Abstract
Background
Primary hepatocellular carcinoma (HCC) and colorectal liver metastases (CRLM) represent the liver’s two most common malignant neoplasms. Liver-directed therapies such as ablation have become part of multidisciplinary therapies despite a paucity of data. Therefore, an expert panel was convened to develop evidence-based recommendations regarding the use of microwave ablation (MWA) and radiofrequency ablation (RFA) for HCC or CRLM less than 5 cm in diameter in patients ineligible for other therapies.
Methods
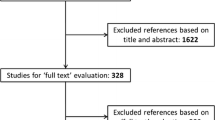
A systematic review was conducted for six key questions (KQ) regarding MWA or RFA for solitary liver tumors in patients deemed poor candidates for first-line therapy. Subject experts used the GRADE methodology to formulate evidence-based recommendations and future research recommendations.
Results
The panel addressed six KQs pertaining to MWA vs. RFA outcomes and laparoscopic vs. percutaneous MWA. The available evidence was poor quality and individual studies included both HCC and CRLM. Therefore, the six KQs were condensed into two, recognizing that these were two disparate tumor groups and this grouping was somewhat arbitrary. With this significant limitation, the panel suggested that in appropriately selected patients, either MWA or RFA can be safe and feasible. However, this recommendation must be implemented cautiously when simultaneously considering patients with two disparate tumor biologies. The limited data suggested that laparoscopic MWA of anatomically more difficult tumors has a compensatory higher morbidity profile compared to percutaneous MWA, while achieving similar overall 1-year survival. Thus, either approach can be appropriate depending on patient-specific factors (very low certainty of evidence).
Conclusion
Given the weak evidence, these guidelines provide modest guidance regarding liver ablative therapies for HCC and CRLM. Liver ablation is just one component of a multimodal approach and its use is currently limited to a highly selected population. The quality of the existing data is very low and therefore limits the strength of the guidelines.
Executive summary
The multidisciplinary management of both primary hepatocellular carcinoma (HCC) and colorectal liver metastases (CRLM) may include liver-directed therapies as part of treatment algorithms; these algorithms focus heavily on control of liver-specific disease as in many cases this serves as a proxy for long-term survival. Hepatectomy is the primary treatment option in patients who can tolerate resection for both HCC and CRLM. Liver-directed therapies include arterial embolization, stereotactic body radiation therapy, and liver ablation. Over the last several decades, microwave ablation (MWA) and radiofrequency ablation (RFA) of liver tumors have been used in high-risk patients unfit for surgical intervention or tumors not amenable to local control with other therapies. As ablation is an evolving technology, outcomes data are primarily reported in liver tumors less than 3 cm in diameter, while data for liver tumors greater than 3 cm are limited for both HCC and CRLM. The authors sought to perform a systematic review of the existing data to assess for meaningful conclusions. Therefore, a multidisciplinary expert panel was convened to develop evidence-based recommendations to support clinicians, patients, and others regarding the role of liver ablation in the treatment of HCC and CRLM up to 5 cm in diameter.
AbstractSection MethodsA systematic review was conducted for six key questions (KQ) regarding the use of either MWA or RFA for solitary HCC or CRLM. Due to the paucity of evidence available, HCC and CRLM less than 5 cm in diameter were combined into two final KQs which were used to develop recommendations. Evidence-based recommendations were formulated using the GRADE methodology by subject matter experts. Additionally, the panel developed recommendations for future research.
AbstractSection Interpretation of strong and conditional recommendationsAll guideline recommendations were assigned “conditional” recommendations. These were based on the GRADE approach. The words “the guideline panel suggests” were used for conditional recommendations.
AbstractSection Key questions addressed by these guidelines-
1.
Should MWA (laparoscopic or open) vs. RFA (laparoscopic or open) be used for HCC or CRLM less than 5 cm ineligible for other therapies?
-
2.
Should laparoscopic MWA vs. percutaneous MWA be used for HCC and/or CRLM less than 5 cm ineligible for other therapies?
-
1.
Should MWA (laparoscopic or open) vs. RFA (laparoscopic or open) be used for HCC or CRLM less than 5 cm ineligible for other therapies?
The panel suggests MWA and RFA are both safe and feasible. There was insufficient evidence to recommend one modality over another in terms of oncologic outcomes (conditional recommendation, very low certainty of evidence).
