Abstract
Background
Robotic-assisted Kasai portoenterostomy (RAKPE) has been utilized to treat biliary atresia (BA). However, RAKPE is not widely performed and its efficacy remains unknown. We summarized the experience of RAKPE for BA and determined its efficacy.
Materials and methods
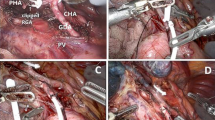
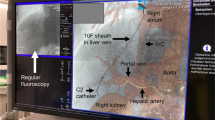
We retrospectively analyzed 25 consecutive infants with non-syndromic type III BA who received RAKPE in our center from January 2020 to July 2021. RAKPE is a three-arm setup and four-trocar operation. Bipolar coagulation was used to dissect the small blood vessels at the hepatic portal. The fibrous cone was shallowly transected with bending electric scissors, followed by gelatin sponge compression to staunch the hemorrhage. Finally, a wide anastomosis was accurately constructed. Demographics and outcomes were recorded.
Results
The mean operative time was 211.64 ± 18.93 min. No conversion to laparotomy or intraoperative complications occurred. The mean estimated blood loss was 7.64 ± 2.43 mL. Enteral feeding was resumed after 3.44 ± 1.23 days. All patients achieved bile excretion postoperatively, and dark green bile-stained stools were passed 1.50 days (range 1.00–3.00 days) after surgery. The average postoperative length of hospital stay was 10.32 ± 2.59 days. The jaundice clearance (JC) rate was 76.00% within 6 months after surgery and the incidence of cholangitis was 48.00% within 1 year following surgery. The survival with native liver (SNL) rate was 80.00% at 1 year and 66.67% at 2 years.
Conclusion
RAKPE can be regarded as a treatment option for patients with BA due to the good outcomes reported. However, long-term studies comparing open or laparoscopic approaches are needed.






Similar content being viewed by others
References
Kasai M (1959) A new operation for “noncorrectable” biliary atresia: hepatic portoenterostomy. Shujutsu 13:733–739
Esteves E, Clemente NE, Ottaiano NM, Devanir J Jr, Esteves Pereira R (2002) Laparoscopic Kasai portoenterostomy for biliary atresia. Pediatr Surg Int. https://doi.org/10.1007/s00383-002-0791-6
Lishuang M, Zhen C, Guoliang Q, Zhen Z, Chen W, Long L, Shuli L (2015) Laparoscopic portoenterostomy versus open portoenterostomy for the treatment of biliary atresia: a systematic review and meta-analysis of comparative studies. Pediatr Surg Int. https://doi.org/10.1007/s00383-015-3662-7
Li Y, Gan J, Wang C, Xu Z, Zhao Y, Ji Y (2019) Comparison of laparoscopic portoenterostomy and open portoenterostomy for the treatment of biliary atresia. Surg Endosc. https://doi.org/10.1007/s00464-019-06905-9
Hinojosa-Gonzalez DE, Bueno LC, Roblesgil-Medrano A, Salgado-Garza G, Hurtado-Arellano S, Farias JS, Torres-Martinez M, Escarcega-Bordagaray JA, Salan-Gomez M, Flores-Villalba E (2021) Laparoscopic vs open portoenterostomy in biliary atresia: a systematic review and meta-analysis. Pediatr Surg Int. https://doi.org/10.1007/s00383-021-04964-5
Ji Y, Yang K, Zhang X, Jin S, Jiang X, Chen S, Xu Z (2021) The short-term outcome of modified laparoscopic Kasai portoenterostomy for biliary atresia. Surg Endosc. https://doi.org/10.1007/s00464-020-07530-7
