the Delphi method. The consensus will inform the development of surgical quality assessment tools for MITG and the creation of a technical framework to aid skill acquisition and surgeon training. The consensus will also enable benchmarking of this procedure so practicing surgeons and certifying bodies are ensured that MITG is being performed competently and, most importantly, safely [27].
Materials and methods
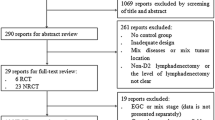
This study utilized the Delphi method to achieve consensus by soliciting international expert opinion on essential technical steps in LND and general aspects of anastomosis creation required to perform MITG for oncological indications (Fig. 1). The study utilized the AGREE II framework for the assessment of the methodological quality of practice guidelines (Appendices 1 and 2). AGREE II comprises 23 items organized into six quality domains: (i) scope and purpose; (ii) stakeholder involvement; (iii) rigor of development; (iv) clarity of presentation; (v) applicability; and (vi) editorial independence that targets various aspects of practice guideline quality [28]. The outcomes of this study were to create consensus on the most important steps of the operation required to achieve optimal oncological outcomes, minimize technical heterogeneity, and inform the training of future surgeons.
The Delphi method
The Delphi method was first developed by the RAND Corporation in 1948. It is a structured and iterative process used to acquire knowledge and opinions from experts on a selected topic [29, 30]. The major advantages of using the Delphi method are that a wide range of views can be obtained, which enables the collation of international opinions while being cost-effective and eliminating the need to travel. It also provides a platform for experts to revise their initial opinions based on the feedback from the group, fostering convergence and consensus-building. The anonymous nature of the Delphi method also ensures that a single dominant group member does not inordinately influence the group's outcome [31]. The Delphi method has been widely used in determining guidelines and recommendations in the medical field, especially on topics that lack RCTs as evidence [27, 32,33,34].
Creation of MITG scoping questionnaire
A novel 100-step scoping questionnaire was created by deconstructing the entire MITG procedure into key technical steps focusing on D2 LND and general aspects of anastomosis creation for oncological indications (see Appendices 3, 4, and 5 for the complete questionnaire). The deconstruction of procedures into their individual elements has been described as a validated and effective strategy [35]. The MITG sub-steps were created based on author group consensus, expert supervision from upper gastrointestinal (UGI) surgical faculty at the University Medical Center Hamburg-Eppendorf, Germany, and the University of Oxford, UK, and peer-reviewed published literature. The survey was refined through iterations. The final version consisted of questions related to the demographics of the expert panel, and the remaining questions were categorized into two main groups: questions surrounding LND and general aspects associated with the creation of the anastomosis.
Selection of experts
Expert surgeons in UGI were identified globally to represent an international consensus on performing MITG in Asian and European countries. Experts were selected based on the following inclusion criteria: high case volume defined as > 20 cases per year in their local institution, national or international board accreditations, and individual credentialing of surgeons based on their number of index cases performed as well as specific expertise in methodology. All panelists were identified as experts in their clinical field and currently practicing minimally invasive surgeons. General surgeons were also considered for the expert panel since some countries do not differentiate between subspecialties despite having UGI high case volume centers. In these cases, the determining inclusion factors were the high case volume center and the UGI expertise of the panelists. Thirty participants representing 12 countries were initially approached through e-mail with personalized invitation letters explaining the project. The membership of the expert panel was anonymized.
Delphi rounds
Statements generated in the scoping questionnaire were presented to the expert panel via an online survey on SurveyMonkey® (USA). The questions were divided into three domains depending on the type of possible answers: questions with a 5-point Likert scale regarding the importance of the subject, questions with a 5-point Likert scale regarding the difficulty of the subject, and binary ‘yes’ or ‘no’ questions. An a priori consensus standard was set at > 80% if the panel deemed the statement important and < 40% unimportant. Panelists were also encouraged to suggest additional statements or modifications to the statements in free text fields. Rounds 2 and 3 questions were modified according to the experts' comments and suggestions from previous rounds. Each round was closed once 90% of the experts had responded. Results were analyzed, and those questions that failed to reach consensus were evaluated, rephrased if necessary, and distributed to the same experts for rounds 2 and 3 of the survey, in addition to novel statements generated from the previous rounds. The survey was closed when all responses reached consensus or agreed on non-consensus.