-
2.
Should laparoscopic MWA vs. percutaneous MWA be used for HCC and/or CRLM less than 5 cm ineligible for other therapies?
The panel suggests that either ablative approach achieves similar overall outcomes, albeit through distinct patterns. The laparoscopic approach obtained better local control and the percutaneous approach had fewer morbidities while obtaining similar overall 1-year survival (conditional recommendation, very low certainty of evidence).
The aim of these guidelines is to assist surgeons and physicians in making management decisions for patients with HCC or CRLM. Given that the evidence for this guideline was based on very low certainty evidence, these guidelines should be applied with caution. They are also intended to provide education, inform advocacy, and describe future areas for research. The guidelines are not meant to mandate a particular approach or strategy given the lack of evidence and intricacies of the healthcare environment, individual patient needs, comorbidities, and surgeon experience. Specific situations require adjustment of treatment plans to suit the needs and priorities of the individual patient. Finally, since the guidelines take a patient-centered approach, patients can use these guidelines as a source of information and for discussion with their physicians.
Similar content being viewed by others
References
Ferlay J, Parkin DM, Curado MP et al (2014) Cancer incidence in five continents, volumes I to X: IARC CANCERBase No. 10. http://ci5.iarc.fr. Accessed 25 Nov 2014
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A (2015) Global cancer statistics, 2012. CA Cancer J Clin 65:87–108
Rich NE, Yopp AC, Singal AG, Murphy CC (2020) Hepatocellular carcinoma incidence is decreasing among younger adults in the United States. Clin Gastroenterol Hepatol 18(242–248):e245
Martin J, Petrillo A, Smyth EC, Shaida N, Khwaja S, Cheow H, Duckworth A, Heister P, Praseedom R, Jah A (2020) Colorectal liver metastases: Current management and future perspectives. World J Clin Oncol 11:761–808
Siegel RL, Miller KD, Goding Sauer A, Fedewa SA, Butterly LF, Anderson JC, Cercek A, Smith RA, Jemal A (2020) Colorectal cancer statistics. CA Cancer J Clin 70:145–164
Bhardwaj N, Strickland A, Ahmad F, Dennison A, Lloyd D (2010) Liver ablation techniques: a review. Surg Endosc 24:254–265
Benson AB 3rd, Abrams TA, Ben-Josef E, Bloomston PM, Botha JF, Clary BM, Covey A, Curley SA, D’Angelica MI, Davila R, Ensminger WD, Gibbs JF, Laheru D, Malafa MP, Marrero J, Meranze SG, Mulvihill SJ, Park JO, Posey JA, Sachdev J, Salem R, Sigurdson ER, Sofocleous C, Vauthey JN, Venook AP, Goff LW, Yen Y, Zhu AX (2009) NCCN clinical practice guidelines in oncology: hepatobiliary cancers. Natl Compr Canc Netw 7:350–391
Decadt B, Siriwardena AK (2004) Radiofrequency ablation of liver tumours: systematic review. Lancet Oncol 5:550–560
McGhana JP, Dodd GD III (2001) Radiofrequency ablation of the liver: current status. Am J Roentgenol 176:3–16
Abdalla M, Collings AT, Dirks R, Onkendi E, Nelson D, Ozair A, Miraflor E, Rahman F, Whiteside J, Shah MM, Ayloo S, Abou-Setta A, Sucandy I, Kchaou A, Douglas S, Polanco P, Vreeland T, Buell J, Ansari MT, Pryor AD, Slater BJ, Awad Z, Richardson W, Alseidi A, Jeyarajah DR, Ceppa EP (2022) Surgical approach to microwave and radiofrequency liver ablation for hepatocellular carcinoma and colorectal liver metastases less than 5 cm: a systematic review and meta-analysis. Surg Endosc 37(5):3340–3353. https://doi.org/10.1007/s00464-022-09815-5
Alonso-Coello P, Oxman AD, Moberg J, Brignardello-Petersen R, Akl EA, Davoli M, Treweek S, Mustafa RA, Vandvik PO, Meerpohl J, Guyatt GH, Schünemann HJ (2016) GRADE evidence to decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 2: clinical practice guidelines. BMJ 353:12089
Alonso-Coello P, Schunemann HJ, Moberg J, Brignardello-Petersen R, Akl EA, Davoli M, Treweek S, Mustafa RA, Rada G, Rosenbaum S, Morelli A, Guyatt GH, Oxman AD, GRADE Working Group (2016) GRADE evidence to decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 1: introduction. BMJ 353:12016
