Abstract
Background
Previous studies analyzing short-term outcomes for per-oral endoscopic myotomy (POEM) have shown excellent clinical response rates and shorter operative times compared to laparoscopic Heller myotomy (LHM). Despite this, many payors have been slow to recognize POEM as a valid treatment option. Furthermore, comparative studies analyzing long-term outcomes are limited. This study compares perioperative and long-term outcomes, cost-effectiveness, and reimbursement for POEM and LHM at a single institution.
Methods
Adult patients who underwent POEM or LHM between 2014 and 2021 and had complete preoperative data with at least one complete follow up, were retrospectively analyzed. Demographic data, success rate, operative time, myotomy length, length of stay, pre- and postoperative symptom scores, anti-reflux medication use, cost and reimbursement were compared.
Results
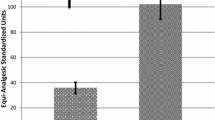
58 patients met inclusion with 25 undergoing LHM and 33 undergoing POEM. There were no significant differences in preoperative characteristics. Treatment success (Eckardt ≤ 3) for POEM and LHM was achieved by 88% and 76% of patients, respectively (p = 0.302). POEM patients had a shorter median operative time (106 min. vs. 145 min., p = 0.003) and longer median myotomy length (11 cm vs. 8 cm, p < 0.001). All LHM patients had a length of stay (LOS) ≥ 1 day vs. 51.5% for POEM patients (p < 0.001). Both groups showed improvements in dysphagia, heartburn, regurgitation, Eckardt score, GERD HRQL, RSI, and anti-reflux medication use. The improvement in dysphagia score was greater in patients undergoing POEM (2.30 vs 1.12, p = 0.003). Median hospital reimbursement was dramatically less for POEM ($3,658 vs. $14,152, p = 0.002), despite median hospital costs being significantly lower compared to LHM ($2,420 vs. $3,132, p = 0.029).
Results
POEM is associated with a shorter operative time and LOS, longer myotomy length, and greater resolution of dysphagia compared to LHM. POEM costs are significantly less than LHM but is poorly reimbursed.
Graphical abstract







Similar content being viewed by others
References
Guidelines for the Use of Peroral Endoscopic Myotomy (POEM) for the Treatment of Achalasia [Internet]. SAGES. 2020 [cited 2022 Mar 6]. Available from: https://www.sages.org/publications/guidelines/guidelines-for-the-use-of-peroral-endoscopic-myotomy-poem-for-the-treatment-of-achalasia/
Wong I, Law S (2017) Peroral endoscopic myotomy (POEM) for treating esophageal motility disorders. Ann Transl Med 5(8):192. https://doi.org/10.21037/atm.2017.04.36
Filicori F, Dunst CM, Sharata A, Abdelmoaty WF, Zihni AM, Reavis KM et al (2019) Long-term outcomes following POEM for non-achalasia motility disorders of the esophagus. Surg Endosc 33(5):1632–1639. https://doi.org/10.1007/s00464-018-6438-z
Shea GE, Johnson MK, Venkatesh M, Jolles SA, Prout TM, Shada AL et al (2020) Long-term dysphagia resolution following POEM versus Heller myotomy for achalasia patients. Surg Endosc 34(4):1704–1711. https://doi.org/10.1007/s00464-019-06948-y
Werner YB, Hakanson B, Martinek J, Repici A, von Rahden BHA, Bredenoord AJ et al (2019) Endoscopic or surgical myotomy in patients with idiopathic achalasia. N Engl J Med 381(23):2219–2229. https://doi.org/10.1056/NEJMoa1905380
Chuah SK, Wu KL, Hu TH, Tai WC, Changchien CS (2010) Endoscope-guided pneumatic dilation for treatment of esophageal achalasia. World J Gastroenterol 16(4):411–417. https://doi.org/10.3748/wjg.v16.i4.411
Nau P, Rattner D (2014) Laparoscopic Heller myotomy as the gold standard for treatment of achalasia. J Gastrointest Surg 18(12):2201–2207. https://doi.org/10.1007/s11605-014-2655-5
Boeckxstaens GE, Annese V, des Varannes SB, Chaussade S, Costantini M, Cuttitta A, et al (2011) Pneumatic dilation versus laparoscopic Heller’s myotomy for idiopathic achalasia. N Engl J Med 364(19):1807–1816. https://doi.org/10.1056/NEJMoa1010502
Is Per-oral Endoscopic Myotomy (POEM) More Effective than Pneumatic Dilation and Heller myotomy? A Systematic Review and Meta-Analysis . SAGES. 2020 [cited 2022 Mar 6]. https://www.sages.org/publications/guidelines/is-per-oral-endoscopic-myotomy-poem-more-effective-than-pneumatic-dilation-and-heller-myotomy-a-systematic-review-and-meta-analysis/
