Abstract
Purpose
To investigate the clinical characteristics of cystic biliary atresia (CBA) and evaluate the midterm follow-up outcomes after laparoscopic treatment.
Methods
We analyzed and compared data retrospectively on CBA patients (group A) and nonsyndromic type III biliary atresia (BA) patients (group B), who underwent laparoscopic Kasai portoenterostomy (LKPE) during the same period.
Results
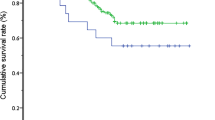
There were no significant differences in operative time, conversion rate, or the incidence of any postoperative complications between groups A and B (P > 0.05). The mean age at surgery (P < 0.01), rates of clearance of jaundice (CJ), cholangitis (P < 0.05), and 5-year survival with a native liver (SNL) were significantly lower in group A than in group B. Among the 35 patients with CBA, the CJ and 5-year SNL rates were significantly better in those with type I (n = 27) than in those with type IIId (n = 8) (P < 0.05).
Conclusions
LKPE is a feasible and safe procedure for CBA. The 5-year SNL after LKPE was better in patients with CBA than in those with nonsyndromic type III BA. The 5-year SNL after LKPE for type I CBA was better than that for type IIId CBA.



Similar content being viewed by others
References
Komuro H, Makino SI, Momoya T, Nishi A. Biliary atresia with extrahepatic biliary cysts–cholangiographic patterns influencing the prognosis. J Pediatr Surg. 2000;35(12):1771–4.
Li Y, Xiang B, Wu Y, Wang C, Wang Q, Zhao Y, et al. Medium-term outcome of laparoscopic Kasai portoenterostomy for biliary atresia with 49 cases. J Pediatr Gastroenterol Nutr. 2018;66(6):857–60.
Lobeck IN, Sheridan R, Lovell M, Dupree P, Tiao GM, Bove KE. Cystic biliary atresia and choledochal cysts are distinct histopathologic entities. Am J Surg Pathol. 2017;41(3):354–64.
Lal R, Prasad DK, Krishna P, Sikora SS, Poddar U, Yachha SK, et al. Biliary atresia with a “cyst at porta”: management and outcome as per the cholangiographic anatomy. Pediatr Surg Int. 2007;23(8):773–8.
Lilly JR, Hall RJ, Vasquez-Estevez J, Karrer F, Shikes RH. The surgery of “correctable” biliary atresia. J Pediatr Surg. 1987;22(6):522–5.
Arima E, Fonkalsrud EW, Neerhout RC. Experience in the management of surgically correctable biliary atresia. Surgery. 1974;75(2):228–32.
Nio M. Japanese biliary atresia registry. Pediatr Surg Int. 2017;33(12):1319–25.
Nio M, Wada M, Sasaki H, Tanaka H. Does hepatic hilum morphology influence long-term prognosis in type I/I cyst biliary atresia? Pediatr Surg Int. 2015;31(10):931–6.
Redkar R, Davenport M, Howard ER. Antenatal diagnosis of congenital anomalies of the biliary tract. J Pediatr Surg. 1998;33(5):700–4.
Hasegawa T, Sasaki T, Kimura T, Sawai T, Nose K, Kamata S, et al. Prenatal ultrasonographic appearance of type IIId (uncorrectable type with cystic dilatation) biliary atresia. Pediatr Surg Int. 2002;18(5–6):425–8.
Davenport M, Ville De, de Goyet J, Stringer MD, Mieli-Vergani G, Kelly DA, McClean P, et al. Seamless management of biliary atresia in England and Wales (1999–2002). Lancet. 2004;363(9418):1354–7.
Davenport M, Betalli P, D’Antiga L, Cheeseman P, Mieli-Vergani G, Howard ER. The spectrum of surgical jaundice in infancy. J Pediatr Surg. 2003;38(10):1471–9.
Caponcelli E, Knisely AS, Davenport M. Cystic biliary atresia: an etiologic and prognostic subgroup. J Pediatr Surg. 2008;43(9):1619–24.
Davenport M, Caponcelli E, Livesey E, Hadzic N, Howard E. Surgical outcome in biliary atresia: etiology affects the influence of age at surgery. Ann Surg. 2008;247(4):694–8.