Andrews JC, Schunemann HJ, Oxman AD, Pottie K, Meerpohl JJ, Coello PA, Rind D, Montori VM, Brito JP, Norris S, Elbarbary M, Post P, Nasser M, Shukla V, Jaeschke R, Brozek J, Djulbegovic B, Guyatt G (2013) GRADE guidelines: 15 going from evidence to recommendation-determinants of a recommendation’s direction and strength. J Clin Epidemiol 66(7):726–735
Chen Y, Yang K, Marusic A, Qaseem A, Meerpohl JJ, Flottorp S, Akl EA, Schünemann HJ, Chan ES, Falck-Ytter Y, Ahmed F, Barber S, Chen C, Zhang M, Xu B, Tian J, Song F, Shang H, Tang K, Wang Q, Norris SL, RIGHT (Reporting Items for Practice Guidelines in Healthcare) Working Group (2017) A reporting tool for practice guidelines in health care: the RIGHT statement. Ann Intern Med 166:128–132
Rogers AT, Dirks R, Burt HA, Haggerty S, Kohn GP, Slater BJ, Walsh D, Stefanidis D, Pryor A (2021) Society of American gastrointestinal and endoscopic SURGEONS (SAGES) guidelines development: standard operating procedure. Surg Endosc 35:2417–2427
Schünemann HJ, Brożek J, Guyatt G, Oxman AD (eds) (2013) GRADE handbook: handbook for grading quality of evidence and strength of recommendations. https://guidelinedevelopment.org/handbook. Accessed Oct 2013
An C, Li WZ, Huang ZM, Yu XL, Han YZ, Liu FY, Wu SS, Yu J, Liang P, Huang J (2021) Small single perivascular hepatocellular carcinoma: comparisons of radiofrequency ablation and microwave ablation by using propensity score analysis. Eur Radiol 31:4764–4773
Correa-Gallego C, Fong Y, Gonen M, D’Angelica MI, Allen PJ, DeMatteo RP, Jarnagin WR, Kingham TP (2014) A retrospective comparison of microwave ablation vs. radiofrequency ablation for colorectal cancer hepatic metastases. Ann Surg Oncol 21:4278–4283
Iida H, Aihara T, Ikuta S, Yamanaka N (2013) A comparative study of therapeutic effect between laparoscopic microwave coagulation and laparoscopic radiofrequency ablation. Hepatogastroenterology 60:662–665
Lee KF, Wong J, Hui JW, Cheung YS, Chong CC, Fong AK, Yu SC, Lai PB (2017) Long-Term outcomes of microwave versus radiofrequency ablation for hepatocellular carcinoma by surgical approach: a retrospective comparative study. Asian J Surg 40:301–308
Santambrogio R, Chiang J, Barabino M, Meloni FM, Bertolini E, Melchiorre F, Opocher E (2017) Comparison of laparoscopic microwave to radiofrequency ablation of small hepatocellular carcinoma (≤3 cm). Ann Surg Oncol 24:257–263
Simo KA, Sereika SE, Newton KN, Gerber DA (2011) Laparoscopic-assisted microwave ablation for hepatocellular carcinoma: safety and efficacy in comparison with radiofrequency ablation: lap-MWA for HCC: safety and efficacy. J Surg Oncol 104:822–829
Takahashi H, Kahramangil B, Kose E, Berber E (2018) A comparison of microwave thermosphere versus radiofrequency thermal ablation in the treatment of colorectal liver metastases. HPB 20:1157–1162
Yang B, Yuwei L (2017) A comparative study of laparoscopic microwave ablation with laparoscopic radiofrequency ablation for colorectal liver metastasis. J BUON 22:667–672
Sakaguchi H, Seki S, Tsuji K, Teramoto K, Suzuki M, Kioka K, Isoda N, Ido K (2009) Endoscopic thermal ablation therapies for hepatocellular carcinoma: a multi-center study. Hepatol Res 39:47–52. https://doi.org/10.1111/j.1872-034X.2008.00410.x
De Cobelli F, Marra P, Ratti F, Ambrosi A, Colombo M, Damascelli A, Sallemi C, Gusmini S, Salvioni M, Diana P, Cipriani F, Venturini M, Aldrighetti L, Del Maschio A (2017) Microwave ablation of liver malignancies: comparison of effects and early outcomes of percutaneous and intraoperative approaches with different liver conditions: new advances in interventional oncology: state of the art. Med Oncol 34:49
Della Corte A, Ratti F, Monfardini L, Marra P, Gusmini S, Salvioni M, Venturini M, Cipriani F, Aldrighetti L, De Cobelli F (2020) Comparison between percutaneous and laparoscopic microwave ablation of hepatocellular carcinoma. Int J Hyperthermia 37:542–548
Acknowledgements
We would like to thank Sarah Colón, the SAGES senior program coordinator, Holly Ann Burt, the SAGES librarian, and the SAGES guidelines committee members for their help with the creation of this guideline.