Statistical analysis
Statistical analysis and descriptive statistics were performed using the SPSS software (version 25.0, IBM SPSS Inc., Chicago, Illinois, USA), and data were given as absolute frequency and mean ± standard deviation. Cronbach's α was calculated to determine internal consistency.
Results
Thirty UGI/general surgery experts were invited to participate in the Delphi survey. Twenty-eight (93.3%) experts across 12 countries completed the first, and 25 (83.3%) completed the second and third Delphi round. The demographic characteristics of the experts are presented in Table 1.
Seventeen out of 30 experts were UGI surgeons (56.7%), and 13 (43.3%) were general surgeons. The majority of experts had more than 20 years experience in MIS.
The total time needed to complete all three rounds was seven months (11/2022–06/2023). In all three groups, there were 100 questions, 65 with 5-Likert scale answers regarding the importance, 19 with 5-Likert scale answers regarding the difficulty, and 16 with yes or no answers (Table 2).
The Cronbach's α for round 1 questions regarding importance (n = 46, 66.7%) was 0.886. For questions regarding the difficulty (n = 12, 17.4%) in round 1, Cronbach's α was 0.896. In round 2, Cronbach's α was 0.779 for questions regarding importance (n = 19, 59.4%) and 0.848 for questions regarding difficulty (n = 7, 21.9%) (Table 2).
Consensus was reached from 22 questions from round 1, 12 from round 2, and 7 from round 3 (Table 2). These were rephrased into 41 consensus statements regarding LND and general aspects of anastomosis creation in MITG (Table 3). The 41 statements were divided into general aspects of the MITG (n = 2), key technical aspects of LND (n = 33), general aspects of LND in MITG (n = 1), and general aspects of anastomosis creation (n = 5) (Table 3).
Statements of non-consensus
A certain number of questions were excluded from rounds 1 and 2 due to either incorporation into the other questions or irrelevance (round 1 n = 10, round 2 n = 11).
Eight questions with a 5-point Likert scale on difficulty performing LND of stations 4sa, 5, 6, 7, 1, 2, 9, 8a, 12a, and 11d required rephrasing due to heterogeneity of answers after rounds 1 and 2 (Table 4). Five questions with a 5-point Likert scale regarding the importance of performing certain MITG steps did not reach an agreement after 3 Delphi rounds, and three questions regarding general aspects of the anastomosis creation with binary responses did not reach consensus (Table 4).
AGREE II checklist
Two independent assessors evaluated the methodological quality of the guidelines using the AGREE II checklist. Twenty-three items divided into six domains were evaluated based on the practice guidelines (Appendix 1). All domains had a score > 70% defined previously as a quality threshold (domain 1: 92%, domain 2: 78%, domain 3: 84%, domain 4: 92%, domain 5: 75% and domain 6: 96%) (Appendix 2).
Discussion
This is the first international Delphi consensus on the recommended technical steps regarding LND and general aspects of anastomosis creation in MITG for oncological indications. This study aimed to establish and summarize the current recommendations on technical steps required to achieve a high-quality MITG for gastric cancer, explicitly focusing on LND and general anastomosis creation. Thirty international UGI and general surgery experts from 12 countries participated in this study, answering 100 questions through 3 Delphi rounds, generating 41 final recommended statements. The study met the quality threshold of > 70% for all six domains of the AGREE II checklist [28].
The majority of the final consensus statements were attained in round 1 of the Delphi, with high interrater reliability and overall homogeneity in their MITG operating technique. This indicates there was general alignment among how experts perform MITG, validating the selection of our expert panel.