Shirota C, Murase N, Tanaka Y, Ogura Y, Nakatochi M, Kamei H, Kurata N, Hinoki A, Tainaka T, Sumida W, Yokota K, Makita S, Oshima K, Uchida H (2020) Laparoscopic Kasai portoenterostomy is advantageous over open Kasai portoenterostomy in subsequent liver transplantation. Surg Endosc. https://doi.org/10.1007/s00464-019-07108-y
Murase N, Hinoki A, Shirota C, Tomita H, Shimojima N, Sasaki H, Nio M, Tahara K, Kanamori Y, Shinkai M, Yamamoto H, Sugawara Y, Hibi T, Ishimaru T, Kawashima H, Koga H, Yamataka A, Uchida H (2019) Multicenter, retrospective, comparative study of laparoscopic and open Kasai portoenterostomy in children with biliary atresia from Japanese high-volume centers. J Hepatobiliary Pancreat Sci. https://doi.org/10.1002/jhbp.594
Lorincz A, Langenburg S, Klein MD (2003) Robotics and the pediatric surgeon. Curr Opin Pediatr. https://doi.org/10.1097/00008480-200306000-00006
Dutta S, Woo R, Albanese CT (2007) Minimal access portoenterostomy: advantages and disadvantages of standard laparoscopic and robotic techniques. J Laparoendosc Adv Surg Tech A. https://doi.org/10.1089/lap.2006.0112
Meehan JJ, Elliott S, Sandler A (2007) The robotic approach to complex hepatobiliary anomalies in children: preliminary report. J Pediatr Surg. https://doi.org/10.1016/j.jpedsurg.2007.08.040
Kumar R, Lal BB, Sood V, Khanna R, Kumar S, Bharathy KGS, Alam S (2019) Predictors of successful Kasai portoenterostomy and survival with native liver at 2 years in infants with biliary atresia. J Clin Exp Hepatol. https://doi.org/10.1016/j.jceh.2018.09.008
Wildhaber BE, Majno P, Mayr J, Zachariou Z, Hohlfeld J, Schwoebel M, Kistler W, Meuli M, Le Coultre C, Mentha G, Belli D, Chardot C (2008) Biliary atresia: Swiss national study, 1994–2004. J Pediatr Gastroenterol Nutr. https://doi.org/10.1097/MPG.0b013e3181633562
Lee WS, Chai PF, Lim KS, Lim LH, Looi LM, Ramanujam TM (2009) Outcome of biliary atresia in Malaysia: a single-centre study. J Paediatr Child Health. https://doi.org/10.1111/j.1440-1754.2009.01490.x
Li YB, Rong LY, Tang JF, Niu HZ, Jin Z, Zhou Y, Cao GQ, Zhang X, Chi SQ, Tang ST (2022) Re-evaluation of laparoscopic hepatic subcapsular spider-like telangiectasis sign: a highly accurate method to diagnose biliary atresia in infants. Front Pediatr. https://doi.org/10.3389/fped.2022.850449
Zhou Y, Jiang M, Tang ST, Yang L, Zhang X, Yang DH, Xiong M, Li S, Cao GQ, Wang Y (2017) Laparoscopic finding of a hepatic subcapsular spider-like telangiectasis sign in biliary atresia. World J Gastroenterol. https://doi.org/10.3748/wjg.v23.i39.7119
Sun X, Diao M, Wu X, Cheng W, Ye M, Li L (2016) A prospective study comparing laparoscopic and conventional Kasai portoenterostomy in children with biliary atresia. J Pediatr Surg. https://doi.org/10.1016/j.jpedsurg.2015.10.045
Li Y, Xiang B, Wu Y, Wang C, Wang Q, Zhao Y, Chen S, Ji Y, Xu Z (2018) Medium-term outcome of laparoscopic Kasai portoenterostomy for biliary atresia with 49 cases. J Pediatr Gastroenterol Nutr. https://doi.org/10.1097/MPG.0000000000001934
Ji Y, Zhou J, Zhang X, Chen S, Xu Z (2021) Laparoscopic Kasai portoenterostomy for cystic biliary atresia: midterm follow-up results of 35 patients. Surg Today. https://doi.org/10.1007/s00595-021-02297-3