Mackenzie TC, Howell LJ, Flake AW, Adzick NS. The management of prenatally diagnosed choledochal cysts. J Pediatr Surg. 2001;36(8):1241–3.
Tanaka N, Ueno T, Takama Y, Fukuzawa M. Diagnosis and management of biliary cystic malformations in neonates. J Pediatr Surg. 2010;45(11):2119–23.
Huang FC, Hwang KP. Differential diagnosis of infantile choledochal cyst with or without biliary atresia. Acta Paediatr Taiwan. 2006;47(4):175–80.
Obaidah A, Dhende NP, Mane SB, Acharya H. Biliary atresia associated with choledochal cyst. Afr J Paediatr Surg. 2009;6(1):61–2.
Nio M, Sano N, Ishii T, Sasaki H, Hayashi Y, Ohi R. Long-term outcome in type I biliary atresia. J Pediatr Surg. 2006;41(12):1973–5.
Takahashi Y, Matsuura T, Saeki I, Zaizen Y, Taguchi T. Excellent long-term outcome of hepaticojejunostomy for biliary atresia with a hilar cyst. J Pediatr Surg. 2009;44(12):2312–5.
Ji Y, Yang K, Zhang X, Chen S, Xu Z. Learning curve of laparoscopic Kasai portoenterostomy for biliary atresia: report of 100 cases. BMC Surg. 2018;18(1):107.
Wong KK, Chung PH, Chan KL, Fan ST, Tam PK. Should open Kasai portoenterostomy be performed for biliary atresia in the era of laparoscopy? Pediatr Surg Int. 2008;24(8):931–3.
Murase N, Hinoki A, Shirota C, Tomita H, Shimojima N, Sasaki H, et al. Multicenter, retrospective, comparative study of laparoscopic and open Kasai portoenterostomy in children with biliary atresia from Japanese high-volume centers. J Hepatobiliary Pancreat Sci. 2019;26(1):43–50.
Shirota C, Murase N, Tanaka Y, Ogura Y, Nakatochi M, Kamei H, et al. Laparoscopic Kasai portoenterostomy is advantageous over open Kasai portoenterostomy in subsequent liver transplantation. Surg Endosc. 2020;34(8):3375–81.
Li Y, Gan J, Wang C, Xu Z, Zhao Y, Ji Y. Comparison of laparoscopic portoenterostomy and open portoenterostomy for the treatment of biliary atresia. Surg Endosc. 2019;33(10):3143–52.
Masumoto K, Kai H, Oka Y, Otake R, Yoshizato T, Miyamoto S, et al. A case of cystic biliary atresia with an antenatally detected cyst: the possibility of changing from a correctable type with a cystic lesion (I cyst) to an uncorrectable one (IIId). Pediatr Surg Int. 2011;27(1):99–102.
Faure A, Hery G, Colavolpe N, Bevilacqua C, Guys JM, De Lagausie P. Laparoscopic cystojejunostomy for type I cystic biliary atresia in children. J Minim Access Surg. 2015;11(4):263–6.
Acknowledgements
This work was supported by grants from the National Natural Science Foundation of China (Grant No: 81401606 and 81400862), the Key Project in the Science & Technology Program of Sichuan Province (Grant No: 2019YFS0322), the Science Foundation for Excellent Youth Scholars of Sichuan University (Grant No: 2015SCU04A15), and the 1·3·5 Project for Disciplines of Excellence–Clinical Research Incubation Project, West China Hospital of Sichuan University (Grant No: 2019HXFH056 and 2020HXFH048).
Author information
Authors and Affiliations
Contributions
YJ, JYZ, XPZ, SYC, and ZCX were involved in the clinical management of the patients and collected clinical details for this study. JYZ reviewed the literature and drafted the manuscript. YJ reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
We have no conflicts of interest to declare in association with the present study.
Ethical approval and consent to participate
The Ethics Committee of the West China Hospital of Sichuan University approved the study. Written informed consent was obtained from the patients’ parents according to the provisions of the Declaration of Helsinki.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ji, Y., Zhou, J., Zhang, X. et al. Laparoscopic Kasai portoenterostomy for cystic biliary atresia: midterm follow-up results of 35 patients. Surg Today 51, 1924–1931 (2021). https://doi.org/10.1007/s00595-021-02297-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-021-02297-3