The results of this study identified several issues regarding the importance and perceived difficulty of performing LND in MITG. Statements that commonly reached consensus related to the importance of how to technically approach of the D2 LND steps. The areas of least consensus related to the perceived difficulty of performing LND of specific lymph node stations. For example, 12% of experts rated performing a sufficient LND along the proper hepatic artery (station 12a) as easy, whereas 12% reported it as very difficult. A potential reason for heterogeneous responses on LND difficulty could be the different experience levels of panelists not only with gastrectomy but also with other index procedures that involve similar operative steps or not, such as bariatric surgeries, hiatal hernia repairs, esophagectomies, or pancreatic surgeries, which might influence the difficulty perception of performing specific surgical steps in MITG. However, no difference in the difficulty statement was detected regarding the volume and experience of the panelists. The only ‘difficulty’ statement where the panelists reached agreement was that station 10 LND is extremely/very difficult, which correlates to MITG's challenges regarding the LND of the splenic hilum [36].
Other than defining aspects related to LND in MITG, it was important to determine the general aspects of the procedure, such as omentectomy and division of the gastrocolic ligament. Interestingly, the panelists agreed that performing omentectomy can be omitted in early tumor stages (T1/T2). However, the necessity of omentectomy in advanced stages (T3/T4) or irrespective of tumor stage did not reach consensus after three rounds despite having been recommended in many guidelines and available literature [37,38,39,40].
The final domain focused on general aspects of anastomosis creation in MITG. Due to the various technical approaches to performing the esophagojejunostomy in MITG, the statements focused on common facets of anastomosis creation rather than choosing one specific way of performing it. The panelists agreed that skillful, safe, efficient, tension- and torsion-free anastomosis is extremely or very important in MITG. The recommendation from round 3 that a frozen section should be performed if the tumor is perceived to be close to the resection margin also reached consensus (92%). However, the panelists could not agree on whether a frozen section should always be performed if the proximal resection margin was less than 6 cm (60% yes vs. 40% no) in round 2. Some surgical steps regarding anastomosis were still heterogenous among panelists, such as whether the R0 resection is oncologically acceptable irrespective of the resection margin distance after neoadjuvant therapy (68% yes vs. 32% no) and regarding the assessment of the perfusion of anastomosis. The panelists were asked whether the assessment of the perfusion of the anastomosis should be performed with indocyanine green fluorescence or a hyperspectral imaging camera, which revealed that 60% of experts stated that it should be performed and 40% of the panel reported it can be omitted. This result may reflect the relatively new use of such perfusion assessment tools in MITG, so the answers may change in the future to reflect the routine incorporation of these tools [41] in case scientific evidence can prove definitive advantages. Regarding the need for anastomosis assessment using an intraoperative leakage test, the panelists reached a consensus that it could be performed at the discretion of the operating surgeon to rule out leakage. This may reflect differences in clinical practice and the absence of evidence in favor of or against routine leak tests. This may also be a statistical problem since intraoperative detection of leaks represents a rather rare finding and thus may be difficult to handle statistically. On the other hand, leak tests may be of clinical value for detecting technical problems while not posing significant risks or added operative time or cost.