Shirota C, Hinoki A, Tainaka T, Sumida W, Kinoshita F, Yokota K, Makita S, Amano H, Nakagawa Y, Uchida H (2022) Laparoscopic Kasai portoenterostomy can be a standard surgical procedure for treatment of biliary atresia. World J Gastrointest Surg. https://doi.org/10.4240/wjgs.v14.i1.56
Abe E, Koga H, Nakamura H, Ochi T, Seo S, Lane GJ, Yamataka A (2022) Mid-term outcome of postoperative biliary atresia patients according to level of transection of the biliary remnant and depth of suturing. Pediatr Surg Int. https://doi.org/10.1007/s00383-022-05097-z
Chan KWE, Lee KH, Wong HYV, Tsui SYB, Mou JWC, Tam YHP (2018) Ten-year native liver survival rate after laparoscopic and open Kasai portoenterostomy for biliary atresia. J Laparoendosc Adv Surg Tech A. https://doi.org/10.1089/lap.2018.0350
Siddiqui AI, Ahmad T (2022) Biliary atresia. StatPearls Publishing, Treasure Island, FL
Ueno T, Kodama T, Noguchi Y, Nomura M, Saka R, Takama Y, Tazuke Y, Bessho K, Okuyama H (2021) Effect of microscopy-assisted portoenterostomy (MAPE) for biliary atresia. Pediatr Surg Int. https://doi.org/10.1007/s00383-020-04794-x
Davenport M, Grieve A (2012) Maximizing Kasai portoenterostomy in the treatment of biliary atresia: medical and surgical options. S Afr Med J. https://doi.org/10.7196/samj.6120
Toyosaka A, Okamoto E, Okasora T, Nose K, Tomimoto Y, Seki Y (1994) Extensive dissection at the porta hepatis for biliary atresia. J Pediatr Surg. https://doi.org/10.1016/0022-3468(94)90011-6
Kobayashi H, Yamataka A, Urao M, Okazaki T, Yanai T, Koga H, Lane GJ, Miyano T (2006) Innovative modification of the hepatic portoenterostomy. Our experience of treating biliary atresia. J Pediatr Surg. https://doi.org/10.1016/j.jpedsurg.2005.12.056
Bax N, Georgeson K (2007) Biliary atresia panel session. In: presentation at the 16th annual congress of the International Pediatric Endosurgery Group (IPEG). Buenos Aires. 2007: 6–9
Ure BM, Kuebler JF, Schukfeh N, Engelmann C, Dingemann J, Petersen C (2011) Survival with the native liver after laparoscopic versus conventional Kasai portoenterostomy in infants with biliary atresia: a prospective trial. Ann Surg. https://doi.org/10.1097/SLA.0b013e318211d7d8
Wada M, Nakamura H, Koga H, Miyano G, Lane GJ, Okazaki T, Urao M, Murakami H, Kasahara M, Sakamoto S, Ishizaki Y, Kawasaki S, Yamataka A (2014) Experience of treating biliary atresia with three types of portoenterostomy at a single institution: Extended, modified Kasai, and laparoscopic modified Kasai. Pediatr Surg Int. https://doi.org/10.1007/s00383-014-3551-5
Ji Y, Yang K, Zhang X, Chen S, Xu Z (2018) Learning curve of laparoscopic Kasai portoenterostomy for biliary atresia: report of 100 cases. BMC Surg. https://doi.org/10.1186/s12893-018-0443-y
Li Z, Ye Y, Wu Z, Wang B (2017) Learning curve analysis of laparoscopic Kasai portoenterostomy. J Laparoendosc Adv Surg Tech A. https://doi.org/10.1089/lap.2016.0204
Wang S, Hu X, Wang J (2022) Learning curve of laparoscopic Kasai portoenterostomy in a tertiary hospital with low caseload of biliary atresia. J Laparoendosc Adv Surg Tech A. https://doi.org/10.1089/lap.2021.0653
