Abstract
Introduction
In patients with history of cancer adrenal metastases can be found in up to 70% of adrenal tumors detected during follow-up. Currently, laparoscopic adrenalectomy (LA) is considered the gold standard approach for benign adrenal tumors but is still controversial in malignant disease. Depending on the patient’s oncological status, adrenalectomy might be a possible treatment option. Our objective was to analyze the results of LA for adrenal metastasis from solid tumors in two referral centers.
Methods
Retrospective analysis of 17 patients with non-primary adrenal malignancy treated with LA between 2007 and 2019 was performed. Demographic and primary tumor data, type of metastasis, morbidity, disease recurrence and evolution were evaluated. Patients were compared according to type of metastases: synchronous (< 6 months) vs metachronous (≥ 6 months).
Results
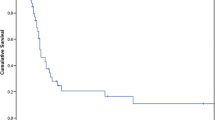
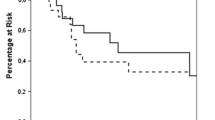
17 patients were included. Median metastatic adrenal tumor size was 4 cm (IQR, 3–5.4). We had one conversion to open surgery. Recurrence was found in 6 patients with one recurring in the adrenal bed. The median OS was 24 (IQR, 10.5–60.5) months and 5-year OS was 61.4% (95%CI: 36.7%–81.4%). Patients with metachronous metastases had better overall survival vs. patients with synchronous metastases (87% vs. 14%, p = 0.0037).
Conclusion
LA for adrenal metastases is a procedure associated with low morbidity and acceptable oncologic outcomes. Based on our results, seems reasonable to offer this procedure to carefully selected patients, mainly those with metachronous presentation. Indication of LA must be done on a case by case evaluation in the context of a multidisciplinary tumor board.
Graphical Abstract



Similar content being viewed by others
Abbreviations
- LA:
-
Laparoscopic adrenalectomy
- LOS:
-
Length of stay
- DFS:
-
Disease-free survival
- OS:
-
Overall survival
- NSCLC:
-
Non-small cell lung cancer
References
Romero Arenas MA, Sui D, Grubbs EG, Lee JE, Perrier ND (2014) Adrenal metastectomy is safe in selected patients. World J Surg 38(6):1336–1342. https://doi.org/10.1007/s00268-014-2454-x
Moreno P, de la Quintana BA, Musholt TJ et al (2013) Adrenalectomy for solid tumor metastases: results of a multicenter European study. Surgery 154(6):1215–1223. https://doi.org/10.1016/j.surg.2013.06.021
Lenert JT, Barnett CC Jr, Kudelka AP et al (2001) Evaluation and surgical resection of adrenal masses in patients with a history of extra-adrenal malignancy. Surgery 130(6):1060–1067. https://doi.org/10.1067/msy.2001.118369
Adler JT, Mack E, Chen H (2007) Isolated adrenal mass in patients with a history of cancer: remember pheochromocytoma. Ann Surg Oncol 14(8):2358–2362. https://doi.org/10.1245/s10434-007-9426-4
Creamer J, Matthews BD (2013) Laparoscopic adrenalectomy for cancer. Surg Oncol Clin N Am 22(1):111–124. https://doi.org/10.1016/j.soc.2012.08.006. (PMID: 23158088)
Bradley CT, Strong VE (2014) Surgical management of adrenal metastases. J Surg Oncol 109(1):31–35. https://doi.org/10.1002/jso.23461
Russo AE, Untch BR, Kris MG et al (2019) Adrenal metastasectomy in the presence and absence of extraadrenal metastatic disease. Ann Surg 270(2):373–377. https://doi.org/10.1097/SLA.0000000000002749
Drake FT, Beninato T, Xiong MX, Shah NV, Kluijfhout WP, Feeney T, Suh I, Gosnell JE, Shen WT, Duh QY (2019) Laparoscopic adrenalectomy for metastatic disease: Retrospective cohort with long-term, comprehensive follow-up. Surgery 165(5):958–964. https://doi.org/10.1016/j.surg.2018.11.008. (Epub 2018 Dec 24 PMID: 30591377)
Gagner M, Lacroix A, Bolte E (1992) Laparoscopic adrenalectomy in Cushing’s syndrome and pheochromocytoma. N Engl J Med 327(14):1033
Maurice MJ, Bream MJ, Kim SP, Abouassaly R (2017) Surgical quality of minimally invasive adrenalectomy for adrenocortical carcinoma: a contemporary analysis using the National Cancer Database. BJU Int 119(3):436–443. https://doi.org/10.1111/bju.13618. (Epub 2016 Sep 1 PMID: 27488744)
Jossart GH, Burpee SE, Gagner M (2000) Surgery of the adrenal glands. Endocrinol Metab Clin North Am 29(1):57–68
Zeiger MA, Thompson GB, Duh QY et al (2009) American association of clinical endocrinologists and american association of endocrine surgeons medical guidelines for the management of adrenal incidentalomas: executive summary of recommendations. Endocr Pract 15(5):450–453. https://doi.org/10.4158/EP.15.5.450. (PMID: 19632968)
NIH state-of-the-science statement on management of the clinically inapparent adrenal mass (“incidentaloma”). NIH Consens State Sci Statements 2002, 19(2): 1–25.