The strengths of this study are the solicitation of global expert opinion unifying views across Asia and Europe and the quality and experience of the experts taking part in this consensus. One of the advantages is the high expert response rate (93%) and low attrition rates (10%) between rounds and the high interrater agreement demonstrated by Cronbach's α, strengthening the content validity and effectiveness of the Delphi method. Furthermore, this study addressed a clinically important issue regarding MITG. Determining a sufficient level of agreement with performing an oncologically acceptable MITG is essential for several reasons. MITG is a complex surgical procedure that requires specialized knowledge and skills. The emphasis on compliance in D2 LND has been proven to be of great importance to patient outcomes [18, 25]. Obtaining a consensus from experts in the field ensures that the recommendations and guidelines for performing the procedure are based on the collective wisdom and experience of skilled surgeons. This helps establish a standard of care and minimizes the variability in surgical techniques, leading to standardized patient outcomes. The Delphi method also drives best practices in medicine since consensus-driven guidelines facilitate knowledge of the most effective and evidence-based approaches, leading to improved patient care. This also helps identify potential risks and develop strategies to mitigate them, thereby enhancing patient safety. By standardizing the procedure and promoting adherence to established guidelines, the quality of care provided to patients undergoing MITG can be improved, reducing the likelihood of adverse events and improving surgical safety.
Such consensus-based guidelines can be incorporated into training programs and surgical curricula to ensure that surgeons receive appropriate education and mentoring in MITG, fostering the development of competent and skilled practitioners. Most importantly, this research is essential for innovation. Delphi consensus can guide the direction of future studies, enabling the focus to shift toward the advancement of MITG. Additionally, consensus guidelines may promote innovation by encouraging the evaluation of new techniques, technologies, and approaches through well-designed research studies.
General limitations of the Delphi method and this study should be recognized. Although the Delphi method should be performed with anonymized panelists to mitigate potential bias and enhance quality and objectivity, this study required the identification of the panelists to ensure the participation of the uttermost experts in MITG. The Delphi method may also be susceptible to the ‘groupthink’ phenomena, where participants tend to conform to a dominant viewpoint or consensus rather than providing independent and diverse opinions. One way of mitigating this effect was the conscious decision to conduct the study online. However, this approach did hinder the establishment of meaningful discussions and clarifying responses on site, as panelists could not directly interact or engage in a real-time dialogue with each other or the researchers. Despite this Delphi consensus being created using a scoping strategy with international input, not all aspects of MITG have been addressed, for example, the optimal limb length and the preferences of exact anastomosis technique (e.g., handsewn versus circular stapler versus linear stapler technique) for anastomosis creation. Another limitation of this study is the lack of investigation about technical aspects or approaches; however, these were not the primary aim of the study, and they will be the object of further studies since the current study focused on oncological outcome and perioperative outcome with regards to general surgical technique.
The results of this study represent the first phase of the ANALYTIQs study that resulted from international collaboration in the EAES Research Sandpit in June 2022. The next step is creating a surgical quality assessment (SQA) tool and its application in video assessments of MITG. This will serve SQA in prospective and randomized studies to ensure optimized surgical performance [42]. The results of the applied SQA will also be used to develop artificial intelligence-based algorithms for automation of SQA. The long-term aims are to determine an SQA of this technique through video-based learning to ensure standardization and improve patient outcomes after MITG for oncological indications. Furthermore, the SQA tool could be used as an intraoperative guide for residents or young surgeons, with the final aim to shorten the learning curve and improve intra- and postoperative results. The predefined surgical steps that emphasize the most important aspects of LND of each lymph node station in MITG for gastric cancer could provide valuable structure in training young surgeons to master this procedure and ensure the best possible patient outcomes through technical impeccability.
In conclusion, this is the first study to determine the crucial technical steps in LND in MITG, deconstructing the integral elements within a complex minimally invasive procedure. It has identified the key technical steps of LND and general aspects of anastomosis creation required to perform adequate MITG for oncological indications by soliciting international expert opinion through a three-round Delphi consensus method. These statements should serve the standardization of the MITG and, through that, the improvement of oncological outcomes through adequate LND.