Runge TM, Ichkhanian Y, Khashab MA (2020) POEM for achalasia: endoscopic myotomy enters its golden age, and we are taking NOTES. Gastrointest Endosc 91(5):1045–9.e1. https://doi.org/10.1016/j.gie.2020.01.008
Costantini M, Salvador R, Costantini A (2021) Spastic motility disorders: diagnosis and management in the era of the chicago classification. Foregut 1(3):254–262. https://doi.org/10.1177/26345161211044971
Kumagai K, Tsai JA, Thorell A, Lundell L, Håkanson B (2015) Per-oral endoscopic myotomy for achalasia are results comparable to laparoscopic Heller myotomy. Scand J Gastroenterol 50(5):505–512. https://doi.org/10.3109/00365521.2014.934915
Cappell MS, Stavropoulos SN, Friedel D (2020) Updated systematic review of achalasia, with a focus on poem therapy. Dig Dis Sci 65(1):38–65. https://doi.org/10.1007/s10620-019-05784-3
Greenleaf EK, Winder JS, Hollenbeak CS, Haluck RS, Mathew A, Pauli EM (2018) Cost-effectiveness of per oral endoscopic myotomy relative to laparoscopic Heller myotomy for the treatment of achalasia. Surg Endosc 32(1):39–45. https://doi.org/10.1007/s00464-017-5629-3
Conte TM, de Haddad LB, P, Ribeiro IB, de Moura ETH, DʼAlbuquerque LAC, de Moura EGH. (2020) Peroral endoscopic myotomy (POEM) is more cost-effective than laparoscopic Heller myotomy in the short term for achalasia economic evaluation from a randomized controlled trial. Endosc Int Open 8(11):E1673–E1680. https://doi.org/10.1055/a-1261-3417
Pasricha PJ, Hawari R, Ahmed I, Chen J, Cotton PB, Hawes RH et al (2007) Submucosal endoscopic esophageal myotomy a novel experimental approach for the treatment of achalasia. Endoscopy 39(9):761–764. https://doi.org/10.1055/s-2007-966764
Inoue H, Minami H, Kobayashi Y, Sato Y, Kaga M, Suzuki M et al (2010) Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy 42(4):265–271. https://doi.org/10.1055/s-0029-1244080
Rieder E, Swanström LL, Perretta S, Lenglinger J, Riegler M, Dunst CM (2013) Intraoperative assessment of esophagogastric junction distensibility during per oral endoscopic myotomy (POEM) for esophageal motility disorders. Surg Endosc 27(2):400–405. https://doi.org/10.1007/s00464-012-2484-0
R Core Team (2021) R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. https://www.R-project.org/
Ortega JA, Madureri V, Perez L (1980) Endoscopic myotomy in the treatment of achalasia. Gastrointest Endosc 26(1):8–10. https://doi.org/10.1016/s0016-5107(80)73249-2
Crosthwaite GL, Sejka M (2020) Per-oral endoscopic myotomy (POEM) overview and experience of 100 cases by a single surgeon in Australia. Ann Esophagus 3:12–12. https://doi.org/10.21037/aoe.2020.03.01
Kohn GP (2018) Is peroral endoscopic myotomy (POEM) ready to replace laparoscopic Heller’s myotomy for achalasia comments on a recent systematic review. Ann Laparosc Endosc Surg 3:8–8. https://doi.org/10.21037/ales.2018.01.03
Kim JY, Min YW (2020) Peroral Endoscopic Myotomy for Esophageal Motility Disorders. Clin Endosc 53(6):638–645. https://doi.org/10.5946/ce.2020.223
Cloutier Z, Mann A, Doumouras AG, Hong D (2021) Same-day discharge is safe and feasible following POEM surgery for esophageal motility disorders. Surg Endosc 35(7):3398–3404. https://doi.org/10.1007/s00464-020-07781-4
Ramirez M, Zubieta C, Ciotola F, Amenabar A, Badaloni A, Nachman F et al (2018) Per oral endoscopic myotomy vs. laparoscopic Heller myotomy, does gastric extension length matter. Surg Endosc 32(1):282–288. https://doi.org/10.1007/s00464-017-5675-x
Kane ED, Budhraja V, Desilets DJ, Romanelli JR (2019) Myotomy length informed by high-resolution esophageal manometry (HREM) results in improved per-oral endoscopic myotomy (POEM) outcomes for type III achalasia. Surg Endosc 33(3):886–894. https://doi.org/10.1007/s00464-018-6356-0
Nabi Z, Ramchandani M, Sayyed M, Chavan R, Darisetty S, Goud R et al (2021) Comparison of short versus long esophageal myotomy in cases with idiopathic achalasia: a randomized controlled trial. J Neurogastroenterol Motil 27(1):63–70. https://doi.org/10.5056/jnm20022