Calcatera NA, Hsiung-Wang C, Suss NR, Winchester DJ, Moo-Young TA, Prinz RA (2018) Minimally invasive adrenalectomy for adrenocortical carcinoma: five-year trends and predictors of conversion. World J Surg 42(2):473–481. https://doi.org/10.1007/s00268-017-4290-2. (PMID: 29022106)
Stefanidis D, Goldfarb M, Kercher KW et al (2013) SAGES guidelines for minimally invasive treatment of adrenal pathology. Surg Endosc 27(11):3960–3980
Fassnacht M, Arlt W, Bancos I et al (2016) Management of adrenal incidentalomas: European society of endocrinology clinical practice guideline in collaboration with the European Network for the study of adrenal tumors. Eur J Endocrinol 175(2):G1-34
Strong VE, D’Angelica M, Tang L et al (2007) Laparoscopic adrenalectomy for isolated adrenal metastasis. Ann Surg Oncol 14(12):3392–3400. https://doi.org/10.1245/s10434-007-9520-7
Sancho JJ, Triponez F, Montet X, Sitges-Serra A (2012) Surgical management of adrenal metastases. Langenbecks Arch Surg 397(2):179–194. https://doi.org/10.1007/s00423-011-0889-1. (Epub 2011 Dec 16 PMID: 22205385)
Howell GM, Carty SE, Armstrong MJ, Stang MT, McCoy KL, Bartlett DL, Yip L (2013) Outcome and prognostic factors after adrenalectomy for patients with distant adrenal metastasis. Ann Surg Oncol 20(11):3491–3496. https://doi.org/10.1245/s10434-013-3050-2. (Epub 2013 Jun 21 PMID: 23793361; PMCID: PMC4879835)
Kim SH, Brennan MF, Russo P, Burt ME, Coit DG (1998) The role of surgery in the treatment of clinically isolated adrenal metastasis. Cancer 82(2):389–394 (PMID: 9445197)
Sarela AI, Murphy I, Coit DG, Conlon KC (2003) Metastasis to the adrenal gland: the emerging role of laparoscopic surgery. Ann Surg Oncol 10(10):1191–1196. https://doi.org/10.1245/aso.2003.04.020. (PMID: 14654476)
Vazquez BJ, Richards ML, Lohse CM, Thompson GB, Farley DR, Grant CS, Huebner M, Moreno J (2012) Adrenalectomy improves outcomes of selected patients with metastatic carcinoma. World J Surg 36(6):1400–1405. https://doi.org/10.1007/s00268-012-1506-3. (PMID: 22411083)
Goldstraw P, Chansky K, Crowley J, Rami-Porta R, Asamura H, Eberhardt WE, Nicholson AG, Groome P, Mitchell A, Bolejack V (2016) International association for the study of lung cancer staging and prognostic factors committee, advisory boards, and participating institutions. The IASLC Lung cancer staging project: proposals for revision of the TNM stage groupings in the forthcoming (Eight) edition of the TNM classification for lung cancer. J Thorac Oncol 11(1):39–51
Ayabe H, Tsuji H, Hara S, Tagawa Y, Kawahara K, Tomita M (1995) Surgical management of adrenal metastasis from bronchogenic carcinoma. J Surg Oncol 58(3):149–154. https://doi.org/10.1002/jso.2930580303. (PMID: 7898109)
Muth A, Persson F, Jansson S, Johanson V, Ahlman H, Wängberg B (2010) Prognostic factors for survival after surgery for adrenal metastasis. Eur J Surg Oncol 36:699–704
Luketich JD, Burt ME (1996) Does resection of adrenal metastases from non-small cell lung cancer improve survival? Ann Thorac Surg 62:1614–1616
Author information
Authors and Affiliations
Contributions
Study concept and design: SDQ, WSN. Acquisition of data: WSN, FI, JC. Drafting of the manuscript: SDQ, WSN. Critical revision of the manuscript for important intellectual content: SDQ, IC, WSN. Final revision and final approval for publication: SDQ. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Disclosures
Drs Sergio D Quildrian, Walter S Nardi, Facundo Iriarte, Maricel Recalde, Inés Califano and Jorge Chapela have no conflicts of interest or financial ties to disclose. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
The ethical approval was carried out by the local Ethics Committee of the British Hospital of Buenos Aires.
Consent to participate
Due to the retrospective nature of this study, the Ethics Committee waived the requirement for written informed consent. However, all patients signed the surgical consent form.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Quildrian, S.D., Nardi, W.S., Iriarte, F. et al. Laparoscopic adrenalectomy for adrenal metastases of solid tumors. Surg Endosc 37, 4651–4657 (2023). https://doi.org/10.1007/s00464-023-09961-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-09961-4