References
Wong MCS, Huang J, Chan PSF, Choi P, Lao XQ, Chan SM et al (2021) Global incidence and mortality of gastric cancer, 1980–2018. JAMA Netw Open 4(7):e2118457
Wang Y, Zhang L, Yang Y, Lu S, Chen H (2021) Progress of gastric cancer surgery in the era of precision medicine. Int J Biol Sci 17(4):1041–1049
Yang WJ, Zhao HP, Yu Y, Wang JH, Guo L, Liu JY et al (2023) Updates on global epidemiology, risk and prognostic factors of gastric cancer. World J Gastroenterol 29(16):2452–2468
Straatman J, van der Wielen N, Cuesta MA, de Lange-de Klerk ES, Jansma EP, van der Peet DL (2016) Minimally invasive versus open total gastrectomy for gastric cancer: a systematic review and meta-analysis of short-term outcomes and completeness of resection : surgical techniques in gastric cancer. World J Surg 40(1):148–157
de Jongh C, Triemstra L, van der Veen A, Brosens LAA, Luyer MDP, Stoot J et al (2022) Pattern of lymph node metastases in gastric cancer: a side-study of the multicenter LOGICA-trial. Gastric Cancer 25(6):1060–1072
Zhang H, Sang J, Liu F (2017) Recognition of specialization of minimally invasive treatment for gastric cancer in the era of precision medicine. Zhonghua Wei Chang Wai Ke Za Zhi 20(8):847–851
Jiao J, Liu S, Chen C, Maimaiti A, He Q, Hu S et al (2020) Comparative study of laparoscopic radical gastrectomy and open radical gastrectomy. J Minim Access Surg 16(1):41–46
van der Wielen N, Daams F, Rosati R, Parise P, Weitz J, Reissfelder C et al (2022) Health related quality of life following open versus minimally invasive total gastrectomy for cancer: results from a randomized clinical trial. Eur J Surg Oncol 48(3):553–560
Park S-H, Kim J-M, Park S-S (2021) Current status and trends of minimally invasive gastrectomy in Korea. Medicina 57(11):1195
Ribeiro U Jr, Dias AR, Ramos M, Yagi OK, Oliveira RJ, Pereira MA et al (2022) Short-term surgical outcomes of robotic gastrectomy compared to open gastrectomy for patients with gastric cancer: a randomized trial. J Gastrointest Surg 26(12):2477–2485
Tsekrekos A, Vossen LE, Lundell L, Jeremiasen M, Johnsson E, Hedberg J et al (2023) Improved survival after laparoscopic compared to open gastrectomy for advanced gastric cancer: a Swedish population-based cohort study. Gastric Cancer 26(3):467–477
Kitano S, Iso Y, Moriyama M, Sugimachi K (1994) Laparoscopy-assisted Billroth I gastrectomy. Surg Laparosc Endosc 4(2):146–148
Kitano S, Iso Y, Moriyama M, Sugimachi K (1994) Laparoscopy-assisted Billroth I gastrectomy. Surg Laparosc Endosc Percutan Tech 4(2):146–148
Beyer K, Baukloh AK, Kamphues C, Seeliger H, Heidecke CD, Kreis ME et al (2019) Laparoscopic versus open gastrectomy for locally advanced gastric cancer: a systematic review and meta-analysis of randomized controlled studies. World J Surg Oncol 17(1):68
Shi Y, Xu X, Zhao Y, Qian F, Tang B, Hao Y et al (2019) Long-term oncologic outcomes of a randomized controlled trial comparing laparoscopic versus open gastrectomy with D2 lymph node dissection for advanced gastric cancer. Surgery 165(6):1211–1216
Shi Y, Xu X, Zhao Y, Qian F, Tang B, Hao Y et al (2018) Short-term surgical outcomes of a randomized controlled trial comparing laparoscopic versus open gastrectomy with D2 lymph node dissection for advanced gastric cancer. Surg Endosc 32(5):2427–2433