Disclaimer
Clinical practice guidelines are intended to indicate the best available approach to medical conditions as established by a systematic review of available data and expert opinion. The approach suggested may not necessarily be the only acceptable approach given the complexity of the healthcare environment. These guidelines are intended to accommodate the numerous variables inherent to the treatment of an individual patient. Treatment strategy must be tailored to the patient on case-by-case basis. These guidelines are applicable to all physicians who are appropriately credentialed regardless of specialty at institutions with appropriate expertise in both laparoscopic and percutaneous approaches.
These guidelines are developed under the auspices of SAGES and AHPBA, the guidelines committee, and approved by the Board of Governors of both societies. The recommendations of each guideline undergo multidisciplinary review and are considered valid at the time of production based on the data available. New developments in medical research and practice pertinent to each guideline are reviewed, and guidelines are periodically updated.
Funding
This work was funded by Society of American Gastrointestinal and Endoscopic Surgeons.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
The following authors disclosed ties: Edwin Onkendi is an investor in ROMtech Modern Technology for Rehabilitation. Mihir M. Shah has received consulting fees from Intuitive. Rebecca Dirks owns publicly traded stock from Johnson & Johnson. Patricio M. Polanco has received the Eugene Frenkel Scholar Award from the Simmons Cancer Center at UT Southwestern Medical Center and consulting fees from Pallisade Bio Inc. He is a participant on a data safety monitoring or advisory board at the Simmons Cancer Center. Timothy J. Vreeland has received consulting fees from Lumabridge. Choon Hyuck Kwon has received consulting fees from Medtronic and Fujifilm, payment or honoraria from Medtronic and Fujifilm, and travel support from Fujifilm. Aurora Pryor has received payment or honoraria from Stryker, Gore, and Medtronic and payment for expert testimony. She holds leadership roles with SAGES, the Fellowship Council, and SAGES Ingenuity. Bethany J. Slater has received consulting fees from Hologic and Cook Medical and holds leadership role with SAGES. Rohan Jeyarajah has received consulting fees from Sirtex, AngioDynamics, and Ethicon, payment or honoraria from Sirtex, and travel support from Methodist Health System. He is a participant on a data safety monitoring or advisory board at AngioDynamics and holds leadership roles with AHPBA and ABS. Eugene P. Ceppa, Amelia Collings, Moustafa Abdalla, Daniel W. Nelson, Ahmad Ozair, Emily Miraflor, Faique Rahman, Jake Whiteside, Subhashini Ayloo, Sunjay S. Kumar, Mohammed T. Ansari, Iswanto Sucandy, Kchaou Ali, Sam Douglas, Joseph Buell, Ahmed M. Abou-Setta, Ziad Awad, John B. Martinie, Fabio Sbrana, William Richardson, and Adnan Alseidi have no financial ties or conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ceppa, E.P., Collings, A.T., Abdalla, M. et al. SAGES/AHPBA guidelines for the use of microwave and radiofrequency liver ablation for the surgical treatment of hepatocellular carcinoma or colorectal liver metastases less than 5 cm. Surg Endosc 37, 8991–9000 (2023). https://doi.org/10.1007/s00464-023-10468-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10468-1