Cazares J, Koga H, Murakami H, Nakamura H, Lane G, Yamataka A (2017) Laparoscopic portoenterostomy for biliary atresia: single-center experience and review of literatures. Pediatr Surg Int. https://doi.org/10.1007/s00383-017-4171-7
Yamataka A (2013) Laparoscopic Kasai portoenterostomy for biliary atresia. J Hepatobiliary Pancreat Sci. https://doi.org/10.1007/s00534-013-0607-1
Li B, Chen WB, Huang X, Xia SL, Zhang FN, Wang SQ, Wang YB (2019) Modifications to expose porta hepatis for laparoscopic portoenterostomy easier in biliary atresia. J Surg Res. https://doi.org/10.1016/j.jss.2018.08.013
Huang SY, Yeh CM, Chen HC, Chou CM (2018) Reconsideration of laparoscopic Kasai operation for biliary atresia. J Laparoendosc Adv Surg Tech A. https://doi.org/10.1089/lap.2017.0535
Rong LY, Li YB, Tang JF, Cao GQ, Wan L, Li XY, Zhang X, Chi SQ, Tang ST (2022) Robotic-assisted choledochal cyst excision with Roux-en-Y hepaticojejunostomy in children: does age matter? Surg Endosc. https://doi.org/10.1007/s00464-022-09496-0
Tang ST, Ruan QL, Cao ZQ, Mao YZ, Wang Y, Li SW (2005) Diagnosis and treatment of biliary atresia: a retrospective study. Hepatobiliary Pancreat Dis Int 4:108–112
Song Z, Dong R, Shen Z, Chen G, Yang YF, Zheng S (2017) Surgical outcome and etiologic heterogeneity of infants with biliary atresia who received Kasai operation less than 60 days after birth: a retrospective study. Medicine. https://doi.org/10.1097/MD.0000000000007267
Schreiber RA, Barker CC, Roberts EA, Martin SR, Alvarez F, Smith L, Butzner JD, Wrobel I, Mack D, Moroz S, Rashid M, Persad R, Levesque D, Brill H, Bruce G, Critch J, Res CPH, G, (2007) Biliary atresia: the Canadian experience. J Pediatr. https://doi.org/10.1016/j.jpeds.2007.05.051
Lertudomphonwanit C, Mourya R, Fei L, Zhang Y, Gutta S, Yang L, Bove KE, Shivakumar P, Bezerra JA (2017) Large-scale proteomics identifies MMP-7 as a sentinel of epithelial injury and of biliary atresia. Sci Transl Med. https://doi.org/10.1126/scitranslmed.aan8462
Chi S, Xu P, Yu P, Cao G, Wang H, Ye Y, Li S, Zhou Y, Li X, Zhou Y, Zhang X, Niu H, Xu L, Cai P, Tang S (2022) Dynamic analysis of serum MMP-7 and its relationship with disease progression in biliary atresia: a multicenter prospective study. Hepatol Int. https://doi.org/10.1007/s12072-022-10322-x
Meinzer A, Alkatout I, Krebs TF, Baastrup J, Reischig K, Meiksans R, Bergholz R (2020) Advances and trends in pediatric minimally invasive surgery. J Clin Med. https://doi.org/10.3390/jcm9123999
Acknowledgements
We would like to acknowledge Professor Patrick Chung for writing assistance.
Funding
National Natural Science Foundation of China (Grant Numbers 81873848 and 82071689).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Mengxin Zhang, Guo-qing Cao, Xiangyang Li, Xi Zhang, Yibo Li, Shuiqing Chi, Liying Rong, Shao-Tao Tang have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, M., Cao, G., Li, X. et al. Robotic-assisted Kasai portoenterostomy for biliary atresia. Surg Endosc 37, 3540–3547 (2023). https://doi.org/10.1007/s00464-022-09855-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09855-x