van der Veen A, Brenkman HJF, Seesing MFJ, Haverkamp L, Luyer MDP, Nieuwenhuijzen GAP et al (2021) Laparoscopic versus open gastrectomy for gastric cancer (LOGICA): a multicenter randomized clinical trial. J Clin Oncol 39(9):978–989
van der Wielen N, Daams F, Rosati R, Parise P, Weitz J, Reissfelder C et al (2023) Three-year survival and distribution of lymph node metastases in gastric cancer following neoadjuvant chemotherapy: results from a European randomized clinical trial. Surg Endosc 37(9):7317–7324
Kim W, Kim HH, Han SU, Kim MC, Hyung WJ, Ryu SW et al (2016) Decreased morbidity of laparoscopic distal gastrectomy compared with open distal gastrectomy for stage I gastric cancer: short-term outcomes from a multicenter randomized controlled trial (KLASS-01). Ann Surg 263(1):28–35
van der Wielen N, Straatman J, Daams F, Rosati R, Parise P, Weitz J et al (2021) Open versus minimally invasive total gastrectomy after neoadjuvant chemotherapy: results of a European randomized trial. Gastric Cancer 24(1):258–271
Nuytens F, Dabakuyo-Yonli TS, Meunier B, Gagnière J, Collet D, D’Journo XB et al (2021) Five-year survival outcomes of hybrid minimally invasive esophagectomy in esophageal cancer: results of the MIRO randomized clinical trial. JAMA Surg 156(4):323–332
Hyung WJ, Yang HK, Park YK, Lee HJ, An JY, Kim W et al (2020) Long-term outcomes of laparoscopic distal gastrectomy for locally advanced gastric cancer: The KLASS-02-RCT randomized clinical trial. J Clin Oncol 38(28):3304–3313
Chan KS, Oo AM (2023) Learning curve of laparoscopic and robotic total gastrectomy: a systematic review and meta-analysis. Surg Today. https://doi.org/10.1007/s00595-023-02672-2
Seika P, Biebl M, Raakow J, Kröll D, Çetinkaya-Hosgör C, Thuss-Patience P et al (2022) The learning curve for hand-assisted laparoscopic total gastrectomy in gastric cancer patients. J Clin Med 11(22):6841
de Steur WO, Hartgrink HH, Dikken JL, Putter H, van de Velde CJ (2015) Quality control of lymph node dissection in the Dutch Gastric Cancer Trial. Br J Surg 102(11):1388–1393
Han SU, Hur H, Lee HJ, Cho GS, Kim MC, Park YK et al (2021) Surgeon quality control and standardization of D2 lymphadenectomy for gastric cancer: a prospective multicenter observational study (KLASS-02-QC). Ann Surg 273(2):315–324
Palter VN, MacRae HM, Grantcharov TP (2011) Development of an objective evaluation tool to assess technical skill in laparoscopic colorectal surgery: a Delphi methodology. Am J Surg 201(2):251–259
Brouwers MC, Kerkvliet K, Spithoff K (2016) The AGREE Reporting Checklist: a tool to improve reporting of clinical practice guidelines. BMJ 352:i1152
Williams PL, Webb C (1994) The Delphi technique: a methodological discussion. J Adv Nurs 19(1):180–186
Fink A, Kosecoff J, Chassin M, Brook RH (1984) Consensus methods: characteristics and guidelines for use. Am J Public Health 74(9):979–983
Graham B, Regehr G, Wright JG (2003) Delphi as a method to establish consensus for diagnostic criteria. J Clin Epidemiol 56(12):1150–1156
Lazarus JV, Romero D, Kopka CJ, Karim SA, Abu-Raddad LJ, Almeida G et al (2022) A multinational Delphi consensus to end the COVID-19 public health threat. Nature 611(7935):332–345
Vogel C, Zwolinsky S, Griffiths C, Hobbs M, Henderson E, Wilkins E (2019) A Delphi study to build consensus on the definition and use of big data in obesity research. Int J Obes (Lond) 43(12):2573–2586
Lam K, Abràmoff MD, Balibrea JM, Bishop SM, Brady RR, Callcut RA et al (2022) A Delphi consensus statement for digital surgery. NPJ Digit Med 5(1):100