Vackova Z, Mares J, Krajciova J, Rabekova Z, Zdrhova L, Loudova P et al (2021) Esophageal motility patterns after peroral endoscopic myotomy in patients with achalasia. J Neurogastroenterol Motil 27(2):205–214. https://doi.org/10.5056/jnm20126
Verlaan T, Rohof WO, Bredenoord AJ, Eberl S, Rösch T, Fockens P (2013) Effect of peroral endoscopic myotomy on esophagogastric junction physiology in patients with achalasia. Gastrointest Endosc 78(1):39–44. https://doi.org/10.1016/j.gie.2013.01.006
Wang XH, Tan YY, Zhu HY, Li CJ, Liu DL (2016) Full-thickness myotomy is associated with higher rate of postoperative gastroesophageal reflux disease. World J Gastroenterol 22(42):9419–9426. https://doi.org/10.3748/wjg.v22.i42.9419
Kumbhari V, Familiari P, Bjerregaard NC, Pioche M, Jones E, Ko WJ et al (2017) Gastroesophageal reflux after peroral endoscopic myotomy: a multicenter case-control study. Endoscopy 49(7):634–642. https://doi.org/10.1055/s-0043-105485
Lu B, Li M, Hu Y, Xu Y, Zhang S, Cai LJ (2015) Effect of peroral esophageal myotomy for achalasia treatment: a Chinese study. World J Gastroenterol 21(18):5622–5629. https://doi.org/10.3748/wjg.v21.i18.5622
Jones EL, Meara MP, Schwartz JS, Hazey JW, Perry KA (2016) Gastroesophageal reflux symptoms do not correlate with objective pH testing after peroral endoscopic myotomy. Surg Endosc 30(3):947–952. https://doi.org/10.1007/s00464-015-4321-8
Laurino-Neto RM, Herbella F, Schlottmann F, Patti M (2018) Evaluationofesophageal Achalasia: from symptoms to the chicago classification. Arq Bras Cir Dig. https://doi.org/10.1590/0102-672020180001e1376
Jung DH, Is PH (2017) Gastroesophageal reflux disease and achalasia coincident or not? J Neurogastroenterol Motil 23(1):5–8. https://doi.org/10.5056/jnm16121
Attaar M, Su B, Wong HJ, Kuchta K, Denham W, Linn JG et al (2021) Comparing cost and outcomes between peroral endoscopic myotomy and laparoscopic Heller myotomy. Am J Surg 222(1):208–213. https://doi.org/10.1016/j.amjsurg.2020.10.037
Khashab MA, Kumbhari V, Tieu AH, El Zein MH, Ismail A, Ngamruengphong S et al (2017) Peroral endoscopic myotomy achieves similar clinical response but incurs lesser charges compared to robotic heller myotomy. Saudi J Gastroenterol 23(2):91–96. https://doi.org/10.4103/1319-3767.203360
Wirsching A, Boshier PR, Klevebro F, Kaplan SJ, Seesing MF, El-Moslimany R et al (2019) Comparison of costs and short-term clinical outcomes of per-oral endoscopic myotomy and laparoscopic Heller myotomy. Am J Surg 218(4):706–711. https://doi.org/10.1016/j.amjsurg.2019.07.026
Lois AW, Oelschlager BK, Wright AS, Templeton AW, Flum DR, Farjah F (2022) Use and safety of per-oral endoscopic myotomy for achalasia in the US. JAMA Surg 157(6):490–497. https://doi.org/10.1001/jamasurg.2022.0807
Kohn GP, Dirks RC, Ansari MT, Clay J, Dunst CM, Lundell L et al (2021) SAGES guidelines for the use of peroral endoscopic myotomy (POEM) for the treatment of achalasia. Surg Endosc 35(5):1931–1948. https://doi.org/10.1007/s00464-020-08282-0
Khashab MA, Vela MF, Thosani N, Agrawal D, Buxbaum JL, Abbas Fehmi SM et al (2020) ASGE guideline on the management of achalasia. Gastrointest Endosc 91(2):213–27.e6. https://doi.org/10.1016/j.gie.2019.04.231
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Lena Shally, Katie Frank, and Drs. Kashif Saeed, Derek Berglund, Mark Dudash, Vladan N Obradovic, David M Parker, Anthony T Petrick, David L Diehl and Jon D Gabrielsen have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplemental Figure 1. POEM operative times since the procedure was first performed in June 2015 (n = 72). Pearson’s correlation coefficient r and associated p-value given in top right corner. Observed values (black points) are overlaid on top of the line of best fit (blue) and its estimated 95% confidence interval (shaded gray band).

Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shally, L., Saeed, K., Berglund, D. et al. Clinical and financial outcomes of per-oral endoscopic myotomy compared to laparoscopic heller myotomy for treatment of achalasia. Surg Endosc 37, 5526–5537 (2023). https://doi.org/10.1007/s00464-022-09652-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09652-6