Khamis NN, Satava RM, Alnassar SA, Kern DE (2016) A stepwise model for simulation-based curriculum development for clinical skills, a modification of the six-step approach. Surg Endosc 30(1):279–287
Nakata K, Nagai E, Ohuchida K, Shimizu S, Tanaka M (2015) Technical feasibility of laparoscopic total gastrectomy with splenectomy for gastric cancer: clinical short-term and long-term outcomes. Surg Endosc 29(7):1817–1822
Haverkamp L, Brenkman HJ, Ruurda JP, Ten Kate FJ, van Hillegersberg R (2016) The oncological value of omentectomy in gastrectomy for cancer. J Gastrointest Surg 20(5):885–890
Metwally IH, Abdelkhalek M, Shetiwy M, Elalfy AF, Abouzid A, Elbalka SS et al (2020) Significance of omental infiltration in gastric cancer patients: a retrospective cohort study. J Gastrointest Cancer 51(3):861–867
Kong M, Chen H, Zhang R, Sheng H, Li L (2022) Overall survival advantage of omentum preservation over omentectomy for advanced gastric cancer: a systematic review and meta-analysis. World J Surg 46(8):1952–1961
Kim TH, Kim IH, Kang SJ, Choi M, Kim BH, Eom BW et al (2023) Korean practice guidelines for gastric cancer 2022: an evidence-based, multidisciplinary approach. J Gastric Cancer 23(1):3–106
Renna MS, Grzeda MT, Bailey J, Hainsworth A, Ourselin S, Ebner M et al (2023) Intraoperative bowel perfusion assessment methods and their effects on anastomotic leak rates: meta-analysis. Br J Surg 110(9):1131–1142
Nickel F, Studier-Fischer A, Hausmann D, Klotz R, Vogel-Adigozalov SL, Tenckhoff S et al (2022) Minimally invasivE versus open total GAstrectomy (MEGA): study protocol for a multicentre randomised controlled trial (DRKS00025765). BMJ Open 12(10):e064286
Acknowledgements
We want to thank the EAES Research Sandpit Panel members, Prof. George Hanna, Prof. Tan Arulampalam, Prof. Sheraz Markar, Suzanne S Gisbertz, and Christos Kontovounisios for choosing and supporting our project.
Funding
Open Access funding enabled and organized by Projekt DEAL. Funded by the European Association of Endoscopic Surgeons EAES Research Sandpit Grant 2022.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Hans F Fuchs has the following conflicts of interest to disclose: Medtronic: Advisory Board; Stryker: Advisory Board; Intuitive Surgical: Educational Grant (ESOMAP trial); Teaching Courses (EAES). Amila Cizmic, Ivan Romic, Andrea Balla, Nicolò Barabino, Gabriele Anania, Gian Luca Baiocchi, Branko Bakula, Carmen Balagué, Felix Berlth, Vasile Bintintan, Umberto Bracale, Jan-Hendrik Egberts, Suzanne S Gisbertz, Ines Gockel, Peter Grimminger, Richard van Hillegersberg, Noriyuki Inaki, Arul Immanuel, Daniel Korr, Philipp Lingohr, Pietro Mascagni, Nathaniel Melling, Marco Milone, Yoav Mintz, Salvador Morales-Conde, Yusef Moulla, Beat P Müller-Stich, Kiyokazu Nakajima, Magnus Nilsson, Matthias Reeh, Pierpaolo Sileri, Eduardo M Targarona, Yuki Ushimaru, Young-Woo Kim, Sheraz Markar, Felix Nickel, Anuja T Mitra have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cizmic, A., Romic, I., Balla, A. et al. An international Delphi consensus for surgical quality assessment of lymphadenectomy and anastomosis in minimally invasive total gastrectomy for gastric cancer. Surg Endosc 38, 488–498 (2024). https://doi.org/10.1007/s00464-023-10614-